The artful dodger: capturing elusive spinal tuberculosis aka Potts disease
BY PROF ALPASLAN ŞENKÖYLÜ
Spinal tuberculosis (TB) can be devastating if left unchecked, but its ability to mimic other diseases makes early detection challenging. Here, Dr Alpaslan Şenköylü explains the increased incidence of spinal TB, outlines diagnostic clues, patient risk factors, and sets out the treatment options that can prevent and correct spine deformity. Early intervention may avoid surgery and disability.
-
Read the quick summary:
- Professor Şenköylü highlights the rising incidence of spinal tuberculosis, its deceptive clinical presentation, and contrasts modern and historical treatment strategies.
- Early detection of spinal tuberculosis is critical; MRI with contrast is a key diagnostic tool, and titanium implants now offer a safer alternative to traditional structural grafts.
- The information supports clinicians in distinguishing spinal TB from tumors or other infections and provides guidance on imaging, patient risk factors, and surgical interventions.
- There is a pressing need for earlier recognition of spinal TB, and ongoing discussions focus on refining global treatment practices and improving access for high-risk and underserved populations.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Spinal tuberculosis—or Potts disease—is an interesting disease because it is both very fragile and very good at hiding its tracks. Often, patients will present at a clinic with symptoms such as back pain and night fever, but of course these symptoms are common across many other diseases too. Spinal tuberculosis often forms a ‘cold abscess’—a lump or swelling, that is not accompanied by a secondary inflammatory response such as inflammation, heat and local tenderness. With TB, it’s often just a mass, so it mimics many kinds of tumors, especially in the musculoskeletal system. This creates a challenge in terms of early diagnosis.
An additional issue is that the people who are most at risk of spinal tuberculosis are often vulnerable, and not well tracked by medical professionals. The mycobacterium behind tuberculosis is very fragile, so it is difficult to get infected with TB if you are relatively young, fit and healthy. In most cases, our very powerful immune system will destroy the mycobacterium. However, people who are very young, such as less than three years old, or people who are over around 70, are more susceptible. The risk increases if you add in comorbidities such as diabetes or intravenous drug use. Often, IV drug users with HIV infections also have tuberculosis.
War and poverty increase incidences of spinal tuberculosis
In developing countries, there are widespread childhood vaccination programs to help protect the population against diseases such as TB. This is often not the case in the developing world, and coupled with low general health and malnutrition, we are seeing increased incidences of the illness. That is not to say this is a disease only of third world countries. Immigration and war have also brought a rise in cases in the developed world.
I am from Turkiye and the conflict in the Middle East over the past 20 years, particularly in Syria and Iraq, has brought many immigrants from those countries. Of course, the circumstances of war are not easy. It compromises basic health services, like vaccination and pregnancy aftercare, and there’s a lack of basics such as money for food and availability of clean water. All these issues mean that immigrants and homeless people are accessing health services at a very late stage, often when the disease has already started to present.
Tuberculosis can sit in the body and develop slowly over a period of years before we start to see the symptoms I outlined such as abscess or spinal deformity. Because tuberculosis is very fragile, it favors well perfused organs with high levels of oxygen, most commonly the lungs. This is why tuberculosis is most commonly understood by people as a lung disease. However, it also often presents in the kidneys. From these primary focuses, the disease travels through the blood into the spine and may develop spinal-TB as a secondary tuberculosis. It is attracted to metaphyseal part of long bones, such as the humerus, tibia and femur, as well as the extremities. It is able to take a strong hold where patients are immunosuppressed.
MRI with contrast: crucial tool in diagnosis
Early treatment greatly improves the prognosis for the patient and surgery can even be avoided, but the difficulties associated with diagnosis mean spinal-TB is often accompanied by high mortality rates. The important thing is for medics treating patients with abscess and no secondary inflammatory response to consider that spinal-TB may be the cause.
Diagnosis can come from a PCR test, which detects the presence of mycobacterium tuberculosis from a sample such as sputum, blood or fluid. However, it is difficult to gather a culture from the spine and lab analysis is not easy, and often time consuming.
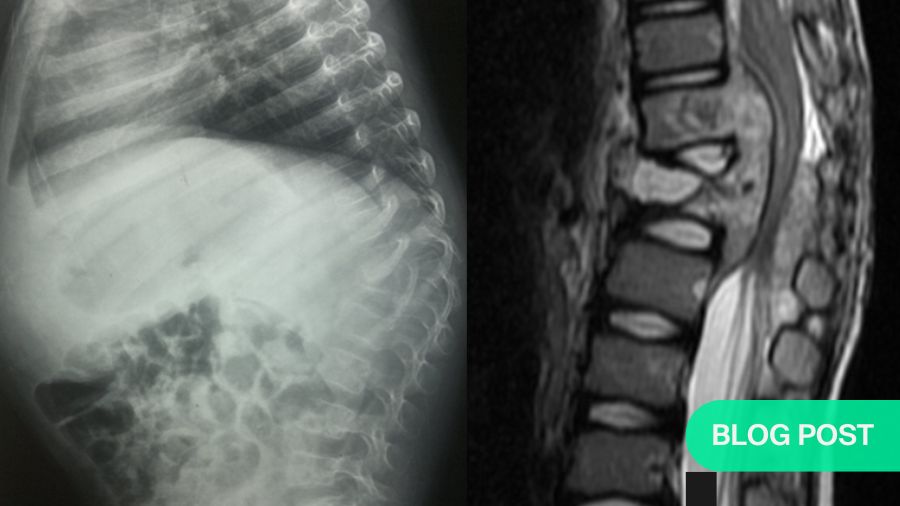
On the other hand, an MRI with a gadolinium contrast injection is really helpful in identifying the contrast media uptake around damaged tissue so called rim enhancement. Protection of disc space is another MRI finding of the spinal TB. For patients with late diagnosed Potts, you will often see epidural abscess formation together with the destruction of the vertebral bodies, which TB tends to attack because of its very strong blood perfusion.
