3D four-column classification and 3D images of complex tibial plateau fractures with posterior articular involvement: New tools for planning treatment
BY YAZAN HATTAR AND HANI ALSULAIMANY

Learning Objectives
This webinar will prepare participants
- to assess the complexity of tibial plateau injury and
- 0utline a stage approach to treating soft tissues in these fractures;
- to select the correct choice of imaging;
- to assess the fracture and its mechanism;
- to discuss options of surgical access; and
- to describe several implant options.
In correcting a complex tibial plateau fracture with posterior articular involvement, our primary objective is to allow for healing while keeping the joint supple, but without increasing the risk of complications, especially infection. Even with severely comminuted fractures, appropriate treatment decisions will allow most patients to return quickly and safely to functionality.
Fulfilling these objectives means first understanding the injury as fully as possible. What was the mechanism of the fracture? How many of the tibial columns are affected? Is there comminution? Is there an depression or hole punched in the tibial plateau? Equally importantly, is the soft tissue ready for a reduction? If so, what approach(es) and implants will allow us to reverse the damage most effectively? The optimal approach often involves multiple stages. And remember, if it comes to a choice between an imperfectly-united joint and a stiff one, the imperfectly united one is much easier to manage.
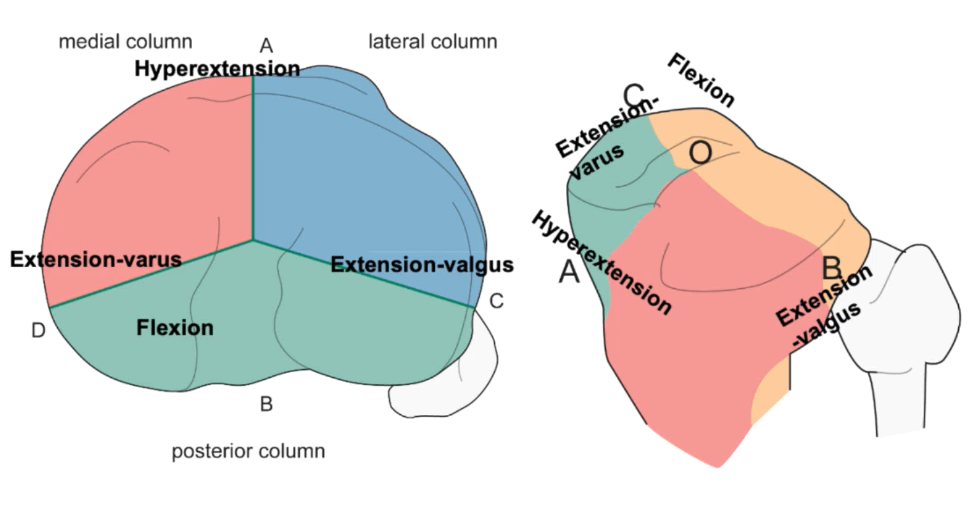
The first step is to use medical imaging to examine and classify the injury. For example, using the AO/OTA classification, considering that we’re focusing on complex fractures here, we are looking at B- or C-class fractures. Of these, the first complex classification would be a B3, with a split articular fracture and a plateau depression; the highest level of complexity—a C3—would involve fractures of two or more columns and multiple fragments or even comminution. The corresponding Schatzker classifications would be 2, 4, 5 or 6. Both the Schatzker and the AO/OTA classification systems have recently been upgraded to four-column conceptualizations. I.e., what was previously simply described as the posterior column is now divided into the posteromedial and the posterolateral columns.
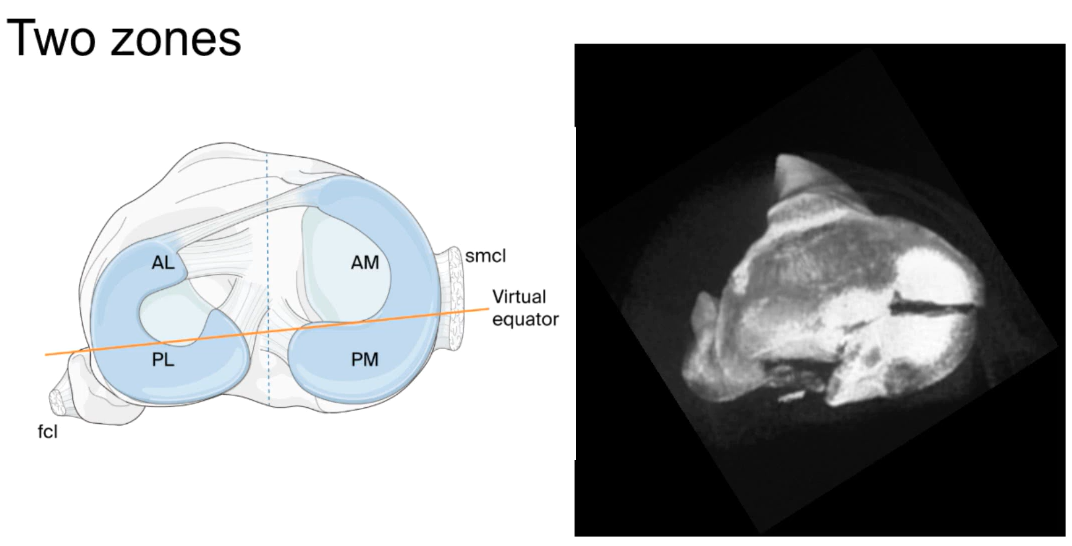
Both the AO/OTA and the Schatzker classification systems are still useful. However, both are built around two-dimensional views. The more recent CT-based 3D construct classification method, which inlvolves the use of specialized software to reconstruct CT scan slices into virtual 3-dimensional models, allows a clearer, brighter view of the fracture site. This is valuable not only for choosing the optimal fixation and instrumentation, but also for deciding on the approach that will allow the most efficient access to the affected areas.
