How to apply molecular prognostication in spine oncology in clinical practice
BY DR RAPHAELE CHAREST-MORIN AND DR C. RORY GOODWIN
Over the last two decades, the outlook for patients with metastatic spine disease has undergone a transformation. While advancements in surgical techniques and stereotactic body radiation therapy (SBRT) have certainly played a role, the real game-changer is the rise of molecular profiling and targeted systemic therapies.
-
Read the quick summary:
- Advancements in molecular prognostication have improved survival for metastatic spine disease patients through molecular prognostication and targeted therapies.
- Key molecular markers EGFR, HER2, and BRAF mutations improve survival rates in lung, breast, and melanoma cancers with targeted therapies.
- Clinical practice integration of the NOMS framework enhances decision-making by incorporating molecular markers and targeted therapies.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
As spine surgeons, our role in these cases expands beyond mechanical stabilization and decompression. We're expected to navigate a landscape where genomics, targeted drugs, and immune therapies significantly influence prognosis, response to treatment, and ultimately, the decision to operate. Understanding the molecular nuances of common tumors like lung, breast, prostate, and melanoma is quickly becoming essential in day-to-day surgical planning.
In this blog post, we aim to walk you through some key points on how to incorporate molecular insights into your clinical practice and surgical decision-making for patients with metastatic spine disease, as well as to provide a good overview of the clinical applications of the latest advancements.
Goodwin CR, De la Garza Ramos R, Bettegowda C, et al. Overview of Molecular Prognostication for Common Solid Tumor Histologies – What the Surgeon Should Know. Global Spine Journal. 2025;15(1_suppl):6S-15S
Understanding molecular markers and targeted therapies
Molecular markers and targeted therapies have revolutionized the treatment of cancer patients, particularly those with metastatic spine disease. These advancements have provided a framework for incorporating molecular prognostication into clinical decision-making, allowing for more personalized and effective treatment plans.
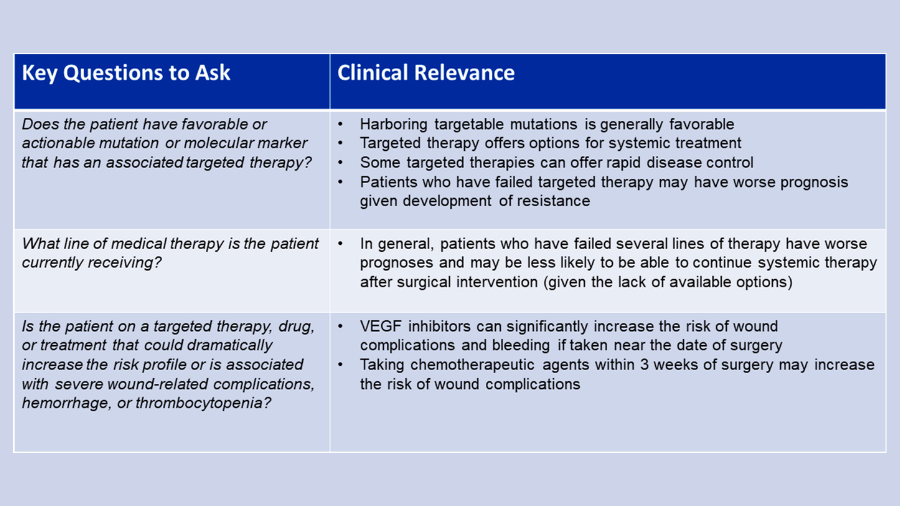
To make this integration practical, consider asking yourself these three questions when evaluating a patient:
- Does the patient have a favorable or actionable molecular marker?
- What line of medical therapy are they on (i.e., newly diagnosed or on their fourth regimen)?
- Is the current treatment associated with high surgical risk (e.g., wound complications from bevacizumab)?
These considerations can help better gauge the likely benefits and risks of surgical intervention.