S Rajasekaran—one of the prominent surgeons in the field—has developed useful “spine at risk” criteria for the young spinal-TB patient. If they have facet joint dislocation, retropulsion, lateral translation or toppling, this is likely to develop into post-TB kyphosis, which can result in the tethering of the spinal cord at the apex, leading to myelopathy and paraparesis or paraplegia of the patient at the end. Morbidity levels are high because treatment involves a very extensive surgery from the posterior approach.
Gold standard treatment for post-TB kyphosis
Interestingly, the gold standard in surgical approaches has changed very little in nearly a century. A British surgeon, Professor Arthur Hodgson provided the modern definition of the treatment in the 1940s, when tuberculosis was rife worldwide. Prof Hodgson travelled to Hong Kong to address a spinal TB epidemic there and ultimately created one of the most prestigious spine centers in the world. I know the history of it well because I did my fellowship in this fantastic center.
Prof Hodgson defined the Hong Kong procedure, which includes anterior radical debridement, removing the necrotic tissues until bleeding healthy bone is observed. This is followed by autogenous grafting with the ribs or iliac bone. The patient is then put into a cast or brace, and the spine generally fuses very well. This technique was used for a very long time and proved really effective. The Medical Research Council, which was a working group involving three centers, took a different approach to spinal TB treatment and then compared their results every 10 years. This provided us with a very well-structured approach based on a treatment flow chart at the end of 20th century.
Early detection greatly improves patient prognosis
While the Hong Kong treatment remains the gold standard, modern advances in materials science have allowed us to move away from structural autografts, which can introduce another morbidity. From the late 1990s we have found that bacteria in the spine struggles to attach to titanium, so you can safely use titanium in an infected area after very good debridement. Then, when the abscess and necrotic tissue are removed, you can add a titanium cage without having to use, for example, structural iliac bone.
Nevertheless, these are high-risk and invasive surgeries, and the best treatment option is always early intervention. If the disease has only local impacts and no neural deficit and deformity, the patient can undergo anti-TB chemotherapy and wear a brace for a year, or a year and a half. Sometimes, this prevents the progression of the disease and surgery is not required. Sadly, for too many patients, diagnosis only happens when the spinal deformity is already very severe. This makes it crucial that medics are able to spot the signs of TB and get our patients the help they need.
Complex spine case: post-spinal tuberculosis deformity
Alpaslan Şenköylü presents a complex case of post-tuberculosis spinal deformity on this AO TV 2024 must-watch interview (for registered users).
About the author:
Professor Alpaslan Şenköylü, MD, is part-time professor and head of the spine team at Gazi University Department of Orthopaedics and Traumatology in Turkey. He fulfilled his residency at Gazi University and completed his clinical spine fellowship under Professors Keith Luk and Kenneth Cheung in Hong Kong University. He has been a full professor in Gazi University since 2013 and a part-time spine surgery consultant in Lösante Hospital and Güven Hospital in Ankara.
Şenköylü's clinical and research interest is spine surgery including complex deformities, trauma, tumors, infections and degenerative conditions. He has published more than 100 peer-reviewed papers and has been serving as Spine Section Editor in the Journal of Orthopaedic Surgery and Acta Orthopaedica et Traumatologica Turcica. Professor Şenköylü is the editor of a book entitled “Essentials of Spine Surgery” (Springer, 2022).
Şenköylü is active in international organizations such as Scoliosis Research Society, Eurospine, AO Spine, and serving in various governance positions, as board member, committee chair, task force member, regional educational trainer, course chair, and faculty for these organizations. On July 1, 2025, Şenköylü started in his new role as the Chairperson of AO Spine Europe and Southern Africa Board.
You might also be interested in...
Why developing countries must do their own innovations and research
Prof S Rajasekaran examines the differences in medical care across the world, and calls for a new approach.
AO Spine deformity courses and educational events
Enhance your surgical skills with AO Spine, on life-like bone models or human anatomical specimens
AO Spine Knowledge Forum Reviews
A round-up of the latest research within the pages of Global Spine Journal.










