Periprosthetic fractures, management of the hip and the knee
Periprosthetic femoral fractures most commonly result from low-energy falls, usually affecting the proximal femur. Commonly, this means damage to a hip prosthesis, i.e., a fracture below the prosthesis, loosening of the prosthesis in the femur, or both. In the US, the majority of cases occur in women aged a mean of 82.5 years.
As these injuries’ annual incidence is expected to go on rising for some time, this blog’s first two segments discuss surgeons’ most important considerations regarding treatment options. The third section deals with periprosthetic joint infections (PJIs), which affect 1–2% of joint replacement recipients in the US. While PJIs are a serious concern everywhere, they are particularly dangerous in developing countries. This segment discusses the challenges of working in an area without access to state-of-the-art diagnostic systems, and where many patients cannot afford full treatment.
This blog post is based on a webinar presented by Drs Michael Schütz, Ismail Hadisoebroto Dilogo, Dwikora Novembri Utomo, Takeshi Sawaguchi, and Andito Wibisono. It summarizes the pathology, biomechanics, and revision techniques, as well as the stability concept of periprosthetic fracture fixation for the hip and knee. Also, periprosthetic bone loss and infection problems and how to deal with these complications are covered.
- State of the art: fixation in periprosthetic fractures provides information on current classification systems, prosthesis replacement and fixation options.
- Revision of total hip arthroplasty for periprosthetic fractures around the hip describes diagnostic and corrective considerations involving hip prosthetic revisions, plus suggestions regarding acetabular defect classifications, correction techniques and recommended implants.
- Periprosthetic joint infection discusses essential considerations regarding PJIs, beginning with the addition of several infection specialists to the surgical team, as well as choosing between various international diagnostic criteria. A two-stage PJI treatment algorithm is also discussed.
State of the art: fixation in periprosthetic fracture
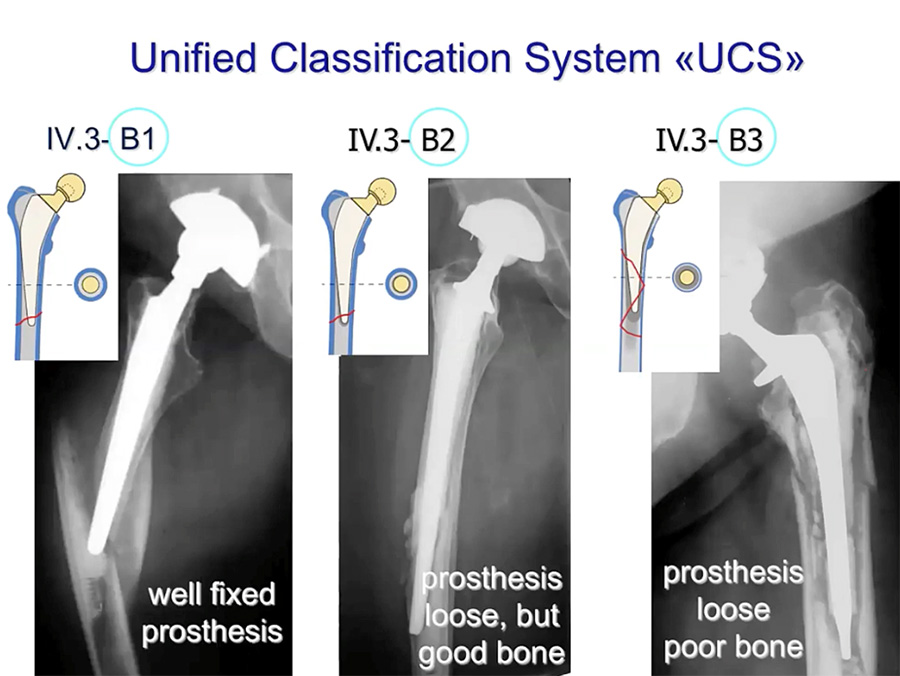
UCS classification of periprosthetic fractures
After taking a thorough patient history regarding the injury, particularly pain or signs of infection, the surgeon should check the patient’s records for previous x-rays or follow-up reports. In current x-rays, a lateral or AP view should show continuous radiolucency at the cement/stem-bone interface, as well as any evidence of the cement fracturing or de-bonding from the implant. To determine the way forward, the Unified Classification System (UCS) for periprosthetic fractures is very useful. As with other classification systems, based on the type and complexity of the fracture, as well as the condition both of the implant and of the surrounding bone, a UCS classification provides a reliable starting point to decide on the most appropriate reduction and fixation options.