Key molecular markers and their clinical implications
-
Lung cancer: Lung cancer is a leading cause of cancer-related deaths worldwide. Molecular markers such as EGFR mutations have been shown to significantly improve survival rates for patients with metastatic spine disease. Targeted therapies like erlotinib, gefitinib, and osimertinib have dramatically improved median survival rates for patients with these mutations.
-
Breast cancer: Breast cancer frequently metastasizes to the bone, including the spine. HER2-positive breast cancer patients have benefited from targeted therapies like trastuzumab, which has significantly improved progression-free and overall survival. Additionally, ER-positive tumors can develop resistance to endocrine therapy, but targeted inhibitors like palbociclib have shown promise in extending progression-free survival.
-
Prostate cancer: The spine is a common site for prostate cancer metastases. Androgen deprivation targeted therapies (ADT) have been the cornerstone of treatment for decades. Recent advancements in targeted therapies, such as cabozantinib and olaparib, have shown promise in improving outcomes for patients with metastatic prostate cancer.
-
Melanoma: Metastatic melanoma has historically been associated with poor survival rates. However, targeted therapies like BRAF inhibitors (vemurafenib, dabrafenib) have shown significant improvements in progression-free and overall survival for patients with BRAF mutations.
Incorporating molecular prognostication into clinical practice
The NOMS framework—now with molecular intelligence
The NOMS (Neurologic, Oncologic, Mechanical, Systemic) framework is a widely accepted decision-making algorithm for managing spinal metastases and many of us use it to guide decisions about metastatic spine disease. Historically, the "O" stood for radiation sensitivity, but that’s no longer enough. Oncologic assessment must now include responsiveness to targeted therapies and immunotherapies.
