Why developing countries must do their own innovations and research
BY DR S RAJASEKARAN

All of us think that we are living under the same planet—the ‘Planet Earth’—but seldom do we realize that this planet is two: one of the ‘Haves’ and the other of the ‘Have-nots’, and the difference between these two is enormous.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
If we look at the per capita GDP of the various nations in this world, the results are alarming, from upwards of USD 66,000 in the United States to just USD 200 and little above in many countries. The difference is huge, and what is worrying is that the difference is increasing every year.
When there is so much discrepancy in wealth, we discuss about many opportunities that are lost. Yet seldom do we think of something very important: the opportunity to do research and achieve self-reliance through meaningful innovations.
Why is this important? If we do not have self-reliance in our research focusing on problems unique to the developing world, we then seek solutions for these problems from the developed world. Solutions are automatically sought from medical research from the western world. However, everything is different for a patient from the developed and the developing world. The spectrum of the disease, the available treatment, the infrastructure that is available, the cost provider, their affordability, and even their expectations from treatment is completely different.
So, when everything is different, the solution cannot be the same.
Arthritis and cataracts—the cost barrier in developing countries
Let us take the example of a gentleman with severe arthritis, and struggling even for his activities of daily life. He requires a joint replacement surgery but in many parts of the world, the cost of a joint replacement equals 18 months of his salary. The reason why less costly and affordable joint replacements are not available is that 95% of the research regarding arthritis and joint replacement prosthesis is confined to the developed world. When the solution comes from the west, it naturally comes with the cost, the business plans, and the profit margins of the developed world. So the solution becomes very expensive. Often this makes it unaffordable to patients in the developing world.
A solution that is not affordable is not a real solution at all. So, self-innovation is the key. The story of Aurolab of Aravind Eye Hospitals, Madurai, India is an inspiring example. In the early ‘90s, India was home to the world’s largest number of preventable blindness due to cataracts. Cataract surgery was always performed without an intraocular lens, but the quality of vision without an intraocular lens is vastly inferior to that with an intraocular lens. Each of these lenses costs hundreds of dollars and most of these poor people were not able to afford it at all.
When Aravind Eye Hospital was established by Dr Venkataswamy with the vision to eradicate preventable blindness, they realized that the single most important hurdle to perform cataract surgeries to the needy on a mass scale was the cost of the intraocular lens. So, they decided to manufacture it themselves. Their indigenous research was successful to provide a lens—which was equally good in quality—for the cost of just USD 2. Because of this huge cost saving, it then became possible to extend the benefits of this to millions and millions of people across the world. From just 150 lenses manufactured every day, they're now manufacturing more than 12,000 lenses and actually serve nearly 15% of the world market.
Since 1992 when they started, Aurolab has meticulously engineered ophthalmic solutions to tackle the world’s most critical vision care challenges. Today, they serve ophthalmologists in 160 countries across the world with a comprehensive suite of more than 200 technologies. To date it stands as an outstanding example of self-reliance and how it can lead way to low cost high quality care. Although it was first started for patients in India, they have extended their reach to more than 160 countries and in 2023, they supplied 3.1 million intraocular lenses, 7.5 million eye drops, and 15 million surgical products across the globe. They serve as a perfect example of how institutions from developing countries can richly benefit from self-innovations and self-reliance.
- The disease spectrum, patient’s expectations, their need, cost provider and affordability are all completely different between the developed and developing countries. When everything is different, the treatment cannot be the same.
- A solution that is neither affordable nor available is not an appropriate solution for the developing world.
- 70% of the disease burden is in the developing world and we need appropriate and affordable solutions. There is an urgent need for surgeons in the developing world to become ‘Surgeon Scientists’.