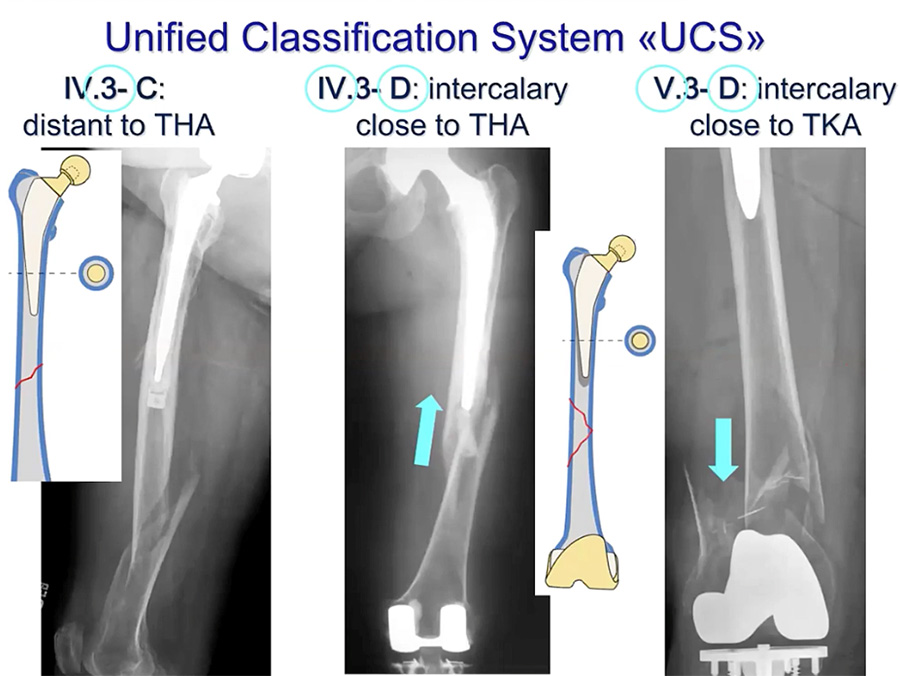
Stability of the prosthesis and bone
The prosthesis may be well-fixed or loose, the bone can be in good or poor condition. The rather simple fractures above are all class B. More complex fractures—classes C and D—are shown below. In the third case, a CT scan is recommended (if possible), looking carefully for signs that the prosthesis has loosened. This lecture focuses on fracture reduction and fixation.
