AO Trauma Course—Fracture Care in Older Adults
This course is aimed at General trauma surgeons, orthopedic surgeons, geriatricians, and medicine physicians who want to:
- Improve their surgical and medical care of patients with fragility fractures
- Make improvements in their hospital's and department's approach to fracture care in older adults
Participants should be actively involved in fragility fracture care. In addition, surgeon participants should have completed the AO Trauma Courses—Basic Principles and Advanced Principles of Fracture Management.
Participants will learn how the overall care of the fragility fracture patient can be substantially improved. Since the fracture represents only one aspect, orthogeriatric comanagement of the patient from admission to completion of rehabilitation is the optimal approach. This course delivers the latest evidence as well as practical details on the comprehensive management of fragility fractures in older adults, with the aim of changing attitudes and improving the care of this patient group.
Why you should choose this course
Top national, regional, and international faculty
2-3 days in duration
For surgeons who already treat (older adults)
Network with colleagues from all over the world
CME credits
Course content
-
Course modules
Module 1: Preoperative phase
Lectures:
- Principles of comanaged care
- Comorbidity and preoperative optimization
- Functional status, treatment goals, and prognosis
- Anticoagulation
Module 2: Operative phase – Day 1
Lectures:
- Regional versus general anesthesia–does it matter?
- Bleeding (optional)
Case Based discussions:
- Upper extremity
- Proximal humerus
- Around the elbow
- Around the wrist
- Lower extremity
- Femoral neck fractures and per-/subtrochanteric fractures
- Pelvis and acetabulum
- Periprosthetic femur fractures
- Fractures around the knee and ankle
- Principles, typical failures, and solutions
- Sarcopenia, frailty, and nutrition
- Pain medication: Pre and postoperative
- Atypical fractures
Module 3: Operative phase
Lectures:
- Full weight bearing
- Postoperative medical management
- Evaluation and management of falls
- Secondary fracture prevention–case
- Osteoporosis management–treatment algorithm
- Delirium
Module 4: Orthogeriatric co-management
- How to involve your team (what elements do you need and how do you create the optimal team) – stress importance of communication, etc
- What is necessary for efficient smooth implementation (protocols, etc)?
- How to convince your hospital management (resources and to pay for it)?
-
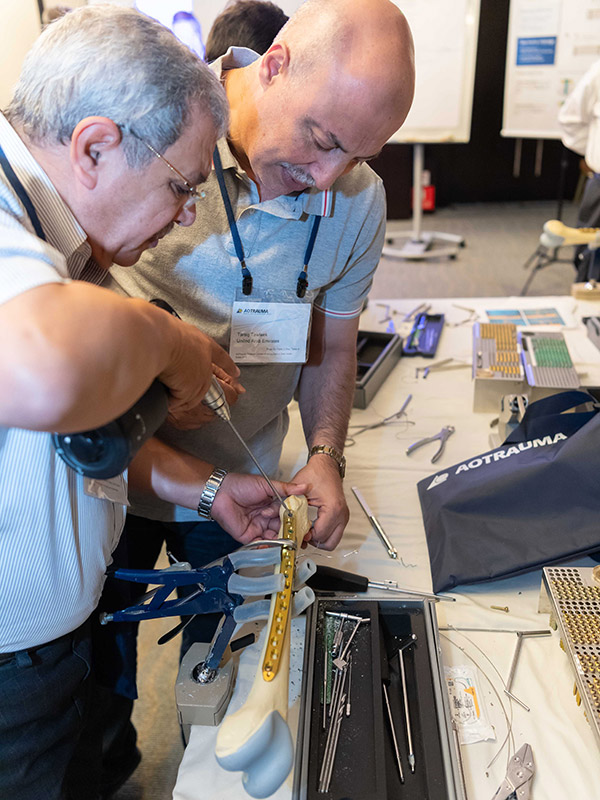
Practical exercises
- Femoral nail with augmentation
- Periprosthetic fracture fixation
Course details may be subject to change. Please check your chosen date and location for the detailed program.
Target audience
- Practicing surgeons in orthopedic trauma, orthopedics, and general trauma
- Geriatricians and other medicine physicians (eg, internal medicine, anesthesiology)
- Residents/trainees (surgical and medical)
Competencies
The education taskforce has identified the following competencies for this area of practice:
- Correctly fix fragility fractures as indicated
- Adapt treatment in line with aging
- Recognize comorbidities and polypharmacy
- Prevent, identify, and treat complications
- Address secondary prevention (osteoporosis, falls)
- Restore function early
- Apply the basic science of fixation and bone biology
- Initiate and comanage patient care with the healthcare team
- Build a system of care for fragility fractures
- Seek to restore and preserve functionality, independence, and quality of life
What does competency-based curriculum development mean?
Resources
Orthogeriatrics Mobile App
Discover this educational tool for health-care professionals managing older adults with fragility fractures.
AO Surgery Reference
Explore the award-winning online repository for surgical knowledge, describing the complete management process from diagnosis to aftercare for fractures in a given anatomical region.
Orthogeriatrics education taskforce

Hala Samir Sweed (Egypt)
Term: 2026

Theo Tosounidis (Greece)
Term: 2025–2026

Radwan G Metwaly (Egypt)
Term: 2025–2026
See a full list of all regional program contributors and past international program editors.
Not the right course?
Find our list of all curricula courses here.