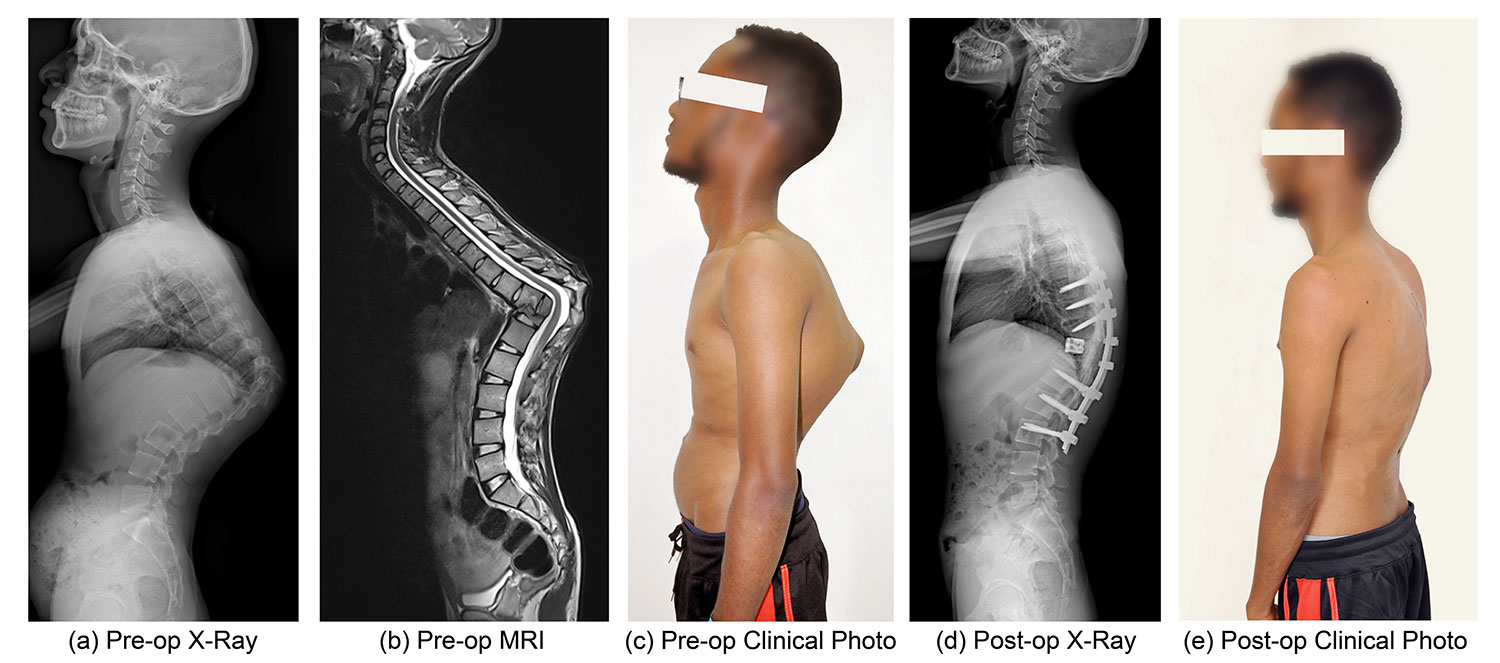
Severe case of post-tuberculosis infective kyphosis. This is still a major problem in the developing world. Patients frequently get severe pain and neurological deficits. Our clinical research was successful in evolving Spine at risk' signs which will help to identify children who are at risk for such progressive deformity and selectively subject them to spinal stabilization. This is very helpful to avoid unnecessary surgical morbidity and also preserve resources. We also evolved a corrective osteotomy procedure performed only from posterior approach. This also helped to reduce mortality and morbidity and improve results significantly. Such clinical research is vital for the developing world.
Spinal deformity and tuberculosis—preserving resources for where they’re most needed
Management of spinal tuberculosis is an other example. Tuberculosis is as old as man himself. Unfortunately it is still not a disease of the past. There are more than two million new patients with spinal tuberculosis every year and 90% of them are in the developing countries. The treatment that was advocated by the western world was radical debridement and reconstruction of the anterior column.
This was based on the principle of treatment of pyogenic infections which was more common in the western world. They also advocated anterior approach on the basis that an anterior disease needs anterior approach. Since TB was most common in the thoracic and thoracolumbar area, many new surgical approaches were devised involving thoracotomy and transdiaphragmatic approach to the thoracolumbar junction. These were surgeries of great magnitude with significant amount of mortality and morbidity.
More importantly, wherever TB was common, the facilities for these major surgeries were not uniformly available and wherever such facilities were available, tuberculosis was not prevalent. This discrepancy was a challenge in the management of this deadly disease.
A careful clinical research and documentation of outcomes allowed Prof S Tuli from India to propose his ‘Middle path regime’ where he advocated conservative therapy with anti-tuberculous drugs as the first choice of therapy and clearly defined a few indications for which patients would benefit from surgery. This saved more than 85% of patients with spinal tuberculosis from a morbid surgery and also allowed huge saving of resources in the developed world.
Clinical innovations and research also led to new surgical procedures where the entire debridement, posterior stabilization and anterior column reconstruction could be performed from the back only. This reduced mortality and morbidity considerably.
