Unilateral Biportal Endoscopy (UBE): Why spine surgeons should make the leap and master the skills
BY DR ASHWINKUMAR VASANT KHANDGE
Spine Surgery has progressed tremendously in recent decades and there has been a paradigm-shift with the introduction of minimally invasive spine (MIS) care. A new era rises with the advent of spine endoscopy for both spine surgeons and the patients. State-of-the art training facilities and ever progressing research into new modalities of teaching have helped the educators to facilitate spine surgeon training to develop the requisite skill set for endoscopic spine surgery. Different MIS approaches are thoroughly covered in the AO Spine MISS Spectrum Seriesonline course. Several Global Spine Congress symposia, pre-courses, and sessions will also focus on the latest advances.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Endoscopic spine surgery has progressed from the generations of full endoscopy like the transforaminal to inter-laminar endoscopy and more recently to the stenosis surgery. The full-endoscopic spine surgeries have stood the test of time but there is a new-contender on the block.
Endoscopy-assisted surgery using an arthroscope and routine spine instruments is what is known as Unilateral Biportal Endoscopy (UBE). UBE has evolved rapidly during the past decade and has been gaining a lot of popularity and traction amongst the spine surgeon fraternity globally. So, the question arises: What is UBE all about?
What is Unilateral Biportal Endoscopy (UBE)?
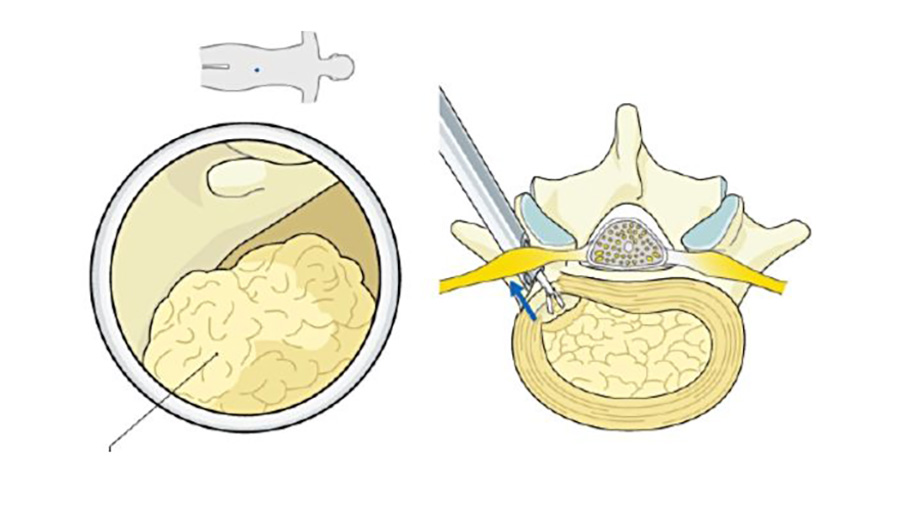
A simple answer to this not so simple question is as follows: UBE utilizes two skin incisions referred further as portals. One portal you make is called the viewing portal and the other one is called the working portal. These two well-planned portals give you a sneak view into the inter-laminar window and help you to perform surgical steps as you would normally do with open or microscopic spine surgery.
Commonly being a right-hand dominant spine surgeon, you stand on the left side of the prone and anesthetized spine patient. Your non-dominant left hand inserts an Arthroscope (4mm 0 degree/ 30 degree) with an arthroscopy sheath through the viewing portal that is well planned. Your dominant right-hand uses the working portal to facilitate routine spine instruments in front of your arthroscopy camera lens.
Once you bring the tip of your instrument in front of your arthroscope lens and can see the same on the screen in front of you—et Voilà! You have just performed one of the most important steps in UBE—Triangulation.
To state in simple words UBE, with the help of a camera and arthroscope, provides a bright, magnified, and illuminated surgical view of the inter-laminar window like what is seen with a microscope. Thus, helping you to perform precise surgical maneuvers with routine spine instruments with less likelihood of an injury to the underlying nerves.
National Spine Conference – Association of Spine Surgeons of India, 2024
Why spine surgeons should train to master UBE?