10:22: Supplementary Fixation Options
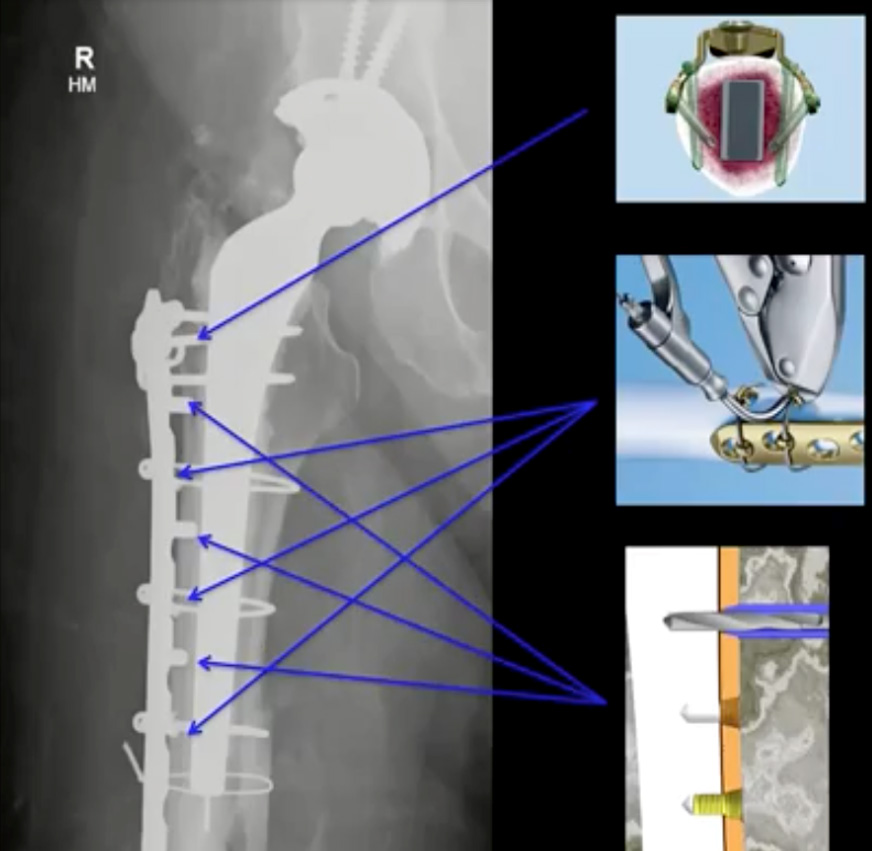
The indicated fixation options are long plating. For more fragmented or comminuted fractures, it is useful to put the necessary plating loosely in place, but not add screws immediately. In preparation for drilling and screwing, cerclage should be used both to reduce the fracture and to pull the plating firmly into place. Only once the implant is oriented as needed and the cerclage tightened should any necessary holes be bored and screws added. If any screws are in place before the cerclage is tightened, the compression can move them, destroying their threading in the bone.
After the plate is fitted to the contours of the femur and roughly in place, cerclage wires can be inserted around the femur. This requires using curved trocars to encircle the femur, then feeding cerclage wire through. Minimally invasive techniques such as this shorten operative time, reduce bleeding and minimize fracture exposure. In the diagram above, the upper-right illustration shows how variable-angle screws can be oriented both to maximize the implant’s stability and to screw beside the implant stem.
Overall, since the introduction of locking plates in the late nineties, and more recently, the development of specialized periprosthetic screws and variable angle screws and locking plates, advances in periprosthetic surgery have greatly broadened the range of flexible, stable fixation options.
Alongside recent developments in periprosthetic technology and surgical technique, demographic ageing has greatly increased the incidence of certain patient-specific complications. As we see more patients living into their eighties and beyond, we must contend with greater incidences of age-linked comorbidities, particularly osteoporosis and cognitive decline. So, while the former of these makes fractures both more likely and more difficult to stabilize, the latter impairs patients’ abilities either to avoid fractures or to comply with complex post-surgical therapeutic regimens. Consideration of such issues is essential to decide on the most appropriate approach for each patient.
Given the number of factors at play, the chief advantage of the advancements noted above is not that they give us a single solution for all patients, but that they allow us to better tailor our treatment decisions to each client’s specific characteristics and needs.
