Evaluation of neurologic complications in adult spinal deformity surgery

The AO Spine Knowledge Forum Deformity recently concluded its landmark study, Evaluation of Neurologic Complications Associated with Surgical Correction of Adult Spinal Deformity (Scoli-RISK). “This study has significantly advanced the understanding of motor neurologic outcomes in complex adult spinal deformity (ASD) surgery, establishing the gold standard for the rate of neurologic complications,” said Principal Investigator Lawrence Lenke.
This AO Spine-sponsored study is executed with support from AO Clinical Evidence (AO CE).
ClinicalTrials.gov Identifier: NCT02949245
-
Read the quick summary:
- The award-winning Scoli-RISK study analyzed neurologic complications in adult spinal deformity surgery, identifying risk factors and long-term patient outcomes.
- Neurologic complications can persist post-surgery; long-term monitoring, surgical refinements, and standardized global practices are crucial for better outcomes.
- Implement risk stratification, enhance surgical techniques, improve postoperative care, and establish global guidelines to reduce complications and improve safety.
The award-winning, multicenter, prospective study that partnered with the Scoliosis Research Society (SRS) aimed to establish the risk of neurologic deficit related to surgical correction of adult spinal deformity and to identify characteristics associated with increased risk of neurologic complications related to the surgery. According to Co-principal Investigator Michael Fehlings “Researchers and clinicians will now continue to build upon its findings, refining techniques and developing innovative strategies to reduce risk and improve patient outcomes.”
Final publication: five-year follow-up outcomes
The latest and final publication from the Scoli-RISK study, titled ‘Long-term follow-up of non-neurologic and neurologic complications after complex adult spinal deformity surgery: results from the Scoli-RISK-1 study’, was published in the European Spine Journal. This publication focused on the five-year follow-up data, detailing long-term adverse events and patient-reported outcomes.
The findings reinforce the importance of continued surveillance of patients beyond the early postoperative period. While immediate complications are often the focus of surgical literature, this study demonstrated that neurologic issues and other complications may manifest or persist years after surgery, necessitating a paradigm shift in postoperative care strategies.
A landmark study in ASD surgery from the AO
The Scoli-RISK study stands out for its extensive scale and rigorous methodology. 272 patients were enrolled from 15 centers across three continents, making it one of the most comprehensive investigations into neurologic complications following ASD surgery. The study followed patients for five years postoperatively, providing invaluable long-term data on outcomes, complications, and patient-reported quality of life measures.
Through its findings, the study has had a profound impact on surgical practices and contributed significantly to the body of knowledge surrounding complex spinal deformity procedures. With 18 peer-reviewed publications and 70 conference presentations, the study has become a cornerstone in ASD surgical research.
Key findings: risk factors and long-term outcomes
One of the most significant contributions of the Scoli-RISK study has been the identification of key risk factors for poor surgical outcomes. These include patient-specific elements such as age, comorbidities, and baseline neurological status, as well as surgical factors like operative time, blood loss, and the extent of spinal correction performed.
Among the study’s notable conclusions was the impact of mechanical complications on long-term outcomes. The findings highlighted how instrumentation failure, implant-related complications, and the necessity for revision surgeries could directly influence neurologic function and overall patient satisfaction. This underscores the need for improved mechanical stabilization strategies and reinforces the importance of careful surgical planning to mitigate these risks.
Regional variations highlight the need for standardization
The Scoli-RISK study revealed regional variations in outcomes and treatment protocols. Across different centers and continents, disparities were noted in surgical approaches, postoperative care, and complication rates.
These regional variations emphasize the need for greater standardization in surgical practices for ASD correction. By harmonizing best practices globally, the study suggests that surgeons can minimize neurologic complications and improve overall patient safety and satisfaction.
The role of Patient-Reported Outcome Measures (PROMS)
A critical takeaway from the Scoli-RISK study is the importance of patient-reported outcome measures (PROMs) in long-term follow-up. Traditional surgical success metrics often focus on radiographic correction and immediate postoperative outcomes. However, Scoli-RISK reinforces the value of longitudinal patient feedback on pain levels, functional improvement, and quality of life.
By utilizing PROMs, Scoli-RISK was able to capture the full spectrum of patient experiences, revealing insights into how neurologic complications affect daily life beyond clinical assessments. This patient-centered approach is essential in shaping future ASD treatment protocols and ensuring that success is defined not just by surgical precision, but by tangible, long-term patient benefits.
