Fragility fractures of the pelvis (FFP): an emerging clinical entity
PROF EM DR POL M ROMMENS
Thanks to fighting against poverty, disease prevention and continuing improvement of medical care, we experience a steady increase of life expectancy all over the globe. However, high age relates to morbidities, reduction of mobility and enhanced risk of injuries such as fractures of the hip, vertebral column, or shoulder joint.
Osteoporosis is a widespread disease among elderly persons, especially women. Due to diminution of bone mineral density, there is an elevated threat of suffering an insufficiency or fragility fracture after minimal trauma. In recent decades, we have been confronted with an emerging clinical entity, which was seldom seen and underestimated before. The incidence of fragility fractures of the pelvis (FFP) has increased by 25% between 1996 and 2010 among Medicare beneficiaries in USA [1]. Similar tendencies are registered in Finland, the Netherlands, Germany, Switzerland, and Belgium.
-
Read the quick summary:
-
Recent decades have seen an increase in the incidence of fragility fractures of the pelvis (FFP)
-
These fractures result from low-energy trauma
-
While not acutely life-threatening, an FFP will cause high pain levels and immobility
-
When considering treatment, the profile of FFP patients is different from younger patients who experience fractures resulting from high-energy trauma
-
Different types of FFP call for different interventions which should include minimal-invasive techniques
-
Further research is needed to answer questions about FFP treatment; the author introduces the AO-Fragility Fractures of the Pelvis (AO-FFP) Registry
-
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Understanding the unique nature of Fragility Fractures of the Pelvis (FFP)
Whereas pelvic ring injuries are classically associated with high-energy trauma, we are looking here at a clinical entity with totally different characteristics. FFP are always the result of a low-energy trauma. In a minority of patients, a traumatic event is not recalled. Due to consistent locations of pelvic fragility fractures, the fracture patterns of FFP are different than in high-energy trauma [2]. We observe an implosion of the pelvic ring instead of an explosion.
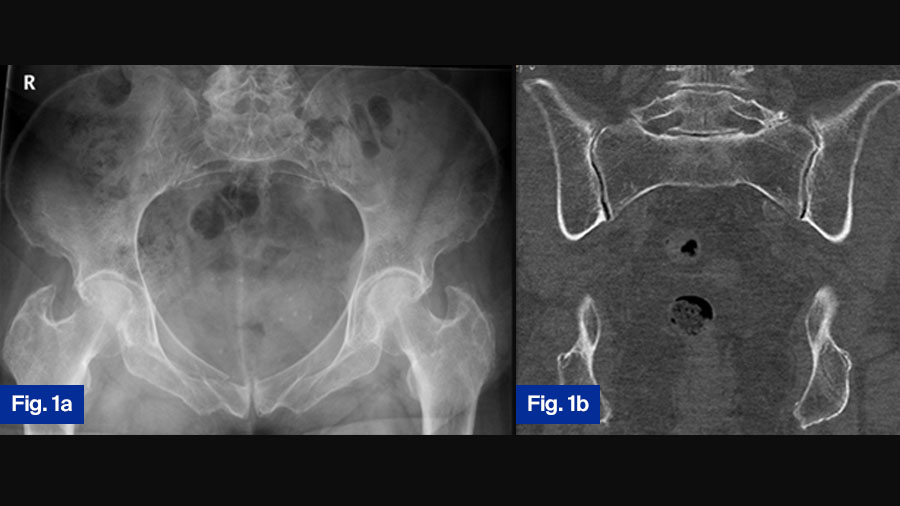
Moreover, new fractures may add to the existing ones. This fracture progression leads to increased instability (Figure 1a-d).
Case study 1: 78-year-old female with progressive fragility fracture
Fig. 1. A seventy-eight-year-old female suffered a domestic fall. The pelvic inlet (a) revealed a slightly displaced fracture of the right pubic ramus. A pelvic CT was taken to exclude fractures of the posterior pelvic ring. On the coronal reconstruction of the posterior pelvis (b), no fracture can be detected. The fracture was classified as FFP Type Ia and conservative treatment initiated.
Due to persisting pain, a second CT was taken one month later. On the coronal reconstruction of the posterior pelvis, a non-displaced fracture of the lateral mass of the sacrum on the left side was now visible (c). Conservative treatment was continued. Because of persistent pain with restricted mobility, a third pelvic CT was taken one month after the second.
The coronal reconstruction of the posterior pelvis revealed an additional fracture of the lateral mass of the sacrum on the right side (d). The fracture progressed from FFP Type Ia to FFP Type IIc.