Revision of total hip arthroplasty on periprosthetic fracture around the hip
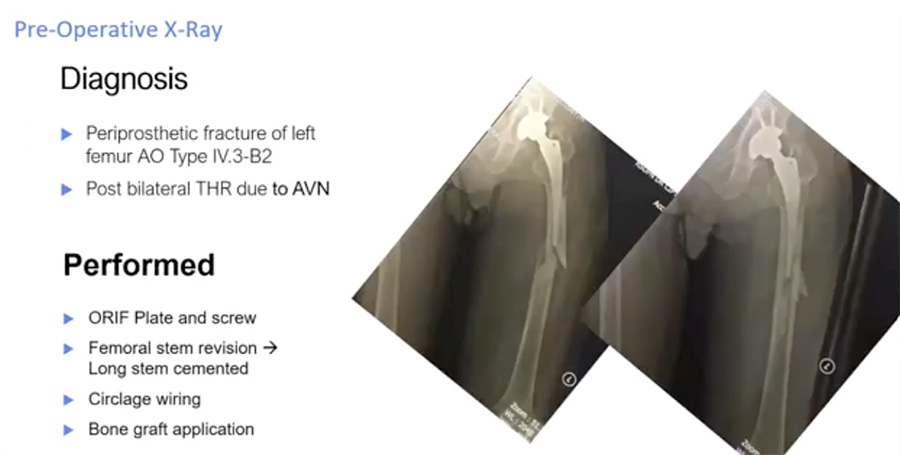
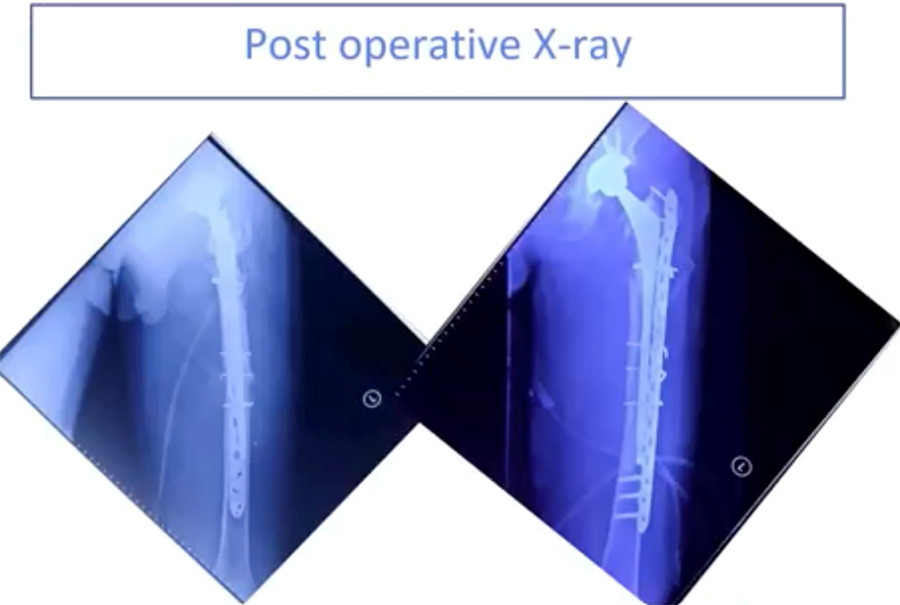
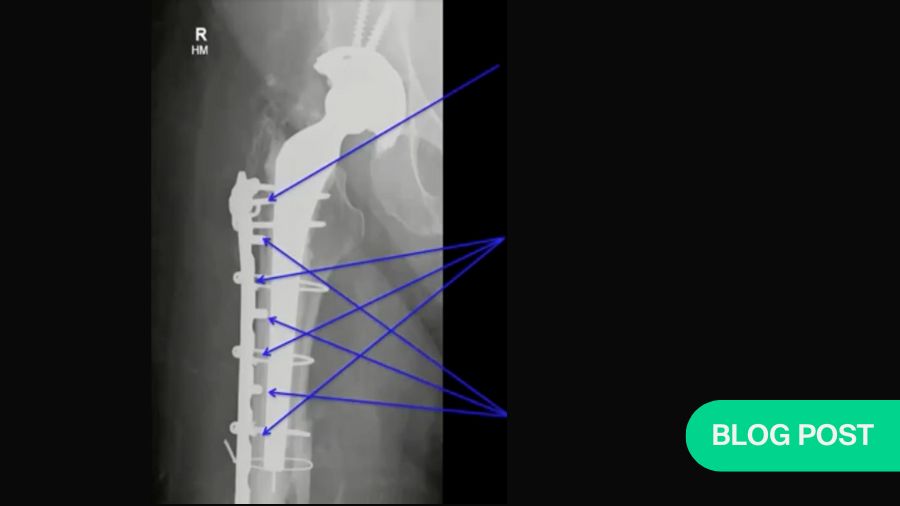
Below are two radiographs of an AO type IV.3–B2 periprosthetic hip fracture in a 56-year-old male. This patient received a total hip replacement seven years previously due to avascular necrosis (AVN). The fracture occurred one month before his hospital admission.
