Radial Nerve Palsy Following Humeral Fractures
BY ASHRAF MOHARRAM AND SIMON LAMBERT
About this Blog
Alongside a humerus fracture, a radial nerve palsy requires a number of decisions. What are my imaging and diagnostic options? Is surgery indicated? If so, which approaches and fixation techniques offer the best chances of recovery?
As Heckler and Bamberger (2008) observed, the available literature can support almost any approach to treating this combination of injuries. This blog and the linked webinar will help you sift through the available information and make decisions that lead to consistently high-quality outcomes for your patients.
Recovery needs
Radial nerve palsy accompanies around 12% of humerus fractures, making it the most common peripheral nerve outcome of long bone injuries. Its functional implications are debilitating, including wrist and finger drop, recovery rates are high. Still, the most reliable path to recovery is not always the most obvious: in many cases, expectant management is recommended. Indications depend, for example, on the type of fracture, whether your imaging suggests entrapment, and whether the patient urgently needs to regain function.
How likely is a radial nerve injury in this case?
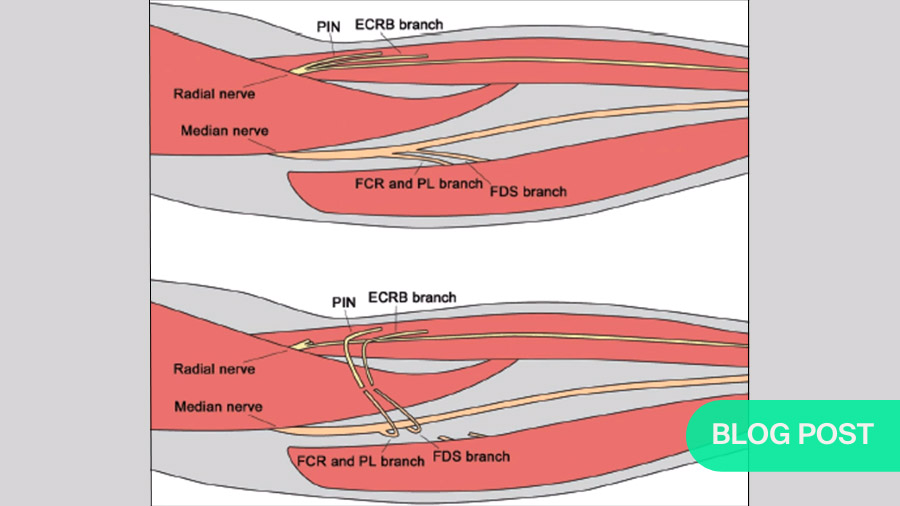
Radial nerve injuries usually occur in fractures affecting a 10–15cm path where the radial nerve courses along the periosteum of the middle and middle-distal humerus. As the nerve has very little mobility in this area, but has only minimal protection, it is highly susceptible to injury.
Transverse and spiral fractures are most likely to result in palsy. These are followed by displaced high-energy fracture patterns. In cases of displacement, stretching is a common source of injury. As stretches as short as 1–2mm can cause damage, virtually any tension is problematic. This also applies to management of the injury.
Holstein-Lewis fractures
Until quite recently, Holstein-Lewis fractures (displaced oblique fractures of the distal humerus) were automatically considered an indication for surgery. However, a systematic review by Shao et al. (2005) showed that the available data did not support surgery. Three years later, when Eckholm (2008) studied 361 cases involving such fractures, they found equal outcomes for fracture and radial nerve recovery with and without surgery.
Indication for immediate exploration
Shao et al. (2005) also reviewed cases of open and closed fractures. In that case, they found no difference between open and closed fractures regarding the incidence of radial nerve palsy. However in cases of open fractures where palsy was present, they found higher incidence of laceration, transection and entrapment.
Therefore, open fractures with radial nerve palsy indicate immediate exploration.
Indication for early exploration and repair
Much more recently, EM Hegeman et al. (2020) published a study of 200 humerus fractures with radial nerve palsy. They found that 65% of palsies involved either no outwardly visible damage to the nerve or very mild damage, i.e., neuropraxia. The remaining 35% involved entrapment (15%), transection (12%) or laceration (8%). Cases of neurotmesis (complete transection) are signaled by loss of brachioradialis function, wrist drop and finger drop. These symptoms indicate early exploration, followed by repair within two weeks.
Indications for also exploring the radial nerve
Certain types of injury indicate exploration of the radial nerve. These include all open humerus fractures, associated vascular injuries (often signaled by a “floating elbow”), high-velocity wounds such as gunshots, penetrating injuries, cases including severe soft tissue damage, and those suggesting nerve laceration.
However, many surgeons consider any humeral fracture that requires surgery and accompanies a preoperative radial nerve palsy an indication of exploring the radial nerve. This strategy is supported by Hegeman et al. (2020), who found that exploration and neurolysis during humerus fracture management led to much higher rates of recovery than expectant management.
Other advantages of exploring the radial nerve with fixation of the humerus include an opportunity to stabilize free-floating bone fragments, check for any lesions on the radial nerve, prevent or correct entrapment, or repair nerve lacerations. Additionally, if it is necessary to shorten the humerus, e.g., to overcome a gap in the radial nerve, this is much easier before bone healing has progressed. Perhaps most importantly, early repair of the nerve (within three weeks) leads to roughly 90% recovery; after that, recovery averages about 68%.
