13C3 distal humeral fractures and possible olecranon osteotomy
BY PEDRO LABRONICI AND FABIO SUAREZ
While complex distal humerus fractures (AO type 13C3) account for a rather low percentage of overall fractures, they are surprisingly common for trauma surgeons. Gaining adequate visualization and access to the fracture site often requires an olecranon osteotomy approach. And in some cases, particularly in older patients or those with life-limiting conditions, a total elbow arthroplasty is indicated.
This blog accompanies and summarizes AO Trauma webinar “13C3 Distal Humeral Fractures”, moderated by Fabio Suarez (Universidad Militar Nueva Granada, Bogota, Colombia ) and presented by Pedro Labronici (Universidade Federal Fluminense, Niterói, Brazil). With this presentation, Labronici draws on his extensive personal experience to clarify many points regarding diagnosis, imaging choices, indications for an olecranon osteotomy, plating decisions, and when the best option is a total elbow arthroplasty.
Learning Objectives
- Define the best images for the diagnosis of a 13C3 fracture.
- Indicate when to use the approach with an olecranon osteotomy.
- a. Describe the biomechanical differences between orthogonal and lateral plate constructs.
b. Differentiate between the indications for orthogonal and lateral plate constructs. - Understand when a total elbow arthroplasty is indicated.
A challenging injury
Complex distal humeral fractures are particularly challenging to treat. In younger patients, this type of fracture typically results from a high-energy impact, such as a fall from a ladder or a motor-vehicle accident. As a result, the fracture may be open, but extensive soft tissue damage and additional injuries may delay treatment. Among older patients, particularly those with osteoporosis, the impact necessary to cause this grade of fracture can be comparatively light; however, the incidence of comorbidities is high.
Question 1: Which preoperative images are best for the diagnosis of a 13C3 fracture
In all cases where a complex distal humerus fracture is suspected, proper diagnosis and treatment calls for the most informative imaging available. If you have access to 3D computed tomography (CT), this is one place where it will be very useful. Because of the number of bone fragments involved, a 2-dimensional CT scan can actually add to the confusion. In order to plan the operation, a set of 3D CT scans can show the relative sizes, locations and orientations of all fragments. As noted below, if a 3D CT scanner is not available, an arthrogram or arthroscope will also provide high-quality, useful images at the time of surgery.
Question 2: What are the indications and contraindications for an olecranon osteotomy
Other possible approaches for distal humeral fractures include paratricipital (medial or lateral) or transtricipital. If either of these will allow adequate visualization and access (particularly if plating is planned), no olecranon osteotomy will be necessary. And if a distal humeral prosthesis—but not a full elbow arthroplasty—is planned, the olecranon must be kept intact, as it is necessary to stabilize the prosthesis.
If no 3D CT scanner is available, an arthrogram, or, preferably, an arthroscope will provide a full view of the joint at the time of surgery.