Implications for future clinical practice
The Scoli-RISK study has laid the groundwork for future research and clinical improvements in ASD surgery. Among its most pressing implications are:
- Preoperative risk stratification: The study reinforces the need for comprehensive risk assessments before surgery. Measures such as advanced imaging, neuromonitoring strategies, and predictive analytics can help anticipate and mitigate complications.
- Surgical technique optimization: Given the mechanical complications identified, the study highlights the necessity of adopting innovative fixation strategies and biomechanical reinforcement techniques to improve construct durability.
- Enhanced postoperative monitoring: The five-year data underscores that patient care must extend well beyond the initial postoperative period. Standardizing long-term follow-up with both clinical assessments and PROMs is essential for ensuring continued patient well-being.
- Global standardization efforts: The study’s identification of regional variations signals the need for international consensus guidelines to unify best practices and improve patient safety worldwide.
- Focus on preventative measures: With neurologic complications being a major concern, proactive strategies such as intraoperative neuromonitoring, targeted rehabilitation, and early intervention protocols should be prioritized in surgical planning.
Looking forward
The Scoli-RISK study is clearly one of the most significant contributions to ASD surgical literature in recent years and has set a new benchmark for evaluating neurologic complications in spinal deformity surgery.
With its vast dataset and impactful insights, this study will serve as a foundation for future advancements in spinal deformity correction. The hope is that by integrating these findings into everyday clinical practice, the global surgical spine community can enhance safety, reduce complications, and ultimately improve the lives of patients undergoing complex spinal deformity surgeries.
List of publications from the Scoli-RISK study
Cerpa, M., Zuckerman, S. L., Lenke, L. G., Carreon, L. Y., Cheung, K., Kelly, M. P., ... & Shaffrey, C. I. (2025). Long-term follow-up of non‑neurologic and neurologic complications after complex adult spinal deformity surgery: results from the Scoli-RISK-1 study. European Spine Journal, 1-11.
Jiang, F., Joshi, H., Badhiwala, J. H., Wilson, J. R., Lenke, L. G., Shaffrey, C. I., ... & Fehlings, M. G. (2024). Spinal cord injury in high-risk complex adult spinal deformity surgery: review of incidence and outcomes from the Scoli-RISK-1 study. Spinal cord series and cases, 10(1), 59.
S. L. Zuckerman, M. Cerpa, L. G. Lenke, C. I. Shaffrey, L. Y. Carreon, K. M. C. Cheung, M. P. Kelly, M. G. Fehlings, C. P. Ames, O. Boachie-Adjei, M. B. Dekutoski, K. M. Kabeaish, S. J. Lewis, Y. Matsuyama, F. Pellisé, Y. Qiu, F. J. Schwab and J. S. Smith. Patient-Reported Outcomes After Complex Adult Spinal Deformity Surgery: 5-Year Results of the Scoli-Risk-1 Study. Global Spine J 2192568220988276, 2021
L. G. Lenke, S. L. Zuckerman, M. Cerpa, C. I. Shaffrey, L. Y. Carreon, K. M. C. Cheung, M. P. Kelly, M. G. Fehlings, C. P. Ames, O. Boachie-Adjei, M. B. Dekutoski, K. M. Kebaish, S. J. Lewis, Y. Matsuyama, F. Pellise, Y. Qiu, F. J. Schwab, J. S. Smith, AO Spine Knowledge Forum Deformity and SRS Scoli-RISK-1 Study Group. The Scoli-RISK 1 results of lower extremity motor function 5 years after complex adult spinal deformity surgery. Eur Spine J 30 (11): 3243-3254, 2021
Shimizu, T., Lenke, L. G., Cerpa, M., Beauchamp, E. C., Carreon, L. Y., Shaffrey, C. I., ... & Fehlings, M. G. (2020). A radiographic analysis of lumbar fusion status and instrumentation failure after complex adult spinal deformity surgery with spinopelvic fixation: two-year follow-up from the Scoli-Risk-1 prospective database. Clinical spine surgery, 33(10), E545-E552.