UBE is a beautiful amalgamation of sports medicine and microscopic spine surgery. Apart from few, the instruments used in UBE are the same that you use in microscopic spine surgery or open spine surgery. Unlike full endoscopy where you are restricted to the endoscopic sheath and working channel of your scope here freedom, versatility and resourcefulness is knit in the fabric of UBE.
Many of us have are excited about learning and mastering a difficult skill set such as UBE to improve surgical outcomes and provide our patients with most recent advance in spine endoscopy.
I started my UBE journey with the same conviction until I realized there are large gaps that need to be filled to make this leap towards mastering this skill set. These gaps can be divided into frustrations, fears, and pain-points that you may face on your journey through these hurdles to UBE mastery.
-
Spine surgeons’ main frustrations on the road to mastering UBE include:
- Limited access to quality UBE training opportunities in their country. Hence, you should always aim for the best training centers around the globe and come back to start performing your UBE cases. You can even visualize yourself as a beacon of hope to newer spine surgeons in your country who are desiring to learn UBE and contemplate starting your own UBE training programs in future.
- You may worry about the learning curve and the number of cases required to master UBE. The literature is divided on the same but based on my experience the number of cases required differs from surgeon to surgeon and is based on your previous experience in open and microscopic spine surgery. I may ruffle someone’s feathers here, but I think being trained in open and microscopic spine surgery is a must to be a good UBE spine surgeon.
- You may also get frustrated about which type of endoscopic spine surgery to choose as there is lack of standardized consensus and protocols for learning by authorized associations. You may get into the perennial debate of full endoscopy versus UBE and how one is superior or better or less invasive than the other. These questions are better answered by discussing face to face with Key opinion leaders (KOLs).
- You may worry about high stress levels during your initial cases. These types of frustrations can be minimized with optimal cadaver workshops, hands-on UBE training workshops and mentorship under experts. Also, understanding your own limitations and wisely choosing beginner cases at the start of your UBE career is the key point here.
- You may suffer from peer pressure and suboptimal support from your reference group. Here, you will benefit immensely by attending dedicated endoscopic spine conferences where you meet like-minded spine surgeons and KOLs in respective specialty. Social media stands tall in the 21st century and you may benefit from LinkedIn and other dedicated UBE groups on Facebook, etc.
-
Common fears when starting using UBE:
- Fear of failure: Fear that you may not be able to learn the technique owning to age (most common reason). Age is just a number and the more experienced in spine surgery you are the faster you will adopt to UBE. But the same doesn’t stand true for younger spine surgeons. Having a thorough open and microscopic MIS spine surgery experience is paramount before starting your UBE journey.
- Fear of complications: Fear of complications in early learning curve is universal in all types of surgical procedures. UBE has a relatively better learning curve. On a lighter note, “the more you bleed in training, the less you bleed in war” and hence the role of optimal cadaveric training and hands on workshops before venturing into individual cases.
- Fear of damage to professional reputation: Here again peer pressure and lack of support from professional community must be handled well.
- Fear of legal issues: One may fear about complications and the legal repercussions that it may invite. These need to be checked at the national level and government health policies.
- Fear of equipment malfunction: UBE or any endoscopic spine surgery uses specialized equipment’s like camera, arthroscope, shaver drill and radiofrequency plasma generator that we as spine surgeons are unaccustomed to. You feel the unfamiliarity of these equipment’s and they form the major hurdle in UBE learning curve. Despite using the same equipment’s multiple times, they may fail in your Nth case and then you may be handed over a completely different and unfamiliar endoscopy tower that you haven’t used before. Hence try to make yourself flexible while using different types of these equipment’s to ease your malfunction anxiety (More on these practical tips further).
- Fear of impaired career progress: As spine surgeons you have been at the forefront of your career beginning from your pre-med to residency days and later fellowships. With UBE your career can get that long lost spark and help you propel forward in the career graph.
-
How to overcome common pain-points perusing UBE:
- Lack of hands-on experience: You may want to visit an UBE expert offering hands on training either in your country or outside.
- Suboptimal Operating Room (OR) support team: You may find it worth to invest in teaching your OR team about the newer technique such as UBE. Training them and getting everyone on the same page is something you should look forward to. Trained OR support team may ease your anxiety and frustration regarding unfamiliar equipment malfunctioning.
