New research toolkit will change the way research on Degenerative Cervical Myelopathy (DCM) is conducted

Selecting the right tools for a job is equally important in medicine as in any other field. The AO Spine Knowledge Forum Spinal Cord Injury (KF SCI) has created a toolkit to equip scientists and help make DCM studies robust, comparable, and focused on the most relevant open questions. One of the KF SCI symposia at the GSC in Prague will present the toolkit, focusing on current concepts and future perspectives of DCM.
The symposium will be moderated by Michael Fehlings and Mark Kotter, both long-time key drivers of AO Spine research. They will address areas of unmet needs, best management for patients with asymptomatic spinal cord compression, and principles around surgical decision-making.
According to Benjamin Davies, co-principal investigator of the AO Spine RECODE-DCM study, “the DCM research community is small, fragmented, and lacking diversity. There is little synergy with researchers working in isolation. Collaboration is a cornerstone of scientific progress, but in DCM, researchers seldom collaborate across borders.”
Accelerating degenerative cervical myelopathy research progress and guidelines for SCI
The AO Spine KF SCI identified the need early on, and under the leadership of Michael Fehlings a combined set of Clinical Practice Guidelines for the management of DCM and Acute Traumatic Spinal Cord Injury was published in the Global Spine Journal in 2017. (Guidelines are periodically reviewed, and the updated Guidelines on traumatic SCI will be published later this year. The latest knowledge is also an upcoming GSC symposia title.)
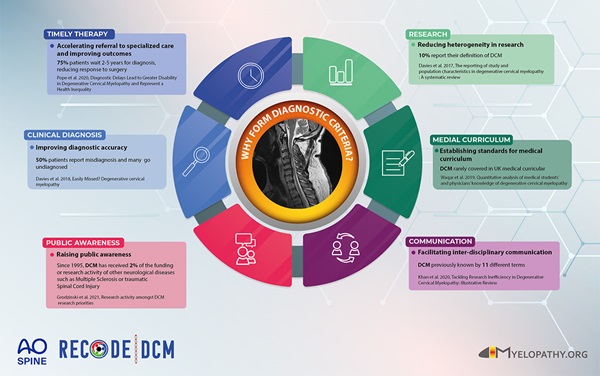
Two years later, the collaborative RECODE-DCM initiative was launched with Myelopathy.org to standardize and synergize researchers' work for faster and more efficient global progress. The newly established minimum dataset, in combination with the top ten priorities and a definition for the index term, can accelerate research findings and improve outcomes that matter most to all stakeholders.
What’s inside the DCM Research Toolkit:
- The Top 10 Research Priorities: the most important questions to tackle and what researchers should focus on to address problems that matter most to people living with, treating, or otherwise affected by DCM.
- The Minimum Dataset: the data points that will ensure researchers measure consistent data points across the globe. The measurement includes minimum core data elements, core outcome set, and the tools to measure the outcomes without burdening the researchers and patients.
- The Index Term and Definition: From the many different terms that have been used to name this condition, the international community selected Degenerative Cervical Myelopathy (DCM). A definition of the condition can be registered in international disease classifications.
Measuring what matters for DCM research
The toolkit development process used a range of methods—systematic reviews, qualitative interviews, and the James Lind Alliance (JLA) priority setting process (PSP)—bringing together the perspectives of a diverse community of stakeholders with lived and/or professional experience of DCM. The global collaborative included surgeons, physiotherapists, neurologists, primary care doctors, people living with DCM, and people caring for people with DCM, allowing input from as many different angles as possible.
The PSP allowed the group to distill and rank the critical research questions. The minimum dataset was established by identifying the disease outcomes at the core of DCM, including outcomes that are sometimes overlooked by healthcare professionals, such as pain and life-impact, but which are the number one recovery priorities for individuals living with DCM.
Also, core data elements, such as demographic factors that can clarify the disease picture, are necessary components of the toolkit. All potential measurement instruments were reviewed, and four tools were selected based on quality, popularity, feasibility to use, and relevance to the core outcomes for both clinicians and patients:
- The modified Japanese Orthopaedic Scale (mJOA)
- The SF-36 Life Impact Scale
- The Neck Disability Index
- The Spinal Adverse Events Severity System
The index term and definition were agreed through an international survey and a multidisciplinary expert consensus meeting. Historically, DCM has gone by many names, such as Cervical Stenosis and Spondylotic Myelopathy, making it difficult to synthesize literature or compare data. Standardized terminology will enhance knowledge translation when all stakeholders speak a common language, and the aim is to create a disease code for Degenerative Cervical Myelopathy.
DCM is much more prevalent than thought, but new research can make a difference
The AO Spine RECODE-DCM Steering Committee now urges researchers and funders to dive into exploring the knowledge gaps in DCM to accelerate the progress in practice.
According to Mark Kotter, principal investigator of AO Spine RECODE-DCM, DCM is the Number 1 cause of chronic spinal cord injury in adults, with some of the worst SF-36 scores measured in the literature. "We need to take it seriously. It is much more prevalent than we thought. But surgery can make a difference, especially if we catch it early.”
Fehlings warns that the estimated 2% of over 40-year-olds with a diagnosis of DCM today is just the tip of the iceberg, particularly in our aging population. “In many people, it can just creep up on them, and it can result in very significant impairment. Often the diagnosis is delayed and not made until people have had significant damage to neurological tissues and very significant issues affecting mobility, walking, hand function, even bowel and bladder control.”
“This new toolkit tells you, as a minimum, what should be in your battery of tests when you’re conducting your research,” Davies continues. "With the current [low] levels of funding for DCM and the many knowledge gaps that were identified, efficiency is necessary." Statistical tests can be powered up when reliable datasets are collated. And when investigating different treatments or studying longitudinal data, robust data can be contrasted unconfounded by variability.
DCM is an under-researched condition, and the AO Spine hopes to inspire a new generation of spine researchers to coalesce around the AO Spine RECODE-DCM initiative and implement the standardized research toolkit. Stimulation of research activity will attract more capital, with funding bodies confident the studies they support are robust, reliable, and relevant to the entire DCM community.
The RECODE-DCM Steering Committee also sees this as an opportunity to bring people together globally, to create important synergies. “If you want to go fast, go alone. If you want to go far, go together,” Davies concludes.
You might also be interested in:
AO Spine KF symposia at the GSC
AO Spine Knowledge Forums will moderate multiple symposia and share their latest knowledge at the GSC.
AO Spine RECODE-DCM
Watch the latest videos and find all the details of the study and its outcomes.
AO Spine Knowledge Forum Spinal Cord Injury
Building on worldwide research partnerships for global impact.
Innovation in spine surgery
Ben Davies considers the role of diversity in developing and applying new approaches as a part of a surgeon's role with the example of DCM.