Fracture-related infection: Consensus recommendations on diagnosis and treatment (an AO webinar)
BY WILLEM-JAN METSEMAKERS AND MICHAEL VERHOFSTAD
Learning Objectives of the Associated Webinar
Regarding fracture-related infections (FRIs), the linked webinar will help participants:
1. To appreciate the importance of
a. a well-established diagnosis
b. the implementation of a multidisciplinary team approach.
2. To recognize/understand/appreciate
a. the main treatment principles for FRIs;
b. factors that influence surgical decision-making; and
c. how to apply up-to-date treatment strategies for FRIs. The included video demonstrations show techniques of
i. Intramedullary canal reaming
ii. Shaping and placement of an antibiotic nail in the intramedullary canal
d. the importance of patient follow-up (as demonstrated in a later phase)
Learning Objectives of the Associated Webinar
Regarding fracture-related infections (FRIs), the linked webinar will help participants:
1. To appreciate the importance of
a. a well-established diagnosis
b. the implementation of a multidisciplinary team approach.
2. To recognize/understand/appreciate
a. the main treatment principles for FRIs;
b. factors that influence surgical decision-making; and
c. how to apply up-to-date treatment strategies for FRIs. The included video demonstrations show techniques of
i. Intramedullary canal reaming
ii. Shaping and placement of an antibiotic nail in the intramedullary canal
d. the importance of patient follow-up (as demonstrated in a later phase)
References
- Birt M.C., Anderson D.W., Toby E.B., Wang J. Osteomyelitis: Recent advances in pathophysiology and therapeutic strategies. J. Orthop. 2016;14:45–52. doi: 10.1016/j.jor.2016.10.004. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]. From Lu, Zhang, et al., Fracture Related Infections and Their Risk Factors for Treatment Failure—A Major Trauma Centre Perspective, Diagnostics (Basel). 2022 May; 12(5): 1289. Published online 2022 May 22. doi: 10.3390/diagnostics12051289
- Bezstarosti H., Van Lieshout E.M.M., Voskamp L.W., Kortram K., Obremskey W., McNally M.A., Metsemakers W.J., Verhofstad M.H.J. Insights into treatment and outcome of fracture-related infection: A systematic literature review. Arch. Orthop. Trauma Surg. 2019;139:61. doi: 10.1007/s00402-018-3048-0. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]. From Lu, Zhang, et al., Fracture Related Infections and Their Risk Factors for Treatment Failure—A Major Trauma Centre Perspective, Diagnostics (Basel). 2022 May; 12(5): 1289. Published online 2022 May 22. doi: 10.3390/diagnostics12051289
- Mario Morgenstern et al., July 2018, The value of quantitative histology in the diagnosis of fracture-related infection. Bone and Joint Journal 100-B(7):966-972. DOI:10.1302/0301-620X.100B7.BJJ-2018-0052.R1
- Justin VC Lemans, et al., The diagnostic accuracy of 18F-FDG PET/CT in diagnosing fracture-related infections. Eur J Nucl Med Mol Imaging. 2019; 46(4): 999–1008. Published online 2018 Dec 7. doi: 10.1007/s00259-018-4218-6. PMCID: PMC6450834. PMID: 30523391
- GAM Govaert et al., High diagnostic accuracy of white blood cell scintigraphy for fracture related infections: Results of a large retrospective single-center study. Injury. Volume 49, Issue 6, June 2018, Pages 1085-1090
- Melissa Depypere et al., Recommendations for Systemic Antimicrobial Therapy in Fracture-Related Infection: A Consensus From an International Expert Group, J Orthop Trauma. 2020 Jan;34(1):30-41. doi: 10.1097/BOT.0000000000001626
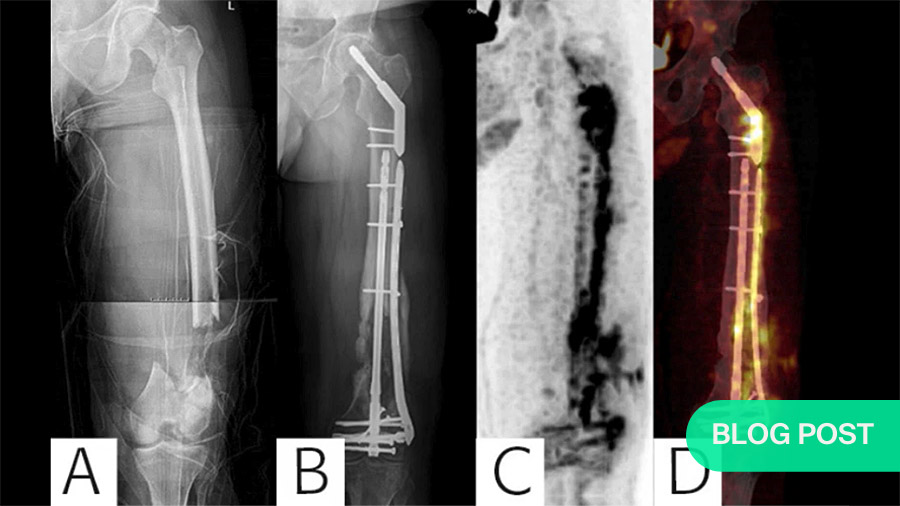
The figure at top of page was published in the following paper:
Diagnosing Fracture-Related Infection: Current Concepts and Recommendations.