J. R. F. Wilson, F. Jiang, J. H. Badhiwala, C. I. Shaffrey, L. Y. Carreon, K. M. C. Cheung, B. T. Dahl, C. P. Ames, O. Boachie-Adjei, M. B. Dekutoski, S. J. Lewis, Y. Matsuyama, H. Mehdian, F. Pellise, Y. Qiu, F. J. Schwab, L. G. Lenke and M. G. Fehlings. The Effect of Tobacco Smoking on Adverse Events Following Adult Complex Deformity Surgery: Analysis of 270 Patients From the Prospective, Multicenter Scoli-RISK-1 Study. Spine (Phila Pa 1976) 45 (1): 32-37, 2020
R. Saigal, D. Lau, S. H. Berven, L. Carreon, M. B. Dekutoski, K. M. Kebaish, Y. Qiu, Y. Matsuyama, M. Kelly, B. T. Dahl, H. Mehdian, F. Pellisé, S. J. Lewis, K. M. Cheung, C. I. Shaffrey, M. G. Fehlings, L. G. Lenke and C. P. Ames. Impact of New Motor Deficit on HRQOL after Adult Spinal Deformity Surgery: Subanalysis from Scoli Risk 1 Prospective Study. Spine (Phila Pa 1976) 46 2020
K. Kwan, H. Yat Hong, L. Lenke, et al. Are Higher Global Alignment and Proportion Scores Associated With Increased Risks of Mechanical Complications After Adult Spinal Deformity Surgery? An External Validation. Clinical Orthopaedics and Related Research 479(2):p 312-320, February 2021
Tuchman, L. G. Lenke, M. Cerpa, M. G. Fehlings, S. J. Lewis, C. I. Shaffrey, K. M. C. Cheung, L. Y. Carreon, M. B. Dekutoski, F. J. Schwab, O. Boachie-Adjei, K. Kebaish, C. P. Ames, Y. Qiu, Y. Matsuyama, B. T. Dahl, H. Mehdian, F. Pellise and S. H. Berven. Unilateral versus bilateral lower extremity motor deficit following complex adult spinal deformity surgery: is there a difference in recovery up to 2-year follow-up? Spine Journal 19 (3): 395-402, 2019
K. Y. H. Kwan, C. Bow, D. Samartzis, L. G. Lenke, C. I. Shaffrey, L. Y. Carreon, B. T. Dahl, M. G. Fehlings, C. P. Ames, O. Boachie-Adjei, M. B. Dekutoski, K. M. Kebaish, S. J. Lewis, Y. Matsuyama, H. Mehdian, F. Pellise, Y. Qiu, F. J. Schwab and K. M. C. Cheung. Non-neurologic adverse events after complex adult spinal deformity surgery: results from the prospective, multicenter Scoli-RISK-1 study. Eur Spine Journal 28 (1): 170-179, 2019
Meghan Cerpa, Lawrence G. Lenke, Michael G. Fehlings, Christopher I. Shaffrey, Kenneth MC Cheung and Leah Yacat Carreon. Evolution and Advancement of Adult Spinal Deformity Research and Clinical Care: An Overview of the Scoli-RISK-1 Study. Global Spine Journal 9 (1S): 8-14, 2019
E. K. Miller, L. G. Lenke, B. J. Neuman, D. M. Sciubba, K. M. Kebaish, J. S. Smith, Y. Qiu, B. T. Dahl, F. Pellise, Y. Matsuyama, L. Y. Carreon, M. G. Fehlings, K. M. Cheung, S. Lewis, M. B. Dekutoski, F. J. Schwab, O. Boachie-Adjei, H. Mehdian, S. Bess, C. I. Shaffrey, C. P. Ames, AOSpine Knowledge Forum Deformity and International Spine Study Group. External Validation of the Adult Spinal Deformity (ASD) Frailty Index (ASD-FI) in the Scoli-RISK-1 Patient Database. Spine (Phila Pa 1976) 43 (20): 1426-1431, 2018
L. G. Lenke, C. I. Shaffrey, L. Y. Carreon, K. M. C. Cheung, B. T. Dahl, M. G. Fehlings, C. P. Ames, O. Boachie-Adjei, M. B. Dekutoski, K. M. Kebaish, S. J. Lewis, Y. Matsuyama, H. Mehdian, F. Pellise, Y. Qiu, F. J. Schwab and AOSpine International and SRS Scoli-RISK-1 Study Group. Lower Extremity Motor Function Following Complex Adult Spinal Deformity Surgery: Two-Year Follow-up in the Scoli-RISK-1 Prospective, Multicenter, International Study. J Bone Joint Surg Am 100 (8): 656-665, 2018