Incorporating molecular markers and targeted therapies into this framework can enhance clinical decision-making and improve patient outcomes. For instance, understanding a patient's molecular profile can help determine the most appropriate surgical intervention and postoperative treatment plan.
Case Examples
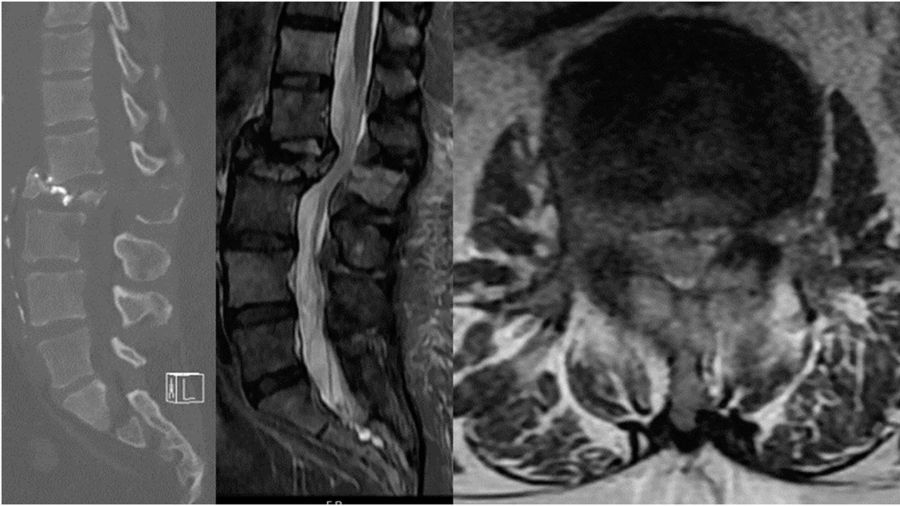
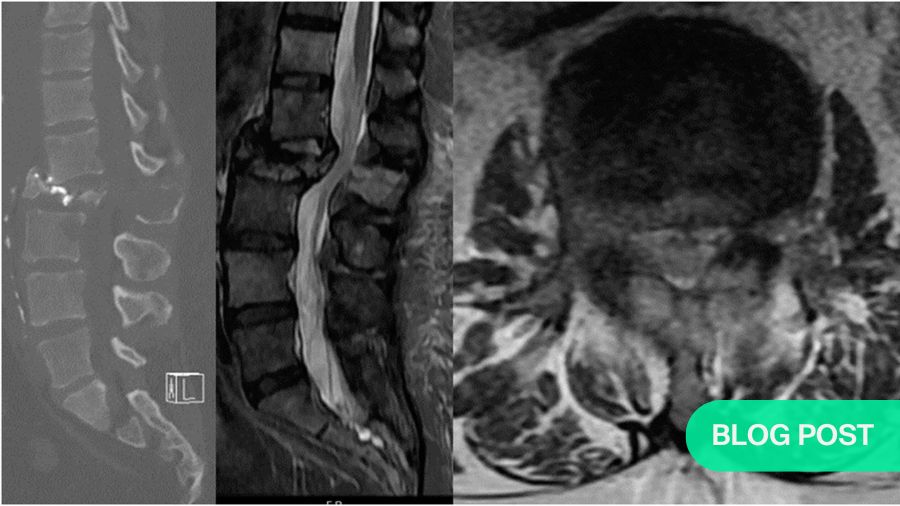
Case 1: A 46-year-old man presents with 3 months of weight loss, back pain, and cough. He is a non-smoker.
Chest imaging reveals a lung nodule consistent with NSCLC (adenocarcinoma) and molecular analysis reveals an EGFR mutation. There is a single metastatic lesion at L2 causing a pathologic fracture with greater than 50% loss of height and retropulsion. He is ambulatory and has pain-limited weakness 4/5 on the hip flexor. He has good performance status (ECOG 1) and his Spine Instability Neoplastic Score is 17. Given the recent diagnosis of NSCLC and the favorable EGFR mutation, patient is started on osimertinib and offered separation surgery plus stabilization.
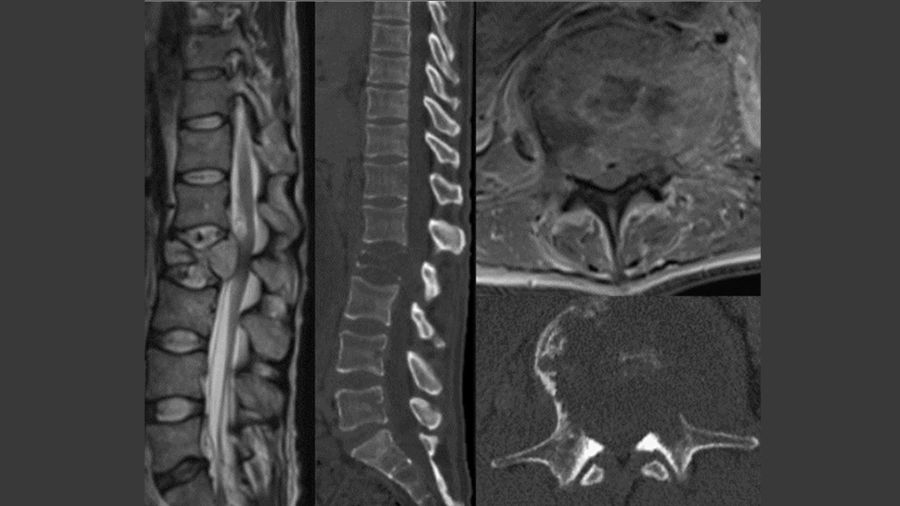
Case 2: A 71-year-old man presents with one week of back pain.
He was diagnosed 5 months ago with NSLC adeno-carcinoma also with an EGFR mutation and started on osimertinib. He has progressed through targeted therapy and recently started chemotherapy.
One month ago, he was found to have metastases to the liver and pelvis and was started on pembrolizumab/ carboplatin/ pemetrexed. He is now found to have an L2 pathologic fracture with retropulsion. He is ambulatory and full strength. His ECOG performance status is 2 and his SINS is 15. The patient seems to have progressed through targeted therapy but just started chemotherapy recently, which still leaves room for further systemic options.