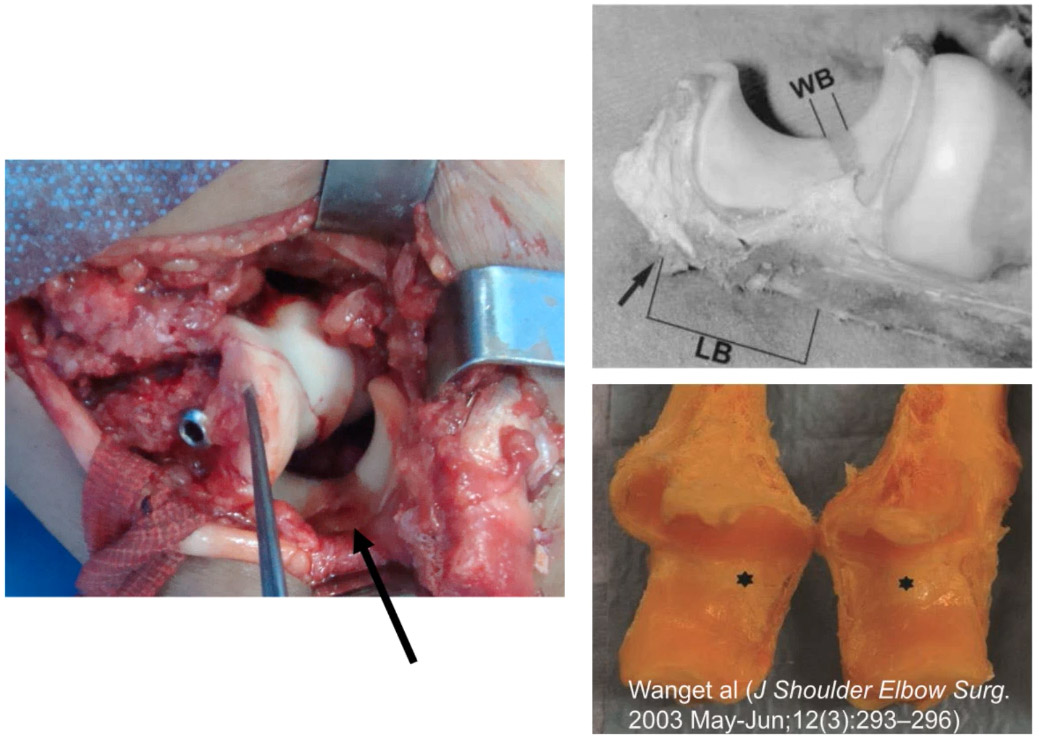
If an osteotomy is necessary—as is usually the case for a 13C3 humeral fracture—then it is necessary to choose the optimal points to begin and end the cut or cuts. As indicated below by the black arrow in the photo on the left, and by the WB in the upper right photo, the least harmful position is the transverse trochlear ridge, i.e., the cartilage-free area strip across the proximal ulna. However, to avoid damaging nearby structures, the cut should not go completely through, i.e., the final millimeter should be broken loose.
Chevron cut pattern reduces the risk of non-union
As for the cut recommended for the osteotomy, the chevron pattern is currently preferred. Although this takes longer to perform, a meta-analysis by Feinstein et al. (2023) showed that, compared to a simple transverse cut, it is significantly less likely to result in non-union.
Elevating the triceps protects it while making room for the surgery
To prepare for the osteotomy, it is necessary to detach the triceps tendon from the shaft of the humerus and keep it elevated. For this purpose, a Cobb elevator can be used to open a channel between the triceps and the humerus. A hemostat can then be used to pull one end of a lab sponge back through. The two ends of this sponge can then be used to pull the triceps back from the humerus and expose the joint. This strategy both keeps the joint clear of obstructions and protects the triceps.
Question 3: Orthogonal or lateral plating: Which offers the greatest biomechanical advantage?
For the reduction of the fracture, it will be necessary to choose between orthogonal or lateral plating. In terms of loss of fixation, complications or other clinical results, there are no significant differences between the two. However, for more distal fractures and those with larger fragments, orthogonal plates are preferable. When dealing with highly comminuted or osteoporotic bone, or short medial and lateral fragments, lateral/ parallel plating offers more biomechanical stability, which is essential.