S. Kato, M. G. Fehlings, S. J. Lewis, L. G. Lenke, C. I. Shaffrey, K. M. C. Cheung, L. Y. Carreon, M. B. Dekutoski, F. J. Schwab, O. Boachie-Adjei, K. M. Kebaish, C. P. Ames, Y. Qiu, Y. Matsuyama, B. T. Dahl, H. Mehdian, F. Pellise and S. H. Berven. An Analysis of the Incidence and Outcomes of Major Versus Minor Neurological Decline After Complex Adult Spinal Deformity Surgery: A Subanalysis of Scoli-RISK-1 Study. Spine (Phila Pa 1976) 43 (13): 905-912, 2018
M. G. Fehlings, S. Kato, L. G. Lenke, H. Nakashima, N. Nagoshi, C. I. Shaffrey, K. M. C. Cheung, L. Carreon, M. B. Dekutoski, F. J. Schwab, O. Boachie-Adjei, K. M. Kebaish, C. P. Ames, Y. Qiu, Y. Matsuyama, B. T. Dahl, H. Mehdian, F. Pellise-Urquiza, S. J. Lewis and S. H. Berven. Incidence and risk factors of postoperative neurologic decline after complex adult spinal deformity surgery: results of the Scoli-RISK-1 study. Spine Journal 18 (10): 1733-1740, 2018
M. P. Kelly, L. G. Lenke, J. Godzik, F. Pellise, C. I. Shaffrey, J. S. Smith, S. J. Lewis, C. P. Ames, L. Y. Carreon, M. G. Fehlings, F. Schwab and A. L. Shimer. Retrospective analysis underestimates neurological deficits in complex spinal deformity surgery: a Scoli-RISK-1 Study. J Neurosurg Spine 27 (1): 68-73, 2017
L. Y. Carreon, S. D. Glassman, C. I. Shaffrey, M. G. Fehlings, B. Dahl, C. P. Ames, Y. Matsuyama, Y. Qiu, H. Mehdian, K. M. Cheung, F. J. Schwab, F. Pellise, K. M. Kebaish and L. G. Lenke. Predictors of Health-Related Quality-of-Life After Complex Adult Spinal Deformity Surgery: A Scoli-RISK-1 Secondary Analysis. Spine Deformity 5 (2): 139-144, 2017
L. G. Lenke, M. G. Fehlings, C. I. Shaffrey, K. M. Cheung, L. Carreon, M. B. Dekutoski, F. J. Schwab, O. Boachie-Adjei, K. M. Kebaish, C. P. Ames, Y. Qiu, Y. Matsuyama, B. T. Dahl, H. Mehdian, F. Pellise-Urquiza, S. J. Lewis and S. H. Berven. Neurologic outcomes of complex adult spinal deformity surgery: results of the prospective, multicenter Scoli-Risk 1 study. Spine (Phila Pa 1976) 41 (3): 204-12, 2016
Be the first to know about new AO Spine content and updates
Sign up for the AO Spine newsletter
You might also be interested in:
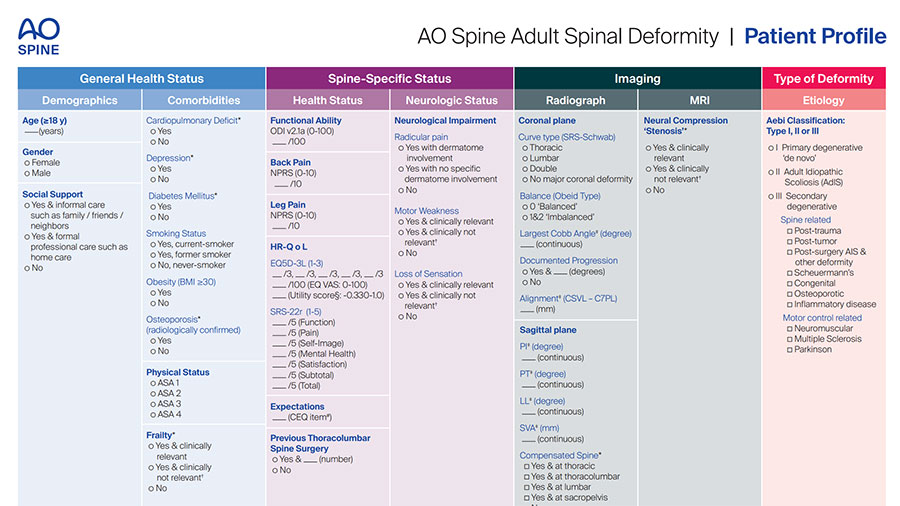
AO Spine Adult Spine Deformity (AO ASD) Patient Profile
The AO ASD Patient Profile provides an overview that allows physicians to systematically consider the factors that could contribute to optimal management of the condition.
AO Surgery Reference Deformity modules
AO Surgery Reference (AO SR) is a resource for the management of fractures and musculoskeletal disease, based on current clinical principles, practices, and available evidence.
AO Spine deformity courses and Global Spine Diploma modules
Developed and taught by world-leading deformity experts, based on latest evidence, providing skills that spine surgeons need for the future.
AO Spine Research programs
AO Spine sponsors innovative studies adhering to the highest standards. We generate knowledge that matters to our members and to our patients.