Symptoms and diagnostic challenges in fragility fractures of the pelvis
The leading symptoms of patients with FFP are intense pain in the pelvic ring and immobility, but there is no acute life-threatening condition. Because of these different properties, the existing frameworks (classifications) are not adequate for evaluation of FFP.
A new, comprehensive classification was elaborated to assess their identity. It is based on the degree of instability (first criterion) and the localization of the fracture (second criterion). Diagnosis is made with conventional x-rays and CT-scan of the pelvis. MRI and dual-energy CT are as sensitive, but less acutely available resources.
FFP Classification: A system for assessing instability and treatment needs
The so-called FFP-classification distinguishes between 4 categories of increasing instability. FFP type I are isolated anterior fractures, FFP type II non-displaced posterior fractures, FFP type III displaced unilateral fractures, and FFP type IV displaced bilateral fractures. The subtypes of the FFP types II, III and IV distinguish between iliac, ilio-sacral and sacral fractures.
- FFP Type I: Isolated anterior fractures (treated conservatively).
- FFP Type II: Non-displaced posterior fractures (may require surgical stabilization).
- FFP Type III: Displaced unilateral fractures (requires surgery).
- FFP Type IV: Displaced bilateral fractures (requires surgery).
In total, there are 11 subtypes: 2 in FFP type I and 3 in FFP type II, III and IV each [3].
Surgical vs. conservative management: controversy in FFP treatment
There is worldwide consensus that high-energy pelvic ring lesions need operative treatment. Open reduction and internal fixation (ORIF) reduces mortality and morbidity, while enhancing functional recovery and quality of life. However, the “personality” of patients, who suffered FFP is totally different from that of younger patients with pelvic ring injuries. All FFP-patients have old age and present with different comorbidities. Due to their frailty, they are at higher risk for invasive therapeutic measures. There is a vigorous debate on what is the best management for FFP patients.
Retrospective studies on larger patient samples with conservatively treated FFP document a much higher one- to five-year-mortality rate than in the reference population, even in patients with isolated pubic rami fractures [4]. On the contrary, FFP-patients, who are treated with ORIF demonstrate high incidences of surgical complications [5].
It can be concluded that surgery must be minimal-invasive, if deemed necessary. Adequate pain management and early mobilization are the pillars of any treatment. Recommendations for surgical treatment are based on the FFP-classification, the clinical condition of the patient at admission and the success of mobilization efforts. FFP type I, which has no posterior fracture, is treated conservatively.
The patients are discharged early or remain ambulatory. FFP type II is the most frequent fracture type. There is no displacement of the posterior fracture, but it may be combined with an anterior fracture. An attempt of conservative treatment consists of pain therapy and mobilization as tolerated with the help of a physiotherapist, walking frame and/or rollator. If there is no progress in mobilization or pain intensity increases within days, a minimal-invasive surgical stabilization is recommended. For FFP type III and IV, surgical stabilization is performed as these are highly unstable lesions.
Minimally invasive surgical techniques for FFP
Different surgical options exist to stabilize the pelvic ring while minimizing risks:
- Posterior Pelvic Stabilization: Ilio-sacral screws, trans-sacral bars, lumbo-pelvic fixation.
- Anterior Pelvic Stabilization: Retrograde transpubic screws, INFIX, pelvic bridges.
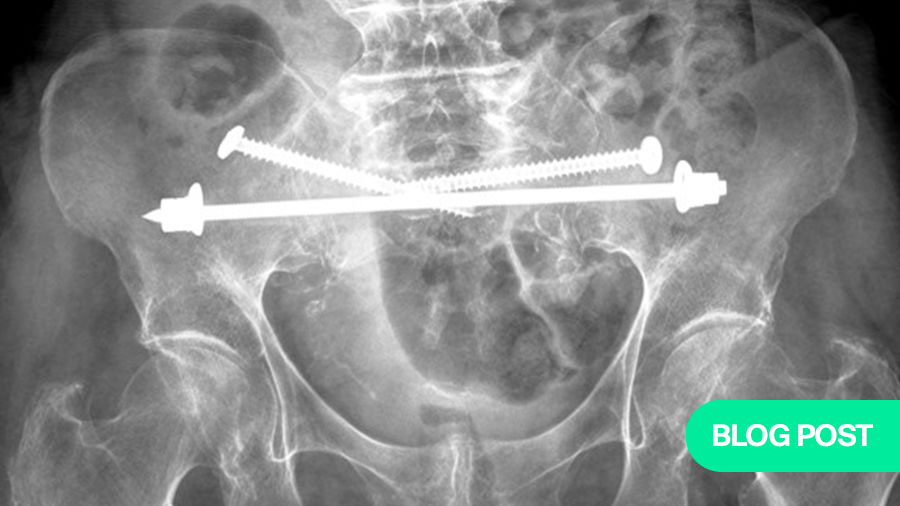
There are different minimal-invasive techniques, which can be used for stabilization of the posterior and anterior pelvic ring. Prerequisite is a thorough preoperative analysis of the specific anatomy of the pelvic ring of each patient, including the measurement of the intra-osseous corridors, through which implants can be inserted. The techniques and implants for the posterior pelvic ring are: ilio-sacral screw osteosynthesis, cement augmentation of ilio-sacral screws, trans-iliac trans-sacral screws, trans-sacral bars (Figure 2a-g), trans-iliac internal fixator, and lumbo-pelvic fixation [6]. Techniques and instruments for the anterior pelvic ring are: retrograde transpubic screw, pelvic bridge, internal fixator (INFIX). Multiple biomechanical studies display the varying stiffness and load-bearing stability of each system.