Case studies illustrating indications for orthogonal versus lateral plating
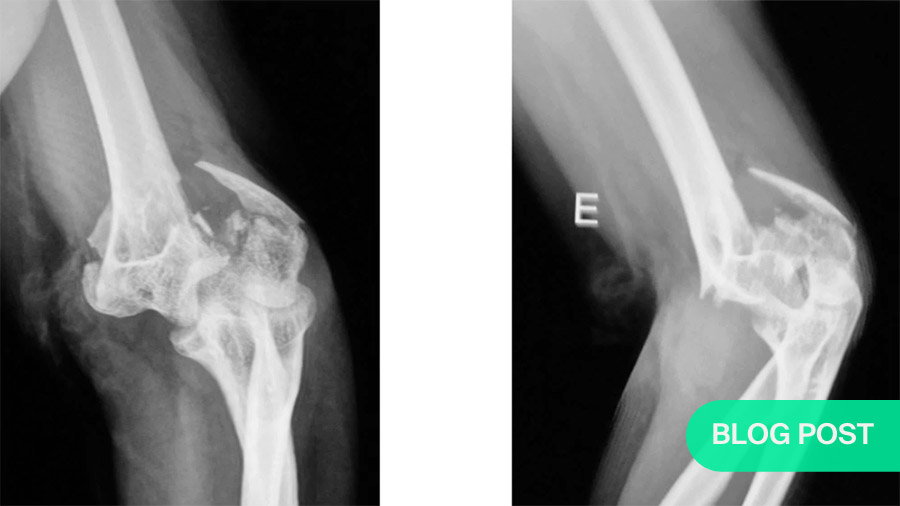
To illustrate indications for orthogonal and lateral plating, Labronici presents two case studies. X-rays and 3D CT images are available for both.
Case study 1 is of an injury sustained by a 30-year-old man in a motor-vehicle accident. Neurovascular status is normal. The diagnostic imaging reveals mainly large fragments, indicating that orthogonal plating will be most useful. As a damage control measure, external fixation is applied to the proximal humerus.
Following an olecranon osteotomy, the fracture is anatomically reduced very accurately using K-wires , after which plating is added.
Two years post-operatively, the subject shows very good extension and flexion.
Case Study 2 shows the result of a ladder fall by a 58-year-old woman with otherwise healthy bone. The degree of comminution is quite severe; therefore, after the olecranon osteotomy, the surgeon opts for parallel plating. To maximize stability, a third plate is added.
Question 4: Understand when a total elbow arthroplasty is indicated.
In some patients, there is no reasonable hope of recovery from an acute distal humeral fracture using reduction. Amjid et al. (2010) specify five groups for whom a total elbow arthroplasty is automatically indicated:
- Non-rheumatoid patients over the age of 75 years;
- Patients with rheumatoid elbow disease (any age);
- Patients with reduced life expectancy (any age);
- Patients with pathological bone (any age);
- Patients with degenerative elbow disease over the age of 60 years
As an illustrative case, Labronici has chosen that of a 66-year-old woman with rheumatoid arthritis. She has suffered a fall with a closed fracture. Her neurovascular status is normal.
As the 3D CT image shows, the fractured elbow has no cartilage. Therefore, a total elbow arthroplasty is performed. Eighteen months post-operatively, the patient shows normal flexion and roughly 35 degrees of extension, with normal rotation of the radius and ulna.
According to Evans et al. (2022), there is a strong chance that this prosthesis will still be functional in ten years’ time. In their study of 1238 total elbow replacements, they found an overall 10-year joint survival rate of over 80%.
Question 5: How should the joint be immobilized postoperatively?
Depending on the details of the surgery and the specific patient characteristics, the surgeon may choose partial immobilization in a sling or full immobilization in a cast. In either case, an angle of 30 degrees extension, i.e., 120 degrees relative to the humerus, is preferable to the previously-favored 90 degree bend.
Labronici comments that not only does greater extension ease the return to normal functionality, it also protects the joint from edema, hematoma and other complications.
Wherever possible, though, the sooner a patient can safely begin functional exercises, the better. These can relieve pain and yield better long-term outcomes regarding flexion and extension.
Take-home messages
- To give your patient the best possible outcome, it is essential to plan the surgery as fully as possible. This will mean
a. using the most informative images available to you:
i. preferably 3D CT scans;
ii. but possibly also an arthrogram or arthroscopy at the time of surgery.
b. choosing the approach that will allow you the best visualization and access to the joint (an olecranon osteotomy may not be necessary); - deciding on whether parallel/transverse or orthogonal plates will offer the necessary containment and stability; and
- enrolling the patient as soon as possible post-operatively in functional therapy.
Other questions, such as whether or how much the ulnar nerve should be transposed, are dealt with in the questions following the presentation.