- Uncertain patient outcomes / Lack of conviction for UBE: You must visit a KOL in UBE or an expert who routinely performs these procedures. Endoscopic spine surgery is a philosophy that starts with careful pre-operative analysis of radiographs, CT scans and MRI scans followed by clinic-radiological correlation. The decision-making process in endoscopic spine surgery requires a specific temperament that takes some time to develop. The easiest and fastest way to develop this temperament is by shadowing an UBE expert and gaining regular insights from them. This process may take time for you but once the attitude of endoscopic spine surgery is developed your surgical decisions will change for the better.
- Time constraints: You may have certain OR days and timing may be restricted. Performing initial UBE cases can be time consuming and hence keeping a timer in front of your eyes near the monitor will help to be time conscious.
- Financial investment in UBE equipment: Having a UBE set and an arthroscopy tower with camera, light source, shaver drill and radiofrequency generator is a prerequisite for UBE. These can be bought by your institution but for almost 50 percent of us (based on data from LinkedIn poll) these expenses or investments are borne by the spine surgeons themselves. Hence adequate financial planning for the purchase and maintenance of these equipment’s should be considered.
- Patient dissatisfaction: You should counsel the patient preoperatively regarding the need to convert an endoscopic spine surgery to open or microscopic spine surgery. This not only helps us avoid patient dissatisfaction but eases you off from unnecessary stress and performance anxiety. Now you can focus on doing the job well instead of doing the job through a particular surgical way.
- Burnout and fatigue: These are real world problems that need to be addressed by quality training, timely appraisals and keeping one involved in academics and academic events.
Don’t feel bogged down by the previously enumerated issues! Our desires will keep us moving on the path to excellence in this surgical field.
-
The most common UBE related desires and motivations that drive spine surgeons:
- Spine surgeons desire of comprehensive UBE training programs with cadaveric training, hands on training and then handholding by the mentor for a specified time duration.
- They desire to advance their surgical career with skill acquisition.
- You desire to be recognized at national or international level for your surgical expertise.
- You desire for peer recognition and improved patient outcomes.
-
Checklist of practical tips to ease your journey into mastering UBE:
- After anesthesia always position your patient prone on a spine frame. The use of a spine frame helps in flexion of the lumbar spine and thus opens the inter-laminar window. A couple of millimeters of added opening will not matter much in open or microscopic spine surgery but it sure does make your life a lot easier in UBE. With UBE the added magnification and an opened interlaminar window aids in performing laminectomy and other surgical steps safely.
- Try to wear a single glove in UBE. UBE is a fluid-medium surgery and outflow normal saline flows out of the working portal. While using radiofrequency probes in coagulation or ablation mode, the local temperature around the tissues may rise. This increase in temperature can be picked up far faster with a single glove prompting yourself to stop the usage of the probe and let some more fluid flow out to cool down the local water temperature around the neural elements.
- There is a lot of variability in the commercial endoscopic spine surgery drapes that are available. Better to use stack of sterile towels to create a dam and a sterile plastic bag to collect the outflow saline all pasted together with an adhesive sterile drape. It is frustrating to get yourself wet in a cold OR and to make your surroundings a pool of water and hence you should be meticulous with water management.
- Making the vertebral end plates squared and parallel is an important point but often neglected before marking and planning your surgical trajectories.
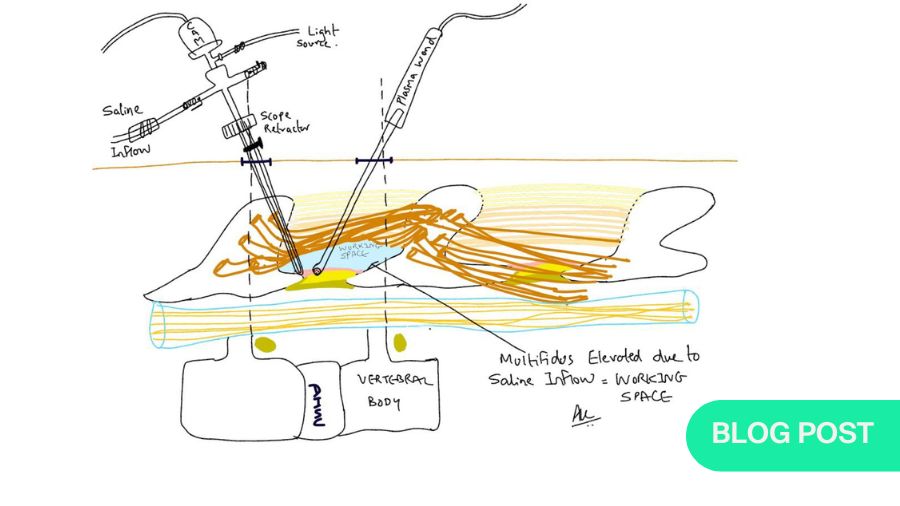
- Using a T-shaped periosteal elevator or the blunt base of a number 7 handle helps you in the pre-endoscopy stage to prepare a working space. The gentle use of these instruments lifts the multifidus muscle and thus reduces the work of a radiofrequency probe and thus minimizing collateral muscle damage.