Evidence favors ORIF plus revision of the total hip arthroplasty (rTHA)
B2 periprosthetic fractures indicate long-stem hip arthroplasty revision.1
After ORIF using minimally invasive plate osteosynthesis (MIPO) techniques, the patient’s post-operative x-rays (below) show a well-reduced fracture with a stable implant, the stem of which extends well past the fracture site. To optimize conditions for fracture healing, the new stem should extend at least two femoral diameters past the fracture or defect.
10:22: Supplementary Fixation Options
The indicated fixation options are long plating. For more fragmented or comminuted fractures, it is useful to put the necessary plating loosely in place, but not add screws immediately. In preparation for drilling and screwing, cerclage should be used both to reduce the fracture and to pull the plating firmly into place. Only once the implant is oriented as needed and the cerclage tightened should any necessary holes be bored and screws added. If any screws are in place before the cerclage is tightened, the compression can move them, destroying their threading in the bone.
TEXT TEXT TEXT ROW
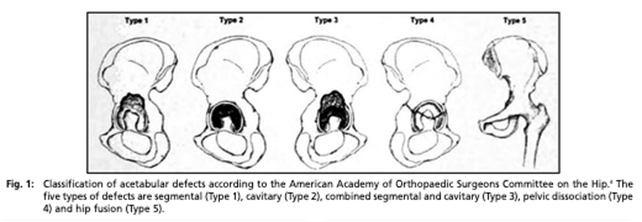
AAOS classifications10 use five main defect types and three sub-types:
I. Segmental defect
II. Cavitary defect
III. Combined segmental and cavitary defect
IV. Pelvic discontinuity
A. With mild segmental or cavitary loss
B. With moderate to severe segmental or cavitary loss
C. With prior pelvic irradiation
V. Hip arthrodesis (fusion)
The Paprosky Classification system for acetabular bone11
The Paprosky classification system is also widely used. While this only specifies three main classes, i.e., degrees of severity, Type II includes three sub-types and Type III includes two. To arrive at a classification, we evaluate the defect based on four variables: femoral head migration, ischial osteoporosis, the Kohler line, and the teardrop.
Correcting for acetabular bone defects
Impaction grafting
For simple segmental or combined structural bone defects (AAOC I, III; Paprosky IIA, B, C) , impaction grafting and cementation can be used with a metal mesh to contain and strengthen the bone-deficient areas. In addition to restoring the bone stock, the mesh allows the surgeon to cement a polyethylene liner into place.
Non-cemented hemispherical acetabular reconstruction
Another possibility is a non-cemented hemispherical acetabular reconstruction. This requires column and partial rim support, e.g., via screws, as well as supplemental fixation. Various fixation options, including porous metal implants, are available to enhance stability and promote biological fixation. Structural allografts are also possible.12
Structural allograft reconstruction
A third possibility, where the host acetabular bone is inadequate for stable component fixation, is structural allograft reconstruction.13 For hip acetabular reconstruction, allografts have largely been replaced by porous metal augmentations; however, if those are unavailable, allografts still offer satisfactory mid- and long-term results.
Modular porous metal augments
For Paprosky types II, IIIA and IIIB (superior rim defects), non-cemented hemispheric or elliptical components are indicated, in combination with modular augments. This type of augment both supports the acetabular component while bone grows in.14
Oblong cup implant
For Paprosky types IIB and IIIA, an oblong cup provides mechanical stability on the host bone, with relatively little bone removal required to match the defect.15 However, bear in mind that an oblong cup covers and replaces the defective bone rather than reconstructing it. Therefore, if any future revision is necessary, the surgeon will have much less bone to work with.
Ring and Case reconstruction
In contrast to the oblong cup, the roof reinforcement ring (e.g., a Ganz ring) and the antiprotrusio cage (e.g., a Burch-Schneider cage) are designed both to provide a scaffold for bone growth and to protect allografted tissue during the remodeling phase. These are recommended for AAOS Types III and IV.