Govaert GAM, Kuehl R, Atkins BL, Trampuz A, Morgenstern M, Obremskey WT, Verhofstad MHJ, McNally MA, Metsemakers WJ; Fracture-Related Infection (FRI) Consensus Group. J Orthop Trauma. 2020 Jan;34(1):8-17. doi: 10.1097/BOT.0000000000001614.
Further readings
-
Read more ...
- Musculoskeletal Infection in Orthopaedic Trauma: Assessment of the 2018 International Consensus Meeting on Musculoskeletal Infection.
Obremskey WT, Metsemakers WJ, Schlatterer DR, Tetsworth K, Egol K, Kates S, McNally M; ICM Orthopaedic Trauma Work Group*; ICM Orthopaedic Trauma Work Group*.
J Bone Joint Surg Am. 2020 May 20;102(10):e44. doi: 10.2106/JBJS.19.01070.
PMID: 32118653 - Intramedullary tissue cultures from the Reamer-Irrigator-Aspirator system for diagnosing fracture-related infection.
Onsea J, Pallay J, Depypere M, Moriarty TF, Van Lieshout EMM, Obremskey WT, Sermon A, Hoekstra H, Verhofstad MHJ, Nijs S, Metsemakers WJ.
J Orthop Res. 2021 Feb;39(2):281-290. doi: 10.1002/jor.24816. Epub 2020 Aug 10.
PMID: 32735351 - Evidence-Based Recommendations for Local Antimicrobial Strategies and Dead Space Management in Fracture-Related Infection.
Metsemakers WJ, Fragomen AT, Moriarty TF, Morgenstern M, Egol KA, Zalavras C, Obremskey WT, Raschke M, McNally MA; Fracture-Related Infection (FRI) consensus group.
J Orthop Trauma. 2020 Jan;34(1):18-29. doi: 10.1097/BOT.0000000000001615.
PMID: 31464858 Free PMC article.Review. - Validation of the diagnostic criteria of the consensus definition of fracture-related infection.
Onsea J, Van Lieshout EMM, Zalavras C, Sliepen J, Depypere M, Noppe N, Ferguson J, Verhofstad MHJ, Govaert GAM, IJpma FFA, McNally MA, Metsemakers WJ.
Injury. 2022 Jun;53(6):1867-1879. doi: 10.1016/j.injury.2022.03.024. Epub 2022 Mar 12.
PMID: 35331479 - Recommendations for Systemic Antimicrobial Therapy in Fracture-Related Infection: A Consensus From an International Expert Group.
Depypere M, Kuehl R, Metsemakers WJ, Senneville E, McNally MA, Obremskey WT, Zimmerli W, Atkins BL, Trampuz A; Fracture-Related Infection (FRI) Consensus Group.
J Orthop Trauma. 2020 Jan;34(1):30-41. doi: 10.1097/BOT.0000000000001626.
PMID: 31567902 Free PMC article. - Diagnostic challenges and future perspectives in fracture-related infection.
Morgenstern M, Kühl R, Eckardt H, Acklin Y, Stanic B, Garcia M, Baumhoer D, Metsemakers WJ.
Injury. 2018 Jun;49 Suppl 1:S83-S90. doi: 10.1016/S0020-1383(18)30310-3.
PMID: 29929701 Review. - The Incidence of Fracture-Related Infection in Open Tibia Fracture with Different Time Interval of Initial Debridement.
Hadizie D, Kor YS, Ghani SA, Mohamed-Saat MA.
Malays Orthop J. 2022 Nov;16(3):24-29. doi: 10.5704/MOJ.2211.005.
PMID: 36589367 Free PMC article. - General treatment principles for fracture-related infection: recommendations from an international expert group.