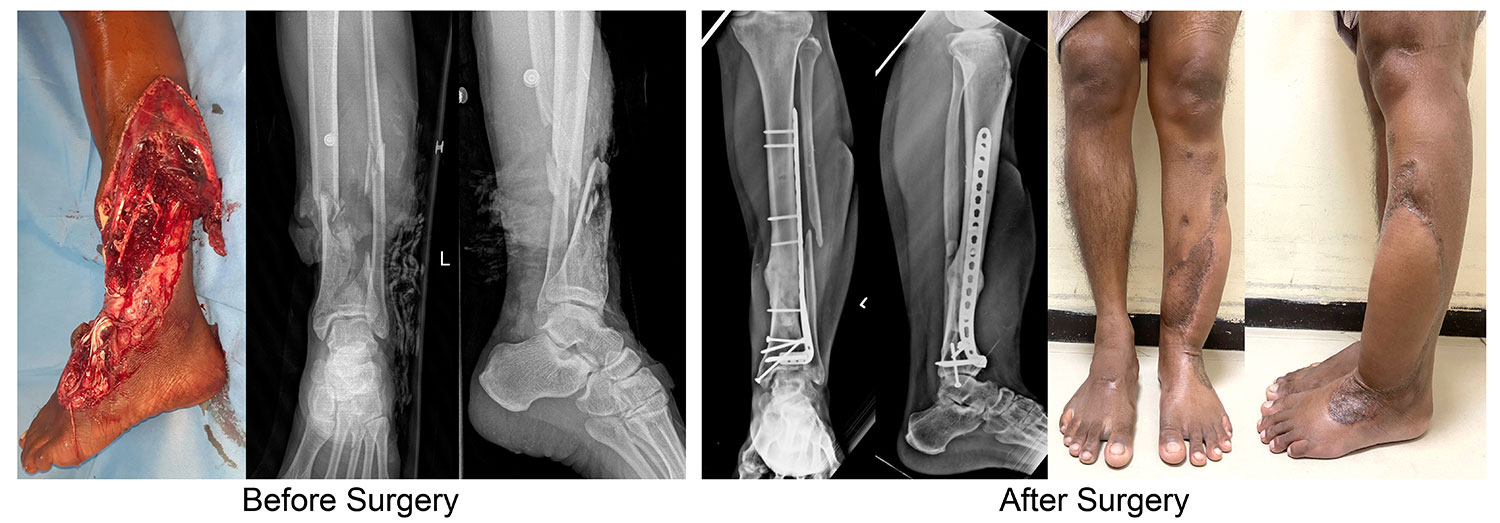
Severe open injuries of limbs are very common in the developing world due to high incidence of road traffic and work place accidents. The treatment for these are very variable in different countries and many limbs were not saved either because of lack of proper protocols or non-availability of expertise or insurance issues. We have done considerable research in this field of salvaging such limbs and also developed ‘GHOISS’ (Ganga Hospital Open Injury Severity Score) which gives very clear guidelines of when to salvage and also the timing and type of limb reconstruction. The indication and protocol for limb salvage are very different from the developed and developing countries and this area is a perfect example of why developed and developing world cannot have the same protocols and indications.
The Ganga philosophy and prevention of limb amputation
Trauma is an other field where, patients with the same injury, are treated differently in different parts of the world. In countries like India, there is one death every three minutes due to road accidents. A large number of these patients are motor-bike riders who suffer serious open injuries to limbs which are very challenging to salvage. In western world, prolonged hospital stay associated with multiple injuries which require salvage and the availability of costly prosthesis led to the trend of recommendation for amputation of most injuries.
However amputation was a challenge in the developing world as it not only had a social stigma, but also seriously disadvantaged the patient due to life style of the developing countries. Further good quality prosthesis was not available in rural areas. These challenges led us to develop GHOISS (Ganga Hospital Open Injury Severity Score) which allowed us to have a clear objective method of assessing open injuries and also various innovations which allowed reduction of stages of reconstruction and cut down costs. This protocol is now followed very widely in developing countries which has allowed saving of amputation of many limbs.
Huge research funding can also affect genuinity of research. Research has now become a big business and there is always the question of genuinity depending upon who funds the research. In an important publication in the British Medical Journal, it was found that in 200 major clinical trials across the world, only 8% were conducted independently of pharmaceutical or industry sponsors. About 87% of trials were co-authored and steered by the industry partners. The trial sponsors were also responsible for data analysis in 73% of the trials. When this is so, the genuinity of the results becomes highly questionable. This may be the reason why many important devices which come as a reliable solution for low back pain with a huge cost often fail to provide relief to the patients. In fact the outcomes are sometimes no better than just conservative treatment.