As well as allowing a liner to be positioned independently of the ring position using antibiotic-treated cement, this system facilitates the elution of antibiotics from that cement. However, roughly 20% of cages fracture or loosen within 10 years.16
Kerboull-Tanaka plate and allograft
The Kerboulli-Tanaka plate is an excellent choice for acetabular reconstruction. Designed by Kerboulli and modified by Tanaka, this plate guides reconstruction of bone stock, particularly in the hip center. This is advantageous if revision becomes necessary. A long-term reliability study by Kim et al. (2015) indicated 10-year survival rates >94%.17
Summary:
Revision surgery in acetabular and femoral bone defect demands an evaluation of the bone loss.
Key treatment concerns are good bone restoration and rigid fixation of the component.
Bone loss may be addressed via an acetabular revision system or a (cemented or cementless) stem system with morselized or structural allograft.
Periprosthetic Joint Infection (PJI)
As the number of people who need arthroplasty is increasing, so is the number of infections. Outcomes include morbidity and mortality. In areas where few people have health insurance, treatment is also very expensive.
Dealing efficiently with an infection requires a combination of knowledge and experience. So, for surgeons who only see a small number of infections per year, it is essential to read and understand the literature and to participate either in webinars or in actual operations whenever possible.
Additional team members will be necessary
Tackling this type of problem requires a high level of teamwork. In addition to the usual surgical team members, an infection team includes a microbiologist, a histobiologist experienced with joint and bone infection, and a pathophysiologist to identify the origin of whatever is found. Clear radiological images and a full set of laboratory results will also be necessary.
That is, finding a reliable diagnosis for PJI requires a combination of clinical evidence. Once we are certain the joint is infected, we need to identify the organism responsible, its origin and route. Then we can choose the appropriate antibiotics both to treat it and to prevent its recurrence.
Preoperative testing
Preoperative exploration requires hematological testing. For example, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) tests will give important information on inflammation, as will medical imaging, including X-rays and PET scans. The synovial fluid will need to be tested. If a culture can be identified, is it gram-positive or -negative? Leukocyte and leukocyte esterase counts will also be necessary.
Intraoperative testing
Intraoperative tissue samples can provide vital histopathology and gram information. There are also several new methods that can be very useful. In Indonesia, for example, surgeons have access to polymerase chain reaction (PCR), but not sonication, microcalorimetry or mass spectrometry.
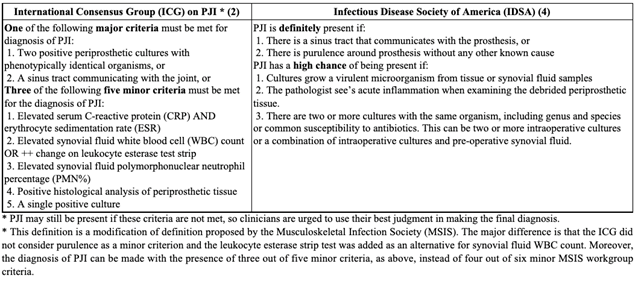
International Consensus Group (ICG) criteria
The International Consensus Group offers a similar set of criteria. While their major criteria are that same as those of the MSIS, their scoring system is simpler: The presence of any three of the five minor criteria indicates an infection. 18
Preventive preoperative antibiotics: Timing is important
According to WHO guidelines, preventive preoperative antibiotics should be started one hour before surgery, then discontinued after 24 hours.
Intraoperative cultures are still necessary
Very early Tsukuyama Type I19 infections may not yield positive preoperative test results. Therefore, intraoperative tissue samples should be taken from multiple locations. If a notable infection is detected, it may be necessary to procede with the operation in stages.
For longer-term infections, the Zimmerli classification system may be more useful.
Route of infection
Infections can be introduced via wounds, during surgery, or hematogenously. Hematogenic infections commonly originate in the mouth. Among diabetics, infections of the extremities also commonly spread to other parts of the body.