Metsemakers WJ, Morgenstern M, Senneville E, Borens O, Govaert GAM, Onsea J, Depypere M, Richards RG, Trampuz A, Verhofstad MHJ, Kates SL, Raschke M, McNally MA, Obremskey WT; Fracture-Related Infection (FRI) group.
Arch Orthop Trauma Surg. 2020 Aug;140(8):1013-1027. doi: 10.1007/s00402-019-03287-4. Epub 2019 Oct 29.
PMID: 31659475 Free PMC article. - Diagnosing Fracture-Related Infection: Current Concepts and Recommendations.
Govaert GAM, Kuehl R, Atkins BL, Trampuz A, Morgenstern M, Obremskey WT, Verhofstad MHJ, McNally MA, Metsemakers WJ; Fracture-Related Infection (FRI) Consensus Group.
J Orthop Trauma. 2020 Jan;34(1):8-17. doi: 10.1097/BOT.0000000000001614.
PMID: 31855973 Free PMC article. - Fracture-related infection: A consensus on definition from an international expert group.
Metsemakers WJ, Morgenstern M, McNally MA, Moriarty TF, McFadyen I, Scarborough M, Athanasou NA, Ochsner PE, Kuehl R, Raschke M, Borens O, Xie Z, Velkes S, Hungerer S, Kates SL, Zalavras C, Giannoudis PV, Richards RG, Verhofstad MHJ.
Injury. 2018 Mar;49(3):505-510. doi: 10.1016/j.injury.2017.08.040. Epub 2017 Aug 24.
PMID: 28867644 - Fracture-related infection.
Moriarty TF, Metsemakers WJ, Morgenstern M, Hofstee MI, Vallejo Diaz A, Cassat JE, Wildemann B, Depypere M, Schwarz EM, Richards RG.
Nat Rev Dis Primers. 2022 Oct 20;8(1):67. doi: 10.1038/s41572-022-00396-0.
PMID: 36266296 Review. - Pathogenesis and management of fracture-related infection.
Depypere M, Morgenstern M, Kuehl R, Senneville E, Moriarty TF, Obremskey WT, Zimmerli W, Trampuz A, Lagrou K, Metsemakers WJ.
Clin Microbiol Infect. 2020 May;26(5):572-578. doi: 10.1016/j.cmi.2019.08.006. Epub 2019 Aug 22.
PMID: 31446152 Review. - Infection after fracture fixation: Current surgical and microbiological concepts.
Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MHJ, Borens O, Kates S, Morgenstern M.
Injury. 2018 Mar;49(3):511-522. doi: 10.1016/j.injury.2016.09.019. Epub 2016 Sep 11.
PMID: 27639601 Review. - Fracture-related infection.
Baertl S, Metsemakers WJ, Morgenstern M, Alt V, Richards RG, Moriarty TF, Young K.
Bone Joint Res. 2021 Jun;10(6):351-353. doi: 10.1302/2046-3758.106.BJR-2021-0167.R1.
PMID: 34076501 Free PMC article.No abstract available. - Definition and diagnosis of fracture-related infection.
McNally M, Govaert G, Dudareva M, Morgenstern M, Metsemakers WJ.
EFORT Open Rev. 2020 Oct 26;5(10):614-619. doi: 10.1302/2058-5241.5.190072. eCollection 2020 Oct.
PMID: 33204503 Free PMC article.Review. - Bone infection: a clinical priority for clinicians, scientists and educators.
Moriarty TF, Muthukrishnan G, Daiss JL, Xie C, Nishitani K, Morita Y, Awad H, de Mesy Bentley KL, Masters E, Bui T, Yan M, Owen J, Mooney B, Gill S, Puetzler J, Wenke JC, Morgenstern M, Metsemakers WJ, Noll C, Joeris A, Richards RG, Schwarz EM, Kates SL.
Eur Cell Mater. 2021 Oct 18;42:312-333. doi: 10.22203/eCM.v042a21.
PMID: 34661245 Review.
- Musculoskeletal Infection in Orthopaedic Trauma: Assessment of the 2018 International Consensus Meeting on Musculoskeletal Infection.
You might also be interested in:
AO Surgery Reference
AO Surgery Reference is your go-to resource for the management of fractures, based on current clinical principles, practices, and available evidence.
myAO
Join AO's digital network! On myAO, you can securely save and share cases, connect and exchange knowledge with peers, and access leading clinical and scientific expertise.
AO video hub
Discover a wealth of educational videos, practical exercises, recorded webinars, expert presentations, and interviews from AO's world-renowned faculty.