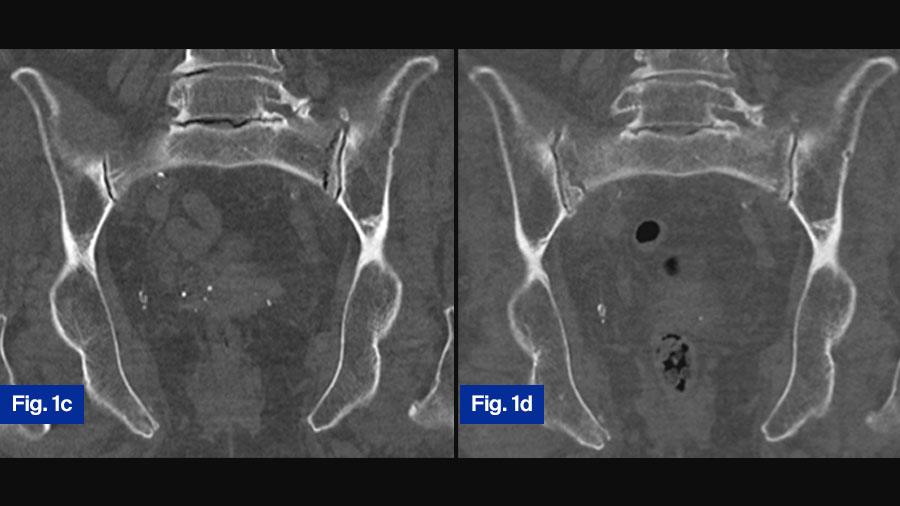
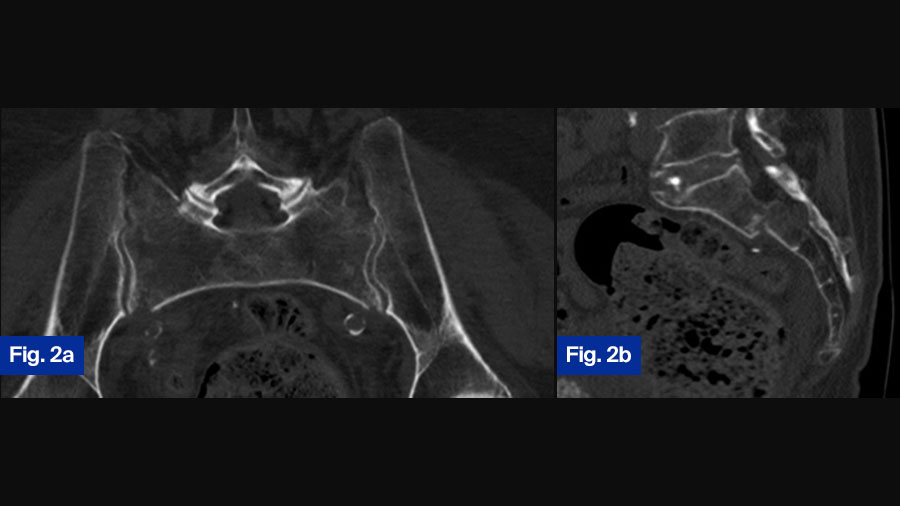
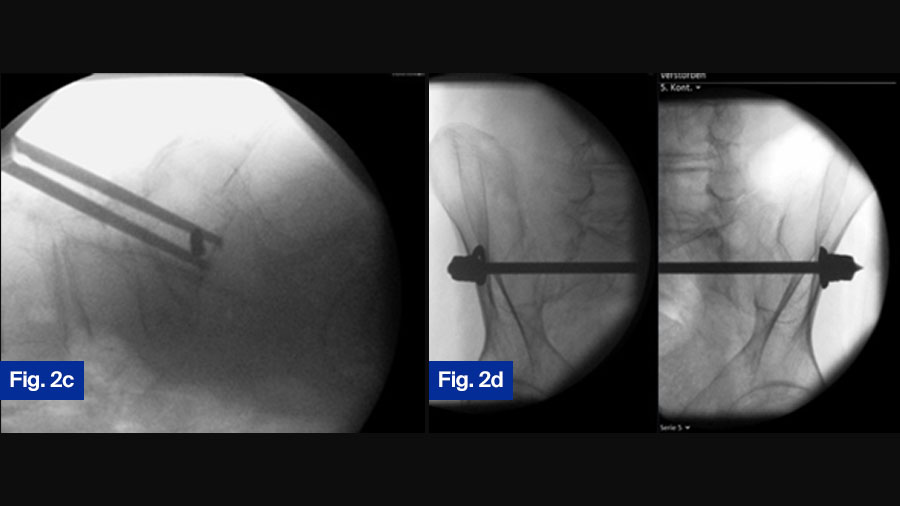
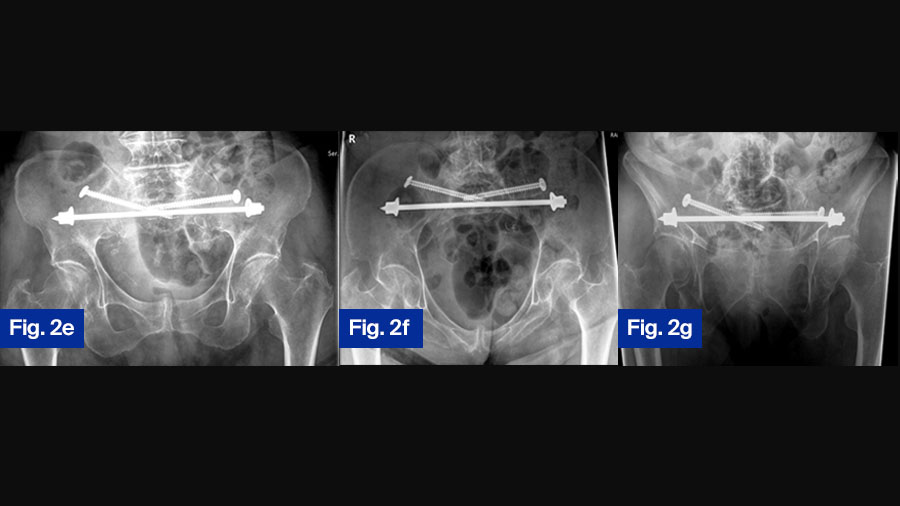
Case Study 2: 92-year-old female with bilateral sacral fracture (FFP Type IVb)
Figure 2. 92-year-old female patient presenting 1 week after fall from standing height with immobilizing pain at lower lumbar spine. (a) Axial CT demonstrating slight displacement of bilateral sacral fracture; (b) sagittal CT with displaced transversal fracture at S1/S2 level. The fracture was classified as FFP type IVb. (c) Lateral fluoroscopic image orientated in direction of the patient (bottom anterior, left cranial) showing overlapping of ilio-cortical densities and ischial notch.
The drill guide is placed centrally in S1 corridor caudal to the ilio-cortical densities. (d) Oblique obturator view to assess the abutment of the washer on the iliac cortex.
Postoperative control at discharge, patient is mobile with a walker ( (e) anterior–posterior, (f) inlet, and (g) outlet view ).
Unanswered questions: the need for further research in FFP treatment
Despite a multitude of publications, there is no consensus on the ideal treatment algorithm of FFP. Many questions remain unsolved: which fractures and which patients profit the most from operative treatment; what is the best time for surgical treatment; is there a need of fixation of the anterior pelvic ring; what is the short- and long-term outcome of surgical treatment for pain intensity, mobility, independency, quality of life and mortality? Retrospective studies only give a partial answer to these questions with a low grade of evidence.
The AO-FFP study: An international research initiative on fragility fractures
There is an urgent need of prospective clinical studies to shed light on these unsolved questions. The AO-Fragility Fractures of the Pelvis (AO-FFP) Registry has been set up to meet this need. It is an international prospective observational study with the aim to investigate outcome of conservative and operative treatment of FFP.
420 patients with FFP type II, FFP type III or FFP type IV will be recruited in a 5-year period in 10 large AO Trauma centers in USA, Canada, Japan, Hong Kong, France, Switzerland, the Netherlands, and Germany. There is no randomization and no recommendation on treatment given by the study protocol. The participating study centers continue to perform the treatment, which is standard in their hospital.
