Upper extremity curriculum
Upper extremity education taskforce
The upper extremity education taskforce is a group of experts who build and continously improve our educational program. It consists of three international program editors (IPEs).

Joyce Koh (Singapore)
Term: 2025–2027

George Dyer (USA)
Term 2026–2028

Pedro Labronici (BR)
Term: 2024–2026
Regional Program Contributors (RPCs)
Asia Pacific
Kevin Yik (Singapore)
Lia Marliana (Indonesia)
Europe and Southern Africa
Lars Müller (Germany)
Fernando Marco (Spain)
Middle East and Northern Africa
Raid Abutalib (Saudi Arabia)
Hashem Abdulwahab Issa Al Qdhah (Jordan)
Latin America
Luis Ocha (Mexico)
Caio Zamboni (Brazil)
North America
Andrew Choo (USA)
Jonah Davies (USA)
AO Curriculum Development Manager:
Past taskforce members
-
Past IPEsSami Roukoz (Lebanon), 2023–2025
Odette Koch (South Africa), 2022–2024
Diane Nam (Canada), 2021–2023
Martin Richardson (Australia), 2020–2022
Ashraf Moharram (Egypt), 2017–2021
Stefaan Nijs (Belgium), 2017–2020
Paul Binhammer (Canada), 2017–2019 -
Past RPCsBrian Buck (USA)
George Dyer (USA)
Jae-Woo Cho (South Korea)
Ali Alsuwaidi (UAE)Zinon Kokkalis (Greece)
Andrey Ratyev (Russia)
Christian Lozano (Peru)
Pablo Vargas (Chile)
Zhou Fang (China)
Joyce Koh (Singapore)
George Dyer (USA)
Martin Richardson (Australia)
Michael McKee (USA)
Diane Nam (Canada)
Sami Roukoz (Lebanon)
Ziyad El-Qirem (Jordan)
Jayasankar Perur Viswanathan (India)
Frederick du Plessis (South Africa)
Frédéric Vauclair (Switzerland)
Jorge Boretto (Argentina)
Alejandro Espinosa (Mexico)
Gregory Della Rocca (USA)
Program description

The curriculum provides the framework for teaching the current management of patient pain, dysfunction, deformity, and cosmesis related to trauma of the upper limb. It covers fractures from the sternoclavicular joint to the fingertip as well as joint injuries and dislocations and soft tissue injuries (the acute trauma phase and the posttraumatic sequelae such as malunion, nonunion, infection, etc).
The high level of interactivity is built-in to the module structures in all of the defined educational events. Lectures are used to introduce the challenges related to each anatomical region and to establish common terminology and approaches as well as to summarize the evidence for current management. Most of the content is, however, delivered through small group discussions, where structured cases integrate the learning objectives from the curriculum. The setting at round tables supports the educational format.
Educational events defined in the curriculum:
AO Trauma Course—Upper Extremity Trauma
AO Trauma Course—Shoulder and Elbow Trauma
AO Trauma Course—Shoulder Trauma
AO Trauma Course—Elbow Trauma
Target audience
“Upper Extremity Trauma” and “Shoulder and Elbow Trauma” courses:
Orthopedic and trauma surgeons with at least 3 years of experience who want to develop expertise in upper extremity fracture care or surgeons with many years of experience who want to update their knowledge. Participants should have completed the AO Trauma Course—Advanced Principles of Fracture Management.
“Masters Shoulder Trauma” and “Masters Elbow Trauma” courses:
Orthopedic, trauma, and shoulder surgeons with at least 5 years of experience who want to update their expertise and want to manage complications and more complex cases. Participants should have completed the AOTrauma Course—Advanced Principles of Fracture Management.
Resources for faculty
Already a faculty member? Explore resources supporting your teaching activities.
Resources
Courses and webinars
Explore our database and search for events on specific topics.
AO Surgery Reference
Explore the collection of expert-recommended AO Surgery Reference pages that match the course content.
Competencies
The curriculum is based upon 7 competencies:
- Perform an appropriate assessment of the patient with trauma to the shoulder, humeral shaft, elbow, forearm, wrist, and hand
- Identify the minimal quality requirements for each assessment tool and the optimal way to gather the required information
- Perform a thorough, stepwise analysis of the problem (what is the mechanical, biological, and soft tissue situation and problem)
- Identify the advantages and disadvantages of the treatment options and decide with the patient which is best for their specific needs
- Develop a comprehensive plan based on the needs of the patient, the injury, the patient factors, and the available surgical options
- Complete the plan (perform operative procedures and nonoperative care)
- Provide and communicate overall care, integrating the team, family, and supporting care system
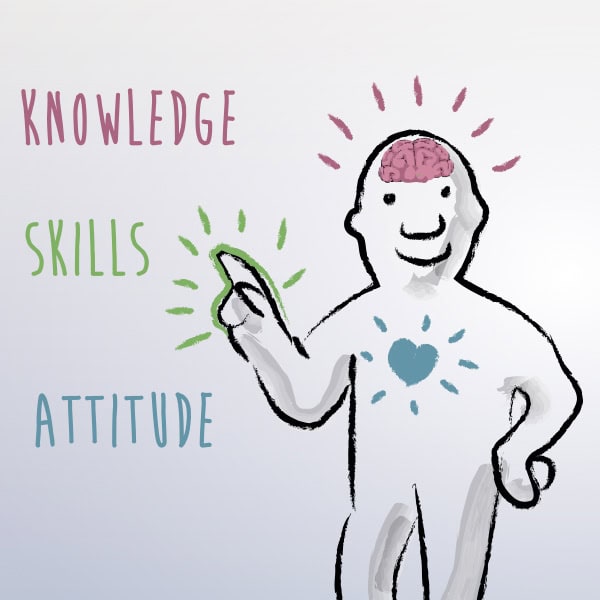
What does competency-based curriculum development mean?
Contacts

To address feedback or questions to this education taskforce, email the Curriculum Development Manager Michael Cunningham.


