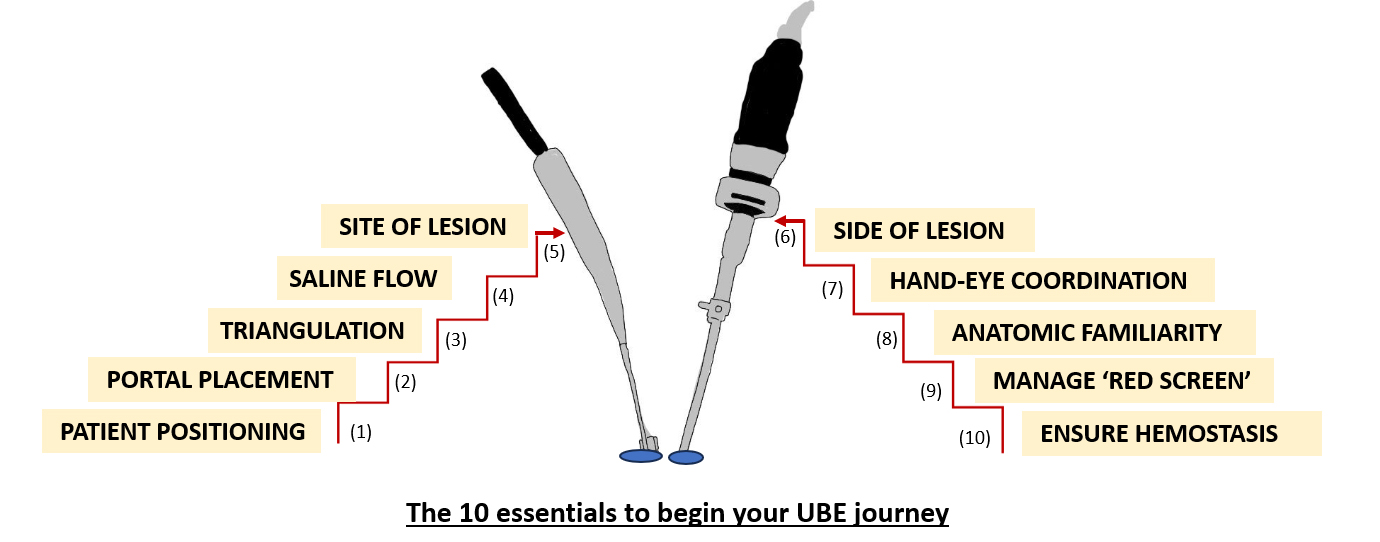
Unilateral Biportal Endoscopy (UBE): 10 essentials for starting your endoscopic journey
BY DR GUNA PRATHEEP KALANCHIAM AND DR JACOB YOONG-LEONG OH

Unilateral Biportal Endoscopy (UBE) is rapidly emerging as a transformative technique in minimally invasive spine surgery, offering an effective and muscle-sparing approach to a range of spinal pathologies. With its dual-portal system—one for visualization and another for instrumentation—UBE bridges the gap between traditional open procedures and modern endoscopic methods. In this article, we share ten essential considerations that can serve as a practical roadmap for surgeons embarking on their UBE journey.
-
Read the quick summary:
- Drs Guna and Oh outline 10 key points for spine surgeons starting with Unilateral Biportal Endoscopy (UBE) procedures.
- Essentials include positioning, portal setup, saline dynamics, and managing complications like the “red screen” phenomenon.
- These insights can help surgeons minimize risk, flatten the learning curve, and safely integrate UBE into their practice.
- Next steps include ongoing training, mastering advanced cases, and contributing to discussion on UBE best practices and innovations.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
The familiarity of the surgical instruments, enhanced visualization, and preservation of paraspinal musculature make UBE particularly appealing to the next generation of spine surgeons.
However, the transition into UBE demands deliberate preparation and a strong grasp of key technical principles to navigate the initial learning curve safely and efficiently.
These ten-points and tactics can serve as a strategy to minimize complications and to even out the steep learning curve to start enjoying the savor of UBE spine surgery.
1. Patient positioning:
The first and the most important step while planning for a UBE spine surgery. Most UBE surgeries are performed in prone position and flexing the spine widens the access to the commonest compressive sites in the spinal canal, namely the disc and the ligamentum flavum. Hence, placing the patient’s spine in kyphotic alignment is key for an ideal UBE decompression.
A wide variety of spine frames are available these days and the positioning frames are selected based on the surgeon preference and availability. Make sure the patient’s abdomen hangs free to prevent the engorgement of epidural veins and minimize the intraoperative bleeding.