Many examples like injecting enzymes or growth factors or thermocoagulation or nucleopathy have been major flops in real life where the initial research showed promising results. The economics of the developed world cannot afford this huge wastage of resources.
Wellness, not treatment of sickness, is the need
Sickness is expensive to treat, and newer treatments are always more expensive. They are of less benefit to the patients and more profit to the industry. These expensive treatments and the percentage of ageing population increase the health care needs of the developed countries. Taking USA for example, the national health care expenditure which includes both public and private spending of health care are projected to climb from USD 4.8 trillion or USD 14423 per person in 2023 to USD 7.7 trillion or USD 21927 per person in 2032. Relative to the size of the economy, the health expenditure is projected to climb from 17.6% of gross domestic product in 2023 to nearly 20% by 2032 as raising healthcare costs continue to outpace the growth in the economy.
Poor countries can scarcely afford this. It would be wiser to prevent a disease than to treat it. Yet, it’s surprising to see that preventive care spending in the US constitutes only 2.9% of the total healthcare expenditures in 2018. Prevention is not only better, but it's also much cheaper than curing the disease. And that is exactly why it is not interesting for the research process in the developing world. Where there is no profit, there is very little money for research.
Let us take the example of old China where a doctor was paid when his patients stayed well. So, he was actually interested in the lifestyle, nutrition, family issues, home environment et cetera. And he was actually more of a health teacher to the whole family. Sickness of the family made the doctor a pauper. It was in his interests to practice good preventive medicine.
So, if you are a clinician or a surgeon from the developing world, there is much you can do for the welfare of humanity through clinical research. We have to convert ourselves from clinician to a clinician scientist. High funded, high budget research is not the only type of research. They are usually often chasing more expensive remedies for old diseases. What the world actually needs now is preventative medicine. This is where genuine research for the welfare of the world is required. There is much to do if you are a doctor in the developing world.
So, why wait?
About the author:
Prof S. Rajasekaran, M.S., DNB, F.R.C.S.(Ed), M.Ch.(Liv), F.A.C.S, F.R.C.S.(Eng.), Ph.D., is the Chairman, Department of Orthopaedic, Trauma and Spine at Ganga Hospital, Coimbatore, India, and Adjunct Professor of Orthopaedic Surgery of Tamilnadu Medical University. Rajasekaran is a past chairperson of AO Spine International Board, of AO Spine Research Commission, and a member of the AO Spine Knowledge Forum Trauma and Infection Advisory Board.
Rajasekaran has a special interest in spine surgery, arthroplasty, and clinical research in major trauma. He leads basic science research in spinal deformities, disc nutrition and biology, and genetics of disc degeneration, and is recipient of numerous prestigious international awards.
References and further reading:
- TEDxAmritaVishwaVidyapeetham talk by S. Rajasekaran
- Rajasekaran S. Natural history of Pott's kyphosis. Eur Spine J. 2013 Jun;22 Suppl 4(Suppl 4):634-40. doi: 10.1007/s00586-012-2336-6. Epub 2012 May 15. PMID: 22584918; PMCID: PMC3691402
- Kurup HV. A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Joint Surg Br. 2007 Apr;89(4):562; author reply 562-3. doi: 10.1302/0301-620X.89B4.19508. PMID: 17463133.
- Rajasekaran S, Sabapathy SR. A philosophy of care of open injuries based on the Ganga hospital score. Injury. 2007 Feb;38(2):137-46. doi: 10.1016/j.injury.2006.04.135. Epub 2006 Sep 6. PMID: 16950263.
You might also be interested in:
AO PEER
The AO Program for Education and Excellence in Research (AO PEER) is a knowledge platform for health care professionals who want to learn and improve their clinical research skills.
AO ITC
The AO Innovation Translation Center (ITC) activities include the development of clinical solutions with industrial partners, innovation gathering, proof-of-concept studies with innovators, strategic investment, and evidence creation through clinical research.
AO Course Finders
Select your specialty and explore all upcoming AO courses, webinars, and online events in your region or worldwide. You can also download a list of all upcoming events in your region
Research grants
As part of the individual research career development program for clinicians, the AO Foundation regularly offers funding opportunities for clinical studies as well as basic and applied research projects that address highly relevant clinical problems.