The recruited patients are followed for one year and during this time, patients are reviewed at 6 weeks, 3, 6 and 12 months after the day of treatment decision. Classification of FFP is performed by the centers and controlled through analysis of preoperative X-rays and CT by the principal clinical investigator (PCI). Time to ambulation is noticed in all patients.
In case of operative treatment, the type and localization of treatment (posterior, anterior, both) and pre-operative complications is registered. At discharge and at the above mentioned timepoints, patients are asked about independency (Barthel index), mobility (Parker Mobility Score), pain intensity (NRS) and quality-of-life (EuroQoL-5D). In case of death, precise date and reason of death is noticed.
Study goals and expected impact on FFP treatment guidelines
With this international study, we gather data from patients from different countries and continents, which are subject to variable treatment algorithms. It will be highly interesting how these algorithms influence the above-mentioned parameters. At first, mortality will be compared between the patient collective that was treated conservatively with the collective that was treated operatively. Secondary outcome measures will also be compared and subgroup analysis performed depending on the FFP-classification and type of treatment.
The data of the AO-FFP study will enable us to answer multiple questions with a high level of evidence. A solid and clear treatment algorithm based on these data can be developed, which can become a guideline, supported by many national medical organizations for orthopaedic trauma, geriatrics, and family doctors. The aim is to establish evidence-based treatment guidelines for FFP, influencing decision-making across orthopedics, geriatrics, and family medicine. Standardized protocols could improve survival, mobility, and quality of life for elderly patients.
We are very grateful for the support that the AO Trauma Research Commission gave us in setting up this important study. We are also very grateful for the continuing and professional support of the AO team at AO ITC, which helps to solve many practical problems, manage the database, and especially motivate the participating centers for permanent recruitment and regular patient controls.
***
AO ITC Clinical Evidence team is the AO's clinical research provider with about 30 clinical research specialists in Medical Scientific Affairs and Clinical Operations. Guided by leading surgeons, AO ITC conducts clinical research on highly relevant trauma and orthopedics topics to produce clinical evidence for better patient care.
Find out more about the 45 AO ITC Clinical Evidence studies currently running in 40 countries.
About the author:
References and further reading:
- Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014 Mar;37(3):151-7. doi: 10.3928/01477447-20140225-50. PMID: 24762143.
- Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976). 2009 Feb 15;34(4):309-15.
- Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 2013 Dec;44(12):1733-44. doi: 10.1016/j.injury.2013.06.023. Epub 2013 Jul 18. PMID: 23871193.
- Rommens PM, Hopf JC, Herteleer M, Devlieger B, Hofmann A, Wagner D. Isolated Pubic Ramus Fractures Are Serious Adverse Events for Elderly Persons: An Observational Study on 138 Patients with Fragility Fractures of the Pelvis Type I (FFP Type I). J Clin Med. 2020 Aug 3;9(8):2498. doi: 10.3390/jcm9082498. PMID: 32756494; PMCID: PMC7463797.
- Rommens PM, Hofmann A, Kraemer S, Kisilak M, Boudissa M, Wagner D. Operative treatment of fragility fractures of the pelvis: a critical analysis of 140 patients. Eur J Trauma Emerg Surg. 2022 Aug;48(4):2881-2896. doi: 10.1007/s00068-021-01799-6. Epub 2021 Oct 11. PMID: 34635938; PMCID: PMC9360165.
- Wagner D, Kisilak M, Porcheron G, Krämer S, Mehling I, Hofmann A, Rommens PM. Trans-sacral bar osteosynthesis provides low mortality and high mobility in patients with fragility fractures of the pelvis. Sci Rep. 2021 Jul 9;11(1):14201. doi: 10.1038/s41598-021-93559-0. PMID: 34244526; PMCID: PMC8270908.
You may also be interested in:
AO Trauma Orthogeriatrics Curriculum
Explore the interdisciplinary program related to fragility fractures and orthogeriatrics. AO Trauma Courses cover Fracture Care in Older Adults and Operative Fragility Fracture Management.
AO Surgery Reference
AO Surgery Reference is a resource for the management of fractures, based on current clinical principles, practices and available evidence. Modules include adult and pediatric trauma and periprosthetic fractures.
AO Trauma Orthogeriatrics App
Your go-to app for managing fragility fractures in older adults. The free educational app is designed for healthcare professionals dedicated to optimizing the care of older adults with fragility fractures.
Osteoporotic Fracture Care—Medical and Surgical Management
AO Trauma publications focus on the clinical and educational needs of orthopedic and trauma professionals. Osteoporotic Fracture Care is a well-rounded and comprehensive resource on fragility fractures and orthogeriatric care.