Watch a video recording of the original AO webinar:
About the authors
Pedro Labronici
Professor of Orthopedics and Traumatology at the Fluminense Federal University, Niteroi, Rio de Janeiro and the Petropolis University (UNIFASE) Petropolis, Rio de Janeiro.
Head of the orthopedics and traumatology service at Santa Tereza Hospital, Petropolis, Rio de Janeiro.
Prof. Fabio A . Suarez R MD
Full professor of the Orthopedic Residency Program
Director of the Hand and upper extremity Fellowship
Universidad Militar nueva granada Hospital Militar Central
Bogota, Colombia
AO Trauma thanks Labronici and Suarez for so generously sharing their time and knowledge on this topic.
References:
- Coles CP, Barei DP, Nork SE, Taitsman LA, Hanel DP, Bradford Henley M. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006 Mar;20(3):164-71. DOI: 10.1097/00005131-200603000-00002. PMID: 16648697.
https://pubmed.ncbi.nlm.nih.gov/16648697/ - Feinstein, Shawn D. et al., Techniques and Fixation of Olecranon Osteotomy: A Systematic Review. Original Research | Volume 5, ISSUE 5, P643-649, September 2023. Open AccessPublished:June 16, 2023 DOI:https://doi.org/10.1016/j.jhsg.2023.04.001
- Amjid Ali, FRCS, Shantanu Shahane, FRCS, David Stanley, MBBS, BSc, FRCS. Total elbow Arthroplasty for distal humeral fractures: Indications, surgical approach, technical tips, and outcome. J Shoulder Elbow Surg. 2010 Mar; 19(2 Suppl):53–58.
- Jonathan P Evans, Jonathan T Evans, Hasan R Mohammad, Adrian Sayers, Ashley W Blom, Michael R Whitehouse, Jonathan L Rees. How long does an elbow replacement last? A systematic review and meta-analysis of case-series and national registry reports with more than 10 years of follow-up. 30 May 2022, Acta Orthopaedica. DOI: 10.2340/17453674.2022.2753
- Li H, Wang Y, Che Z, Gou Y, Xu L, Lu B. [Effect of functional exercise at different time and different immobilization positions on functional recovery of elbow joint with type C distal humeral fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017 Aug 15;31(8):946-951. Chinese. doi: 10.7507/1002-1892.201701021. PMID: 29806431; PMCID: PMC8458583.
- Lauder, A., Richard, M.J. Management of distal humerus fractures. Eur J Orthop Surg Traumatol 30, 745–762 (2020).
Yette TRr, Weatherby PJ, Somerson JS. Complications of articular distal humeral fracture fixation: a systematic review and meta-analysis. Journal of Shoulder and Elbow Surgery 2921;30(8):1957-1867 - Moursy M, Wegmann K, Wichlas F, Tauber M. Distal humerus fracture in patients over 70 years of age: results of open reduction and internal fxation. Archives of Orthopaedic and Trauma Surgery (2022) 142:157–164.
- Wang X, Liu G. A comparison between perpendicular and parallel plating methods for distal humerus fractures: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020 Jun 5;99(23):e19602.
- Shih, CA., Su, WR., Lin, WC. et al. Parallel versus orthogonal plate osteosynthesis of adult distal humerus fractures: a meta-analysis of biomechanical studies. International Orthopaedics (SICOT) 2019;43449–460
- Tyllianakis M, Solou K, Lakoumentas J, et al. Long-Term Functional Outcomes and Complications of Intra-Articular (AO type B, C) Distal Humerus Fractures in Adults: A Retrospective Review. Cureus. 2022);14(1): e21094
- Saini R, Sharma A, Rathore KS, et al. Clinical and Functional Outcomes of Anatomical Plating in Distal Humerus Fractures in Adults Cureus 2013; 15(2): e35581
- Doornberg j, Lindenhovius A, Kloen P, et al. Two and three dimensional computed tomography for the classification and management of distal humeral fractures: evaluation of reliability and diagnostic accuracy. J Bone Joint Surg 2006;88:1795-1801.