- You should always triangulate your surgical instruments under C-arm fluoroscopy guidance in antero-posterior and lateral projections. This helps you to cross check the levels with MRI images and avoids wrong level surgery and prolonged surgical time.
- A right-handed surgeon stands on the left side of a prone patient. The endoscopy tower with the screen, the C-arm monitor, and the c-arm screen come from the opposite side in front of your field of vision.
- Shaver burrs are recommended in UBE Spine surgery for the following reasons: vast catalogue of disposable burrs with different sizes and shapes, hood to protect the underlying neural tissues, high torque and optimal RPM and the facility to attach suction tubing to the shaver handpiece. Foot-controlled shaver burrs are preferred.
- Radiofrequency plasma equipment’s form an integral part of UBE. There is a lot of variation in the types of probes that are available in the market. Most frequently used probes are 90-degree ones that are foot pedal controlled. Using a hand-controlled probe is preferred by some spine surgeons therefore you must try different probes before you settle on a particular machine and probe. The coagulation and ablation settings vary from one machine to another and hence it would be a good idea to talk to your mentor regarding the same.
- Another point that is commonly missed is to get the video recordings of your surgeries. I recommend you review these videos on the same evening and try to edit them with marked surgical step subtitles.
This habit will serve two purposes: One you will focus on two questions:
a. What went well in my UBE case?
b. What could have been done better?
Here, instead of focusing on other things with these focused questions we re-orient our thinking and mindset towards growth.
Secondly, editing your videos and converting them to sizeable chunks of approximately 4–8-minute duration, you set yourself up for any future academic event where you can present these videos.
- Use a timer: It is advisable to use a timer while performing UBE cases. You may very well be lost looking at the screen into the beautiful world of spine endoscopy, coagulating every small bleeder and taking down every small tissue strand. These things may prolong the surgical orientation and hence a timer will make you time aware and relaxed.
- Scope retractor: With full endoscopy you have something called as an endoscopy sheath that helps in soft tissue retraction and can double down as a nerve root retractor. In UBE it is advisable to use a scope retractor, a specialized instrument to aid in retraction. The scope retractor is one of the few essential and unique instruments required in UBE.
- Angled curettes: Small angled curettes can help you to release the attachments of the yellow ligament and thus helping an en-bloc removal.
- Hemostasis: Hemostasis is an important component of any spine surgery. But with UBE an important distinction arises as it is a fluid-medium surgery. With microscopic spine surgery or open surgery, we are trained to hold the suction in our non-dominant hand that aids you to suck the bleeding and also in some tissue retraction. In UBE the same thing is done by the arthroscopy sheath but instead of “Suction” we are “Washing” away the blood with a uniform flow of normal saline from the sheath. Hence UBE is not suctioning but washing away the bleeding.
- Rotating Kerrison punches: These are not a pre-requisite but nice to have in your UBE set. Check them yourself in cadaver workshops before investing in these specialized punches.
- Relaxation in OR with calm music can be helpful to some spine surgeons. This is dependent on you but having a supporting OR team is highly advantageous.
- The orientation of UBE is like microscopic spine surgery. But a critical difference exists as microscopic spine orientation is three-dimensional, and UBE is two-dimensional and hence every surgical step needs to be double checked in the initial learning curve to avoid inadvertent complications.