2. Portal placement:
UBE, as we all know, is a dual (viewing and working) portal targeted surgical approach. So, it is important to place your portals in the right place based on the pathology to be addressed. Skin markings are usually placed in the anteroposterior fluoroscopy and in the initial cases of practice, a longitudinal skin incision is preferred over a transverse incision as it can be converted to open or microscopic approach with ease. Importance must be also given to the fascial incisions, and a cruciate incision is preferrable in the fascia to enable proper saline outflow.
Especially in patients with excessive lumbar lordosis, and in patients with migrated disc prolapse, portal placement could be tricky. So, choose your patients appropriately in the early stages of your UBE adoption.
3. Triangulation:
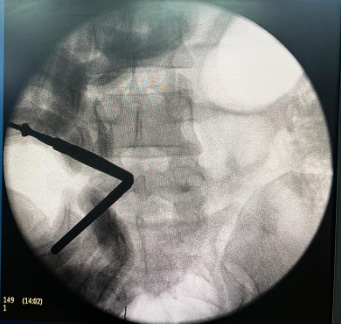
Intraoperative fluoroscopy image showing steps of triangulation at spino-laminar junction.
As orthopedic surgeons, ‘triangulation’ is a familiar word from arthroscopic training, and UBE exactly follows the same principles. It basically involves bringing the spine instruments in the working portal in view with the endoscope in the viewing portal. This step is performed under fluoroscopy guidance and could be challenging for the early adopters. It is important to be calm, focus on the process and take your time in the initial cases.
Especially in patients with high body mass index and thicker soft tissue, maintaining a proper triangulation could be arduous. Attending hands-on UBE workshops and cadaveric training can speed up the learning process.
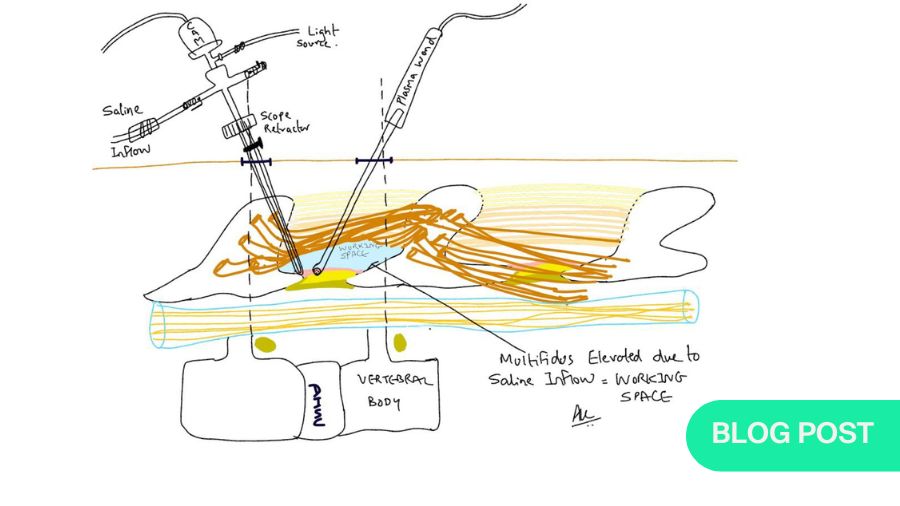
4. Saline dynamics:

Note the unhindered Saline outflow through the working portal.
Unlike knee or shoulder, the posterior spinal architecture does not have a true cavity, and UBE, being a water-based procedure, essentially involves saline flow in the surgical field. For the free flow of saline, the surgeon should create the space in the surgical field by detaching the posterior spinal musculature initially and later, by removing the bony elements during the surgery.
Unhindered saline inflow and outflow should be given the utmost attention throughout the procedure to have a clear endoscopic vision. The bony and soft tissue debris removed during the surgery are also washed out by the outflowing saline. We must focus on avoiding excessive saline pressure in the operating field to reduce the hydrostatic pressure induced neural damage.
5. Location of the pathology:
Be wise in choosing the more forgiving and less demanding pathologies as early cases. A lumbar level pathology is always a better choice than the cervical and thoracic lesions. Also opt for pathologies that can be managed using the more familiar interlaminar approach, rather than foraminal or extra foraminal pathologies.
Once the surgeon gains confidence with the common ipsilateral surgical techniques, over the top and contralateral approaches can then be a part of their UBE surgical journey. Decompression of calcified lesions (calcified disc, ossified yellow ligament), multi-level surgeries, and UBE fusion surgeries are reserved for experienced hands.
As soon as finishing the training in UBE, surgeons should start with decompressions and then progress towards instrumentation and fusion.