- Dakouré PWH, Ndiaye A, Ndoye JM, et al. Posterior surgical approaches to the elbow: a simple method of comparison of the articular exposure. Surg Radiol Anat (2007) 29:671–674.
- Coles CP, Barei DP, Nork SE et al. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma 2006;20:164–171.
- Kudo T, Hara A, Iwase Het al. Biomechanical properties of orthogonal plate configuration versus parallel plate configuration using the same locking plate system for intra-articular distal humeral fractures under radial or ulnar column axial load. Injury. 2016;47(10):2071-2076.
- Shin SJ, Sohn HS, Do NH. A clinical comparison of two different double plating methods for intraarticular distal humerus fractures. J Shoulder Elb Surg. Journal of Shoulder and Elbow Surgery Board of Trustees; 2010;19(1):2–9.
- Lee SK, Kim KJ, Park KH, et al. A comparison between orthogonal and parallel plating methods for distal humerus fractures: a prospective randomized trial. Eur J Orthop Surg Traumatol. 2013;24: 1123–1131.
- Athanaselis ED, Komnos G, Deligeorgis D, et al. Double Plating in Type C Distal Humerus Fractures: Current Treatment Options and Factors that Affect the Outcome. Strategies Trauma Limb Reconstr. 2022 Jan-Apr;17(1):7-13.
- Harvey, Edward J. MD, MSc. In Older Adults with Distal Humeral Fractures, Total Elbow Arthroplasty Did Not Differ from Open Reduction-Internal Fixation for Reoperations in the Long Term. The Journal of Bone and Joint Surgery 102(10):p 907, May 20, 2020.
- Spierings KE, Schoolmeesters BJ, Doornberg JN, Eygendaal D, van den Bekerom MP. Complications of olecranon osteotomy in the treatment of distal humerus fracture. Clin Shoulder Elb. 2022 Jun;25(2):163-169. doi: 10.5397/cise.2021.00591. Epub 2022 Apr 4.PMID: 35545245
- Zlotolow DA, Catalano LW 3rd, Barron OA, Glickel SZ. Surgical exposures of the humerus. J Am Acad Orthop Surg. 2006 Dec;14(13):754-65. doi: 10.5435/00124635-200612000-00007.PMID: 17148623 Review
- Meldrum A, Kwong C, Archibold K, Cinats D, Schneider P. Olecranon Osteotomy Implant Removal Rates and Associated Complications. J Orthop Trauma. 2021 May 1;35(5):265-270. doi: 10.1097/BOT.0000000000001979.PMID: 33086235
- Beeres FJ, Oehme F, Babst R. Distal humerus fracture-extensile approaches. Oper Orthop Traumatol. 2017 Apr;29(2):115-124. doi: 10.1007/s00064-016-0474-4.PMID: 27921119 Review
- Lu S, Zha YJ, Gong MQ, Chen C, Sun WT, Hua KH, Jiang XY. Olecranon osteotomy vs. triceps-sparing for open reduction and internal fixation in treatment of distal humerus intercondylar fracture: a systematic review and meta-analysis. Chin Med J (Engl). 2021 Jan 27;134(4):390-397. doi: 10.1097/CM9.0000000000001393.PMID: 33617182
- Ting FSH, Huang A, Potra R, Ferreira L, King GJW. Morphology of Proximal Ulna Bare Area: A Guide for Olecranon Osteotomy. J Hand Surg Am. 2022 Sep 26:S0363-5023(22)00449-X. doi: 10.1016/j.jhsa.2022.07.010. Online ahead of print.PMID: 36175248
You might also be interested in:
AO Surgery Reference
AO Surgery Reference is your go-to resource for the management of fractures, based on current clinical principles, practices, and available evidence.
myAO
Join AO's digital network! On myAO, you can securely save and share cases, connect and exchange knowledge with peers, and access leading clinical and scientific expertise.
AO video hub
Discover a wealth of educational videos, practical exercises, recorded webinars, expert presentations, and interviews from AO's world-renowned faculty.