Patient is offered separation surgery plus stabilization.
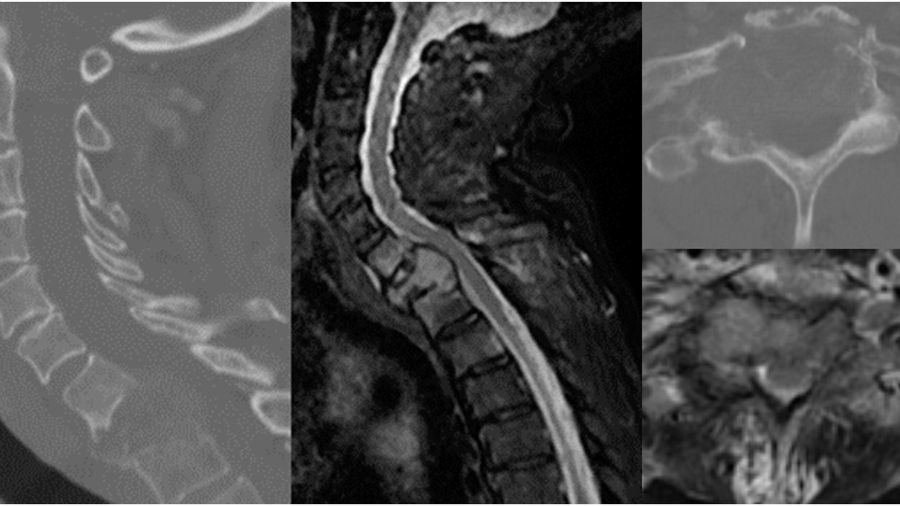
Case 3: A 60-year-old man with advanced NSCLC and no favorable mutations presents with multiple metastases, severe myelopathy, and 3 weeks of severe neck pain and gait instability, which has resulted in him spending most time in bed.
Given his poor prognosis and lack of systemic treatment options, he is palliated with best supportive care.
He has been previously treated with several lines of therapy including osimertinib, pembrolizumab/ carboplatin/pemetrexed, docetaxel, and gemcitabine. He is found to have multiple lung nodules consistent with NSCLC (adenocarcinoma) and molecular analysis reveals no favorable mutation after testing for EGFR, ALK, BRAF, and KRAS. He has metastases to liver, lymph nodes, adrenal glands, pelvis, and spine. He has a T1 pathologic fracture with high-grade cord compression; on exam he is 4+/5 strength but severely myelo- pathic. His ECOG performance status is 4 and SINS 15.
This patient does not harbor any favorable mutation for targeted therapy and is already presenting with advanced disease. Medical Oncology does not consider him a candidate for systemic treatment currently.
Patient is not offered surgery and palliated with best supportive care.
Conclusion
The integration of molecular markers and targeted therapies into clinical practice has significantly improved the survival and quality of life for patients with metastatic spine disease. By incorporating these advancements into decision-making frameworks like NOMS, clinicians can provide more personalized and effective treatment plans, ultimately leading to better patient outcomes.
As these therapies continue to evolve, they offer hope for improved survival rates and quality of life for patients with metastatic spine disease. The ongoing advancements in targeted therapies, such as EGFR inhibitors for lung cancer and BRAF inhibitors for melanoma, demonstrate significant progress in managing metastatic spine disease. As we continue to research and develop this field, we can expect further breakthroughs that will refine and expand the clinical applications of these therapies, ultimately leading to better patient outcomes.
For a more detailed understanding and for tumor-specific highlights for spine surgeons, access the full article through PubMed: PMID: 39801124.