6. Side of the lesion:
Majority of the surgeons are right hand dominant. Hence, it is ideal to choose a left sided pathology as initial cases for obvious reasons – the instruments can be held in the surgeon’s dominant hand and all the surgical work can be performed with better control. Surgeons even train to operate the right sided pathologies by standing on the left side of the patient and placing the portals contralaterally. In ambidextrous surgeons, the side of the pathology would be less impactful in decision making.
Young surgeons should be trained to operate the pathologies on both right and left sides, irrespective of the side of the dominance.
More on the right-sided approach in Unilateral Biportal Endoscopy (UBE): right-sided approach for right-handed surgeons.
7. Hand-eye co-ordination:
In UBE, the endoscope and the instruments are placed at an angle, directed towards the pathological site. Hence, hand-eye coordination is an essential aspect of UBE surgery. Surgeons should be able to assess the distance of the endoscope to the surgical tools intra-operatively to avoid the damage to the endoscopic lens. Especially while using Rongeur, high speed drill, neural damage can also occur if used inappropriately.
Good experience with the use of burr in microscopic spine surgery speeds the learning process, though the magnification in UBE is much higher than the microscope.
8. Anatomical familiarity:
Surgeons should be aware of the endoscopic spinal anatomy before starting to perform UBE surgeries independently. The facetal synovial tissues, meningovertebral ligaments, midline dural folds would be well appreciated under the endoscope which a surgeon seldom focuses on during open spine surgery.
Hence, such anatomical structures and landmarks like the J-point (lumbar spine), V-point (cervical spine), V-cleft of the ligamentum flavum need specific attention during the surgical procedure to lessen the risk of adverse events and improve the overall patient safety.
Also, the adequacy of decompression while viewing though the endoscope must be clearly understood by the beginners to perform the clean and complete surgical job.
9. Tackle the ‘red screen’ phenomenon:
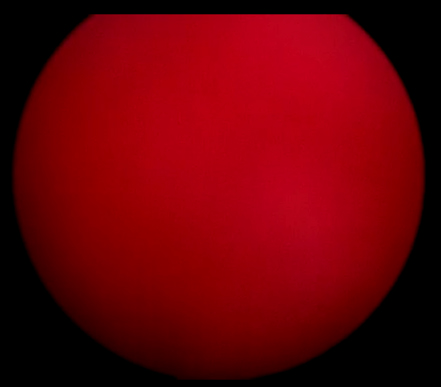
Image showing “Red screen” Phenomenon in endoscopic monitor during UBE surgery.
Continuous bleeding during UBE surgery is a troublesome event. It prolongs the overall duration of the surgery and even in some cases where bleeding could not be controlled, we end up converting it to open surgery.
The term “red screen” phenomenon is used in cases where the endoscopic screen is completely obscured by the bleeding at the surgical site. This creates a lot of anxiety for the operating surgeon and hence, surgeons should be able to locate the bleeders early and address it when the vessel starts with a minor ooze.
The important part of managing this condition is not to panic and stay calm during this event. Advancing the endoscope towards the bleeder gives a better magnified view of the vessel, enabling proper coagulation. Other strategies like transient minimal increase in saline pressure and use of flowable hemostatic agents would also be very helpful in this regard.
10. The final hemostasis:
The last and the most important step in UBE is achieving hemostasis before final wound closure. Unlike open spine surgery, there is very less dead space formation in UBE and inadequate hemostasis would result in hematoma formation in the small, operated space resulting in significant nerve root compression.
Though the hematoma seen in a post-operative MRI scan can be asymptomatic, symptomatic patients would warrant re-exploration and evacuation of the hematoma. Hence, confirming optimal hemostasis is of paramount importance before proceeding with wound closure. In our experience, placement of drains for 24–48 hours has helped to reduce the risk of symptomatic post-operative hematoma.
Conclusion
Unilateral Biportal Endoscopy (UBE) represents a significant advancement in the realm of minimally invasive spine surgery, combining surgical familiarity with the precision of endoscopy. The ten essentials outlined here—ranging from optimal patient positioning to mastering saline dynamics and ensuring final hemostasis—provide a structured framework for surgeons aiming to adopt UBE with confidence.
While the learning curve may appear steep, careful case selection, hands-on training, and attention to technique can lead to consistent, safe, and satisfying outcomes. As experience grows, the potential of UBE extends well beyond decompressions, opening doors to more advanced procedures and a broader scope of spinal care. With preparation and practice, spine surgeons can integrate UBE into their clinical repertoire and deliver its benefits to a growing patient population.