DAIR:
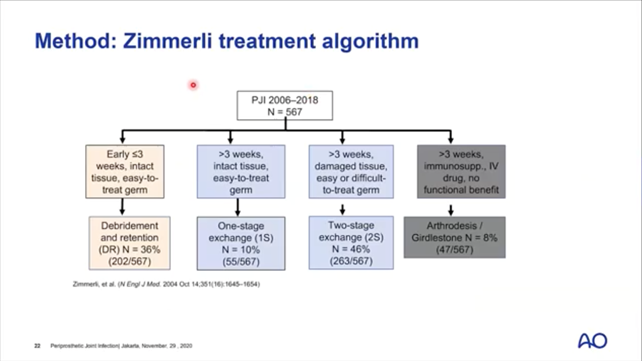
Where infection is present, a combination of debridement, antibiotics, and implant retention (DAIR) is recommended. Following Zimmerli’s algorithm (below), for infections more that 3 weeks old, a multi-stage approach may also be necessary. In some cases, the only possibility is a salvage operation.
Most common choice with PJI: 2-stage exchange
Where an infection is present, the most common choice among surgeons is a two-stage exchange. In the first stage, they remove the implant, debride the site and install an antibiotic-impregnated cement spacer. After waiting for the antibiotics to take effect (2-6 weeks, depending on the institution), the new prosthesis can be implanted and the tissue biopsied. In all cases, the patient should take oral antibiotics for six weeks.
Special patient considerations
Certain patient conditions, e.g., immunosuppression or cognitive decline, require special consideration.
Country-specific considerations
In developing countries, because of financial concerns, patients often arrive at a very advanced state of infection, and may opt for only the first part of a multi-stage treatment. Also, certain antibiotics may not be available. For example, at the time of this lecture, Daptomycin and Tobramycin were unavailable in Indonesia.
Watch a recording of the AO Trauma expert presentations on periprosthetic fractures:
The recording expands on the topics covered in this article. Experts presenting are Ihsan Oesman, Takeshi Sawaguchi, Michael Schütz, Ismail Hadisoebroto Dilogo, Dwikora Novembri Utomo, and Andito Wibisono.
References:
- Stoffel K, Blauth M, Joeris A, Blumenthal A, Rometsch E. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: a systematic review. Arch Orthop Trauma Surg. 2020 Oct;140(10):1381-1394. doi: 10.1007/s00402-020-03332-7. Epub 2020 Feb 21. PMID: 32086558; PMCID: PMC7505881.
- Gallaghan JJ et al. The adult hip 3rd Ed. 2017. Lippincott Williams Wilkins
- Menken LG, Rodriguez JA. Femoral revision for periprosthetic fracture in total hip arthroplasty. J Clin Orthop Trauma. 2020 Jan-Feb;11(1):16-21. doi: 10.1016/j.jcot.2019.12.003. Epub 2019 Dec 14. PMID: 32001978; PMCID: PMC6985170.
- Menken LG et al., Femoral revision for periprosthetic fracture in total hip arthroplasty. J Clin Orthop. Trauma 2020 Jan-Feb; 11(1):16–21
- Ibid. Menken LG et al.
- Munro JT, Garbuz DS, Masri BA, Duncan CP. Tapered fluted titanium stems in the management of Vancouver B2 and B3 periprosthetic femoral fractures. Clin Orthop Relat Res. 2014 Feb;472(2):590-8. doi: 10.1007/s11999-013-3087-3. PMID: 23719963; PMCID: PMC3890200.
- Moazen M, Mak JH, Etchels LW, Jin Z, Wilcox RK, Jones AC, Tsiridis E. Periprosthetic femoral fracture--a biomechanical comparison between Vancouver type B1 and B2 fixation methods. J Arthroplasty. 2014 Mar;29(3):495-500. doi: 10.1016/j.arth.2013.08.010. Epub 2013 Sep 12. PMID: 24035619.
- Lei PF, Hu RY, Hu YH. Bone Defects in Revision Total Knee Arthroplasty and Management. Orthop Surg. 2019 Feb;11(1):15-24. doi: 10.1111/os.12425. Epub 2019 Feb 27. PMID: 30809942; PMCID: PMC6430493.