Avoiding stiffness, infection or soft tissue damage is crucial
Regarding approaches, it is essential to consider the condition of the soft tissue. As this may be quite badly damaged either from the initial impact or from the movement of the bone ends, it may be necessary to immobilize the bone temporarily with an external fixator. This will distract the fracture until the soft tissue has settled down enough to withstand the necessary approach(es). Even if this makes it less likely that you will achieve a perfect reduction, an imperfect union is easier to manage than a stiff knee or an infection.
Where multiple structures must be accessed, it is also necessary to gauge, for example, the minimum number of approaches necessary both to buttress the main fragment and to address a tibial plateau depression with a graft. If two approaches are necessary, it may be possible to execute that approach without a major change to the patient’s position. The “floating position” is a good example of a flexible position that allows a range of changes in approach and access angles without re-draping.
Buttressing, double-plating and bridging may all be necessary
As for specific fixation techniques, considering the stress the knee joint needs to withstand, the larger fragments often require buttressing. Double-plating may also be appropriate, while smaller fragments may require bridging. Where evulsion has occurred, all affected fragments need to be either secured particularly well or removed. Nothing can be left to chance.
Also, as revisiting the surgical site greatly increases the chances of complications, the more problems that can be anticipated and addressed in a single operation, the better. By allowing maximal previsualization, 3D imaging allows the surgical team to prepare for virtually any necessity. As a general rule, though, where internal fixation is necessary, revision is particularly difficult and may extend the period of immobilization considerably. Therefore, do not settle for sub-optimal internal fixation.
Essential information: the mechanics of the injury
Clear 3-D imaging can also help us fill in one more vital piece of information: the mechanics of the injury itself. The better we can understand this, the more effectively we can reverse the forces that caused the fracture. For example, a hyperextension injury usually involves the anterior columns with varus or valgus extension. This could affect the medial and the lateral columns. And flexion injuries usually involve the posterior column—or columns, depending on whether we’re using a 3- or a 4-column model. In any case, the injury mechanics will also tell us where damage is most likely to have occurred on the tibial plateau. I.e., knowing the types and directions of the forces that caused the most obvious damage also allows us to investigate for less obvious damage that could lead to later complications. As noted, three-dimensional image reconstructions are tremendously useful for this.
To expand on this idea of how understanding the forces involved in the injury can help with our decision-making, a fracture commonly has a compression side and tension side. Initially, compression drives fragments inwards; meanwhile, on the opposite side, tension tension tends to pull comminuted fragments outward. In both cases, knowing the direction of the forces allows us to decide on appropriate approaches, fixation strategies and implants.
As tibial plateau injuries tend to be high-impact events, they often require a range of fixations, e.g., from buttressing of large fragments to bridging of smaller ones, as well as allo-, auto- or synthetic grafts (for plateau indentations). For these decisions, the older three-column-based classifications are still usually completely adequate. However, where damage affects the posterior column, a four-column description/classification allows us to distinguish easily between the posteromedial and -lateral quadrants. For surgeons, this information allows more comprehensive guidelines regarding our approach and fixation decisions.
Adding 3-D reconstructions of CAT or MRI images
To include the advantages of current imaging possibilities and computing power, a range of software solutions—some of them free and open-source—are available to convert slicing scans into three-dimensional virtual models. For study or demonstration purposes, the virtual models can even be 3D-printed in very little time. Most importantly, allowing us to view the injury site from all angles offers major advantages not only for deciding on our implantation and reduction strategies, but also on the finer details of access and patient positioning. By minimizing the time the patient is under anaesthesia, this also reduces the chances of complications.
Posterior approaches for posterior column fractures
Finally, many of us learned in medical school that we should avoid operating on the back of the knee. While this is generally still good advice, for tibial plateau fractures involving the posterior column, a posterior approach often offers the only acceptable access for the necessary fixation. In addition, as posterior approaches offer more limited space, smaller posterior implants are available to avoid impingement or overcrowding.
Most importantly, if you know the anatomy well and understand the mechanics of the fracture, you can do the necessary work without creating more problems further down the road. And if you’re not fully confident with this type of approach, nothing beats working with a surgeon who’s been there before. And again, when it comes to planning, paired with modern imaging options, the 3D column classification system will guide your approach very reliably.
To see several case examples and demonstrations, please watch our AO Trauma webinar:
About the Authors:
Yazan Hattar, Chairman AO Trauma Jordan Chapter, AOTMENA Education Committee Member, Specialty Hospital, Amman, Jordan
Hani Alsulaimany, MD, Assistant Professor of Orthopedics, King Saud bin Abdulaziz University for Health Sciences, King Abdulaziz Medical City, Educational Officer, AO Trauma (Saudi Arabia Chapter), Jeddah, Saudi Arabia.
Further readings:
Luo CF, Sun H, Zhang B, et al. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010 Nov;24(11):683-92. doi: 10.1097/BOT.0b013e3181d436f3.
You might also be interested in:
AO Surgery Reference
AO Surgery Reference is your go-to resource for the management of fractures, based on current clinical principles, practices, and available evidence.
myAO
Join AO's digital network! On myAO, you can securely save and share cases, connect and exchange knowledge with peers, and access leading clinical and scientific expertise.
AO video hub
Discover a wealth of educational videos, practical exercises, recorded webinars, expert presentations, and interviews from AO's world-renowned faculty.