About the authors:
Dr Raphaële Charest-Morin, MD, FRCSC, is a spine surgeon in practicing in the Vancouver Spine Surgery Institute. Her current practice focuses on adult spine surgery with a sub-specialty interest in spinal oncology and frailty. She is an active member of the AO Spine Knowledge Forum Tumor working to advance patient care and treatment for patients with both metastatic and primary spine tumors which is one of her primary research interests.
Dr Charest-Morin’s reputation for clinical excellence has made her a popular and in-demand presenter at international spine conferences. In addition, she is a member of the Canadian Spine Society, AO Spine North America, and a clinical assistant professor in the Department of Orthopaedics at the University of British Columbia.
Dr C. Rory Goodwin is the Director for Spinal Oncology, Surgical Director for the Duke Center for Brain and Spine Metastasis, Associate Residency Program Director, and an Associate Professor of Neurosurgery, Radiation Oncology and Orthopaedic Surgery at the Duke University Medical Center. He has a clinical research interest in surgical decision-making and algorithms to predict clinical outcomes for patients diagnosed with spinal tumors, and a basic science interest in genomic and proteomic mediators of primary and metastatic spine tumor formation and progression.
Dr Goodwin has over 280 peer-reviewed manuscripts as well over 300 conference abstracts and presentations.
References and further reading:
- Global Spine Journal Special Issue: Precision Medicine in Spinal Oncology by the AO Spine Knowledge Forum Tumor, GSJ. 2025;15(1S)
- Goodwin CR, De la Garza Ramos R, Bettegowda C, et al. Overview of Molecular Prognostication for Common Solid Tumor Histologies – What the Surgeon Should Know. Global Spine Journal. 2025;15(1_suppl):6S-15S
- AO Spine Knowledge Forum Clinical Recommendations special collection in the Global Spine Journal
You might also be interested in:
Precision medicine in spinal oncology
The 2025 Focus Issue from the AO Spine Knowledge Forum Tumor explores in detail the current state of Precision Medicine in Spinal Oncology.
Video lectures by KF Tumor
A series of recorded lectures from the world’s leading experts in the treatment and research of spine tumors.
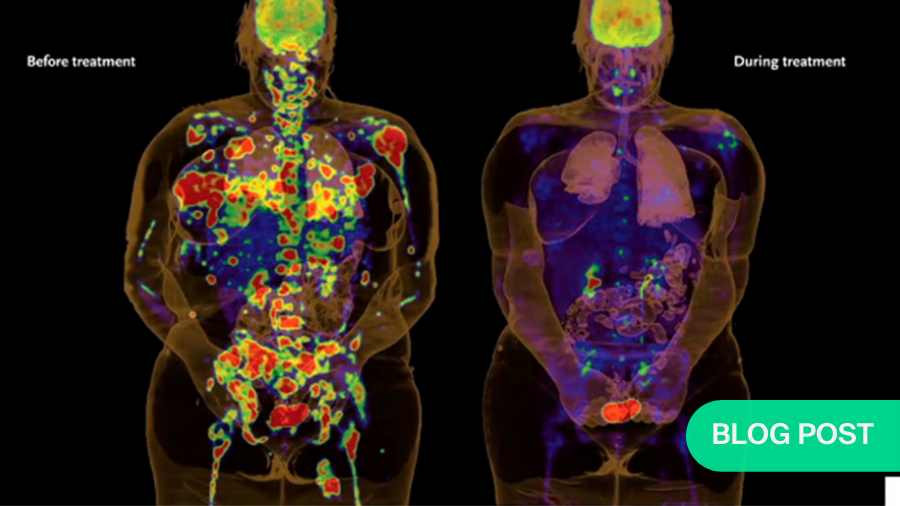
Targeted therapies in cancer treatment
Explore the a brave new world of targeted therapies and how they have vastly improved prognosis in cancer treatment with Dr Chetan Bettegowda.
AO Spine Guest Blog
Read or submit your own guest blog post on spinal tumors or any interesting aspects in spine care and spine surgeons' lives.