- Morgan-Jones R, Oussedik SI, Graichen H, Haddad FS. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015 Feb;97-B(2):147-9. doi: 10.1302/0301-620X.97B2.34144. PMID: 25628273.
- Abbas, Azlina & Merican, Azhar & Mohamad, Jamal. (2007). Morsellized Allograft and Acetabular Reconstruction Cage: Follow-up of 2 to 9 years. Malaysian Orthopaedic Journal. 1. 5-7. 10.5704/MOJ.0705.002.
- Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994 Feb;9(1):33-44. doi: 10.1016/0883-5403(94)90135-x. PMID: 8163974.
- Meneghini RM, Ford KS, McCollough CH, Hanssen AD, Lewallen DG. Bone remodeling around porous metal cementless acetabular components. J Arthroplasty. 2010 Aug;25(5):741-7. doi: 10.1016/j.arth.2009.04.025. Epub 2009 May 26. PMID: 19473807.
- Lee PT, Raz G, Safir OA, Backstein DJ, Gross AE. Long-term results for minor column allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2010 Dec;468(12):3295-303. doi: 10.1007/s11999-010-1591-2. PMID: 20878280; PMCID: PMC2974884.
- Sporer SM. How to do a revision total hip arthroplasty: revision of the acetabulum. J Bone Joint Surg Am. 2011 Jul 20;93(14):1359-66. doi: 10.2106/JBJS.9314icl. PMID: 21792504.
- Landor I, Vavrík P, Jahoda D, Pokorný D, Popelka S, Sosna A. Oblong implants for revision total hip arthroplasty. Acta Chir Orthop Traumatol Cech. 2009;76:462-472. 23.
- Zehntner MK, Ganz R. Midterm results (5.5-10 years) of acetabular allograft reconstruction with the acetabular reinforcement ring during total hip revision. J Arthroplasty. 1994 Oct;9(5):469-79. doi: 10.1016/0883-5403(94)90092-2. PMID: 7807103.
- Kim Y, Tanaka C, Kanoe H. Long-Term Outcome of Acetabular Reconstruction Using a Kerboull-Type Acetabular Reinforcement Device with Hydroxyapetite Granule and Structural Autograft for AAOS type II and III Acetabular Defects. J Arthroplasty. 2015 Oct;30(10):1810-4. doi: 10.1016/j.arth.2015.04.034. Epub 2015 May 6. PMID: 25981327.
- Parvizi, Javad & Gehrke, Thorsten. (2014). Definition of Periprosthetic Joint Infection. The Journal of Arthroplasty. 29. 1331.
- Tsukayama DT, Goldberg VM, Kyle R. Diagnosis and management of infection after total knee arthroplasty. J Bone Joint Surg Am 2003;85-A(Suppl 1):S75-S80
found in:
Gomes LSM. Early Diagnosis of Periprosthetic Joint Infection of the Hip-Current Status, Advances, and Perspectives. Rev Bras Ortop (Sao Paulo). 2019 Jul;54(4):368-376. doi: 10.1055/s-0039-1693138. Epub 2019 Aug 20. PMID: 31435100; PMCID: PMC6701967.
Recommended reading:
- Auñón Á, Coifman I, Blanco A, García Cañete J, Parrón-Cambero R, Esteban J. Usefulness of a Multiplex PCR Assay for the Diagnosis of Prosthetic Joint Infections in the Routine Setting. Orthop Surg. 2022 Feb;14(2):383-388. doi: 10.1111/os.13187. Epub 2022 Jan 2. PMID: 34978153; PMCID: PMC8867406.
https://www.researchgate.net/publication/357529715
You might also be interested in:
AO Trauma Competency-Based Curriculum Courses
Learn more about the AO Trauma’s competency-based curriculum courses and explore our educational events.
Courses and events
Find all upcoming AO Trauma courses and events in your region and worldwide in more than 100 countries.
Videos and webinars
Leading AO Trauma surgeons and our experienced production team produce first-class videos for educational purposes.