Biomechanical evaluation different fixation methods for three types of pelvic ring fractures
Background
Pelvic ring fractures occur with an incidence of 0.3 to 8% and have a bimodal distribution affecting young and active or elderly fragile patients. Different classification systems have been developed for a better understanding of a specific pelvic ring fracture, e.g., fractures of fragile bone without an adequate injury mechanism are classified using the Fragility Fractures of the Pelvis (FFP) classification system. There are several minimal invasive stabilization techniques and strategies available, but the biomechanical efficiency of these fixations for various fracture types has not yet been fully understood.
Goal
To examine biomechanically different fixation methods for (1) AO C1-3/FFP IIIc unstable pelvic fractures, (2) AO 61 B3.3/Young-Burgess LC III bilateral superior and inferior pubic ramus (Butterfly) fractures, and (3) AO 61 C1.3/FFP IIb non-displaced sacral crush fractures in artificial pelvic bone models.
Results
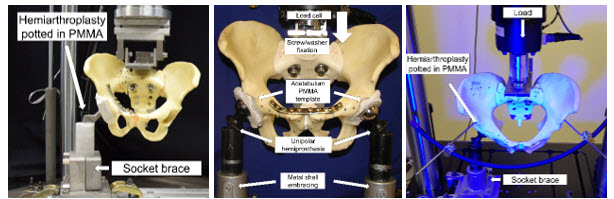
Cyclic loading to failure was performed on instrumented artificial bone models using either a hemi-pelvic one-leg-stance or a two-leg stance model to evaluate and compare the biomechanical competence of various fixation techniques. Interfragmentary motions were continuously measured throughout the test cycles by means of optical motion tracking. The results of three sub-studies highlighted the best fixations strategies for the different fracture types, as follows. First, in FFP IIIc fractures using an SI screw together with anterior plate or creeping screw provided the highest stability. If an FFP IIIc fracture is present, both the anterior and posterior pelvic ring should be addressed. Stabilization of the anterior pelvic ring by means of an external fixator significantly improved the stability compared to an isolated stabilization of the posterior pelvic ring. An S1-S2-Ala-ilium construction was particularly well suited for stabilizing the posterior pelvic ring fracture. Second, for surgical treatment of Butterfly fractures, there was no significant difference between anterior plate osteosynthesis and trans-pubic bilateral screw osteosynthesis regarding axial stiffness, cycles and maximum force to failure and dislocation after 500 cycles. Depending on the clinical picture, either open surgical plate osteosynthesis or the rather minimally invasive use of trans-pubic screws can be used. Third, the use of a Herbert Screw for fixation of the posterior pelvic ring in AO 61 C1.3 fractures was compared to one SI screw, two parallel SI screws or one augmented SI screw. Cement augmentation of the SI screw resulted in significantly more stability. The use of two SI screws, augmented SI screw and the Herbert Screw seemed to be biomechanically superior to the conventional SI screw.
-
Partner
Raschke M (Prof), Münster University Hospital, Münster, Germany