About the authors:
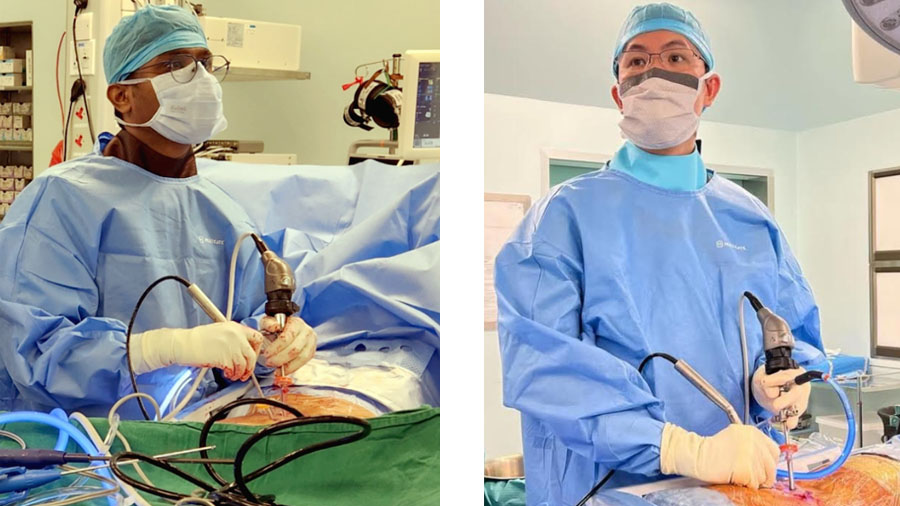
Dr Guna Pratheep Kalanchiam, MBBS; MS (ORTHO); FNB (SPINE); Global Diploma (Spine); FESS (Korea); FRSS (Singapore); FMISS (AO Asia-Pacific) is a fellowship-trained Orthopaedic Spine Surgeon from Madurai, Tamil Nadu, India. He was awarded the AO Spine International Minimally Invasive Spine Surgery Fellowship, the fellowship in Robotic Spine Surgery in 2024, and also the Asia Pacific International fellowship in Spine Deformities (2025). He specializes in Unilateral Biportal Endoscopy, minimally invasive, Robotic, and complex Spine deformities. He is a faculty member in various regional Spine Conferences, and has presented his work at several National and International meetings.
Dr Guna has a keen research interest and has published his work in various high-impact international scientific journals. He is an active member of the AO Spine, the AO Spine Youth Club, the Asia Pacific Spine Society (APSS), the Association of Spine Surgeons of India (ASSI), and the Pacific and Asian Society of Minimally Invasive Spine Surgery (PASMISS). Through his continued efforts and contributions to UBE surgery, he strives to improve the quality of patient care and the surgical outcomes.
Dr Jacob Yoong Leong Oh MBCHB; MMed (Ortho); FRCS Orth & Tr; FISS is an Orthopedic surgeon from Singapore and currently serves as Senior Consultant and chief of Spine Surgery, at the Department of Orthopedic Surgery at Tan Tock Seng Hospital. He is also the founder and director of the National HealthCare Group (NHG) Spine Centre. His area of interest lies in Minimally Invasive Spine Surgery, Adult Spine deformity, Spinal navigation, and Robotics.
Dr Jacob Oh is associated with various international organizations and has been appointed as a board member of, ASEAN MISST, PASMISS, and ISASS AP. He is the AO Spine Educational officer for East Asia, and Secretary of the Singapore Spine Society.
References and further reading:
- Kalanchiam GP, Kaliya-Perumal AK, Sampath L, Boey ETH, Oh JY. Complications in Uniportal vs Unilateral Biportal Endoscopic Decompression for Lumbar Spinal Stenosis: A Scoping Review. Global Spine J. 2025 May 30:21925682251346413. doi: 10.1177/21925682251346413. Epub ahead of print. PMID: 40448305; PMCID: PMC12126473.
- More about the steep learning curve for UBE, the pain-points, and a checklist of practical tips how to overcome the obstacles is provided by Dr Ashwinkumar Vasant Khandge in a Guest Blog article on Unilateral Biportal Endoscopy (UBE): Why spine surgeons should make the leap and master the skills.
- Dr Ashwinkumar Vasant Khandge unpacks the mysteries of right-sided UBE approach in Unilateral Biportal Endoscopy (UBE): right-sided approach for right-handed surgeons.
You might also be interested in...
AO Spine MISS resources
Our educational MISS material and courses cover all types of minimally invasive spine operations through tubular/microscopic, endoscopic, and instrumented procedures.
AO Spine Guest Blog articles
Read more guest authored articles on hot topics or submit your own proposal and share your work with the global spine community.
Be part of the GSC success story!
The Global Spine Congress is the worlds most international spine congress. Submit your abstracts and register early to secure your place and save.