Arguments against early exploration
In cases with no specific signs, e.g., of neurotmesis, some surgeons suggest a more hands-off approach. As spontaneous recovery rates are high, common arguments against early exploration include the risk of complications, or the fact that treating a radial nerve with a healed fracture is much easier than with an unhealed, mobile one. Another is that the neurilemmal sheath’s tendency to thicken with time can help define the extent of the damage, thereby facilitating a repair.
To look for evidence for or against early exploration without specific indications to do so, LAM Hendrickx (2021) conducted a systematic review of 1758 radial nerve palsy cases. Comparing cases where surgeons explored the radial nerve during open/operative humerus reduction vs those that involved closed reductions and no radial nerve treatment, they found no difference in recovery rates.
Further, regarding recovery of primary radial nerve palsy, when comparing patients managed non-operatively versus those explored early, they concluded that no beneficial effect could be demonstrated.
Therefore, if no indications are clear while you are fixing your humerus, there is no benefit to invasively exploring your radial nerve.
Again, Shao et al. (2005) supported a patient approach. Their systematic review indicated that, in cases with no specific indication for surgery on their own, there was no significant benefit to earlier versus later operative intervention.
So, with a closed humerus fracture with no indication of surgery on its own, a primary radial nerve palsy isn’t an indication for invasive exploration. This is also true with Holstein-Lewis fractures. With close management of these fractures and expectant treatment of the radial nerve palsy, spontaneous recovery should be expected, with recovery rates of 73–90%.
Treatment options for primary radial nerve palsy with closed humerus fractures
Expectant treatment vs Early exploration
Where there are no clear indications for surgery and the injury is managed by expectant observation, the nerve recovers in 73–92% of cases. Where no recovery is occurring, later exploration and, if necessary, nerve transfer are possible. If recovery still fails, tendon transfer is also possible.
Expectant treatment includes exercises to preserve the range of motion, dynamic splinting, and four-week follow-ups to monitor progress. The latter step includes regular checks for a progressive Tinel’s sign, which is a strong indicator of nerve recovery.
Diagnostic Technology
The role of EMG
Electromyography (EMG) baseline measurements should be taken first three to four weeks, then twelve weeks after the injury. If no nerve growth is occurring, readings can accelerate indications for reinnervations by about four weeks. Where they show recovery, expectant management can continue.
Ultrasonography
One diagnostic tool growing in popularity is ultrasonography. A sonogram allows an experienced viewer to differentiate severed from intact nerves and identify entrapped ones. This can eliminate much of the need for invasive exploration.
Sonography is an inexpensive, relatively portable, non-invasive and painless technology. Prospective clinical studies have showed high correlation between ultrasound readings and operative findings. In cadaveric studies, sonographic readings showed sensitivity of 89% and specificity of 95%. However, it is not yet part of standard diagnostic workups. This is at least partly because ultrasonography is a very observer-dependent process, i.e., understanding sonograms takes practice.
Therefore, given its accuracy and non-invasiveness, ultrasound’s use should be increased.
Recovery timeframe
Recovery from radial nerve palsy averages 24 weeks. For low-impact injuries sign of recovery can appear as early as three weeks, with full recovery common in twelve. In high-impact cases, some recovery should be measurable at 14 weeks, with full recovery at six months.
Summary
Radial nerve palsy is a common but complex problem. The following is a very brief summary of the 5 major topics and associated points I hope you will take away from this discussion. Please note that some of these points refer to the procedures summarized in point form below.
- Ultrasound is a tremendously useful tool to identify severed, lacerated or entrapped nerves.
- Early nerve exploration and fixation of humerus is recommended for patients with open fractures, fractures otherwise indicated for surgical fixation, or secondary radial nerve palsy, or if ultrasounds show entrapment, or laceration.
- Expectant treatment should include EMGs at four–six weeks (baseline), another at twelve weeks, and clinical follow-up that includes Tinel sign tests. If there are signs of recovery, non-operative treatment can continue. If not, a late surgical intervention is indicated. However, never wait more than six months post-op to do so.
- Treatment options for late surgical interventions include neurorrhaphy, nerve grafting, internal splinting, nerve transfer, and tendon transfer.
- And finally in cases of secondary nerve palsy, if you visualize your nerve during the procedure, treat it expectantly. If not, an immediate exploration is warranted.
AO Trauma thanks Ashraf Moharram for this highly informative weblog and the webinar it accompanies. We also thank Simon Lambert for his generous participation in the question-and-answer period that follows the webinar.
Watch the webinar:
About the author:
You might also be interested in:
AO Surgery Reference
AO Surgery Reference is your go-to resource for the management of fractures, based on current clinical principles, practices, and available evidence.
myAO
Join AO's digital network! On myAO, you can securely save and share cases, connect and exchange knowledge with peers, and access leading clinical and scientific expertise.
AO video hub
Discover a wealth of educational videos, practical exercises, recorded webinars, expert presentations, and interviews from AO's world-renowned faculty.