- Knowledge update: Like every spine surgery technique UBE demands what the Japanese call as “Kaizen” or continuous improvement. This can happen by reading textbooks on UBE, following literature, attending meetings and academic events focused on endoscopic spine surgery. If you are in an academic institution it will help to give topics on UBE to your residents and fellows to work on and to thus get the younger generation involved.
- Practicing in an institution or in private practice never be shy to convert your UBE cases to microscopic or open spine surgery if need arises. It is a good idea to always carry your surgical loupe with you for UBE cases. Never commit that the surgery will be done through UBE technique as there are a lot of variables that are not in your control. It is a good idea to be well informed and comfortable with different equipment’s on the endoscopy tower.
- Avoid unnecessary debates of whether full endoscopy is better, or UBE is better. Once you talk with KOL s and experts you should make up your mind as to which path you want to walk on. It is always better to know all forms of endoscopy but for the want of time, choose one and don’t look back.
- When to start UBE? As previously emphasized UBE takes a level of spine surgical maturity before you venture into the technique. I advise everyone to transition from open spine surgery to microscopic spine surgery and then to UBE. One should be ready and competent to convert UBE to microscopic spine surgery in the face of a complication. Hence, the skill set of open spine and MIS gives you the apt surgical orientation and helps you to understand the relevant surgical anatomy in detail before UBE.
To conclude, you must pursue UBE with intense dedication and focus and have patience in your initial learning curve. Mastery will come after hours of deliberate practice on cadaveric models and UBE simulators. Hand-eye coordination takes time but once it develops UBE will become your second nature like open or microscopic spine surgery and then the vast expanse of spine surgery will open to you. Having faith and conviction in your surgical technique will help you deliver the best results to your patients and help avoid burn-out and fatigue.
With UBE we are probably in the “Early Adopter” phase of the technology adoption curve, and the more spine surgeons that comment and contribute their take the better. Increasing spine surgeon engagement to UBE and related topics may help the technique to propel and reach the masses.
About the author:
Dr. Ashwinkumar Vasant Khandge, MS, DNB, MNAMS, F. ASSI, F.EMISS, is a distinguished Consultant Endoscopic Spine Surgeon, clinical associate professor in Orthopedics and Spine Surgery at Sudarshan Orthovision Hospital and Dr. D Y Patil Medical College and Research Centre, located in Pune, India. With extensive expertise in his field, Dr. Khandge holds notable positions, serving as an invited national faculty member on Unilateral Biportal Endoscopy (UBE) and as a consultant to Nexon Medical in Switzerland, where he contributes to the development of innovative educational methods for training spine surgeons in UBE techniques.
His commitment to advancing spinal surgery is further evidenced by his involvement with the AO Spine MISS Taskforce, where he serves on the supporting surgeon board and has played a pivotal role in designing the AO Spine UBE curriculum. Dr. Khandge's dedication to both clinical practice and education reflects his passion for improving patient outcomes and advancing the field of spine surgery. With his multifaceted roles as a surgeon, educator, and innovator, Dr. Ashwinkumar Vasant Khandge continues to make significant contributions to the field of orthopedics and spine surgery on both national and international levels.
Further reading:
- Pao JL, Lin SM, Chen WC, Chang CH. Unilateral biportal endoscopic decompression for degenerative lumbar canal stenosis. J Spine Surg. 2020 Jun;6(2):438-446. doi: 10.21037/jss.2020.03.08. PMID: 32656381; PMCID: PMC7340817.
- Heo DH, Hong YH, Lee DC, Chung HJ, Park CK. Technique of Biportal Endoscopic Transforaminal Lumbar Interbody Fusion. Neurospine. 2020 Jul;17(Suppl 1):S129-S137. doi: 10.14245/ns.2040178.089. Epub 2020 Jul 31. PMID: 32746526; PMCID: PMC7410385.
- Kim JS, Park CW, Yeung YK, Suen TK, Jun SG, Park JH. Unilateral Bi-portal Endoscopic Decompression via the Contralateral Approach in Asymmetric Spinal Stenosis: A Technical Note. Asian Spine J. 2021 Oct;15(5):688-700. doi: 10.31616/asj.2020.0119. Epub 2020 Nov 16. PMID: 33189115; PMCID: PMC8561150.
- Books:
Unilateral Biportal Endoscopy: How do I do it
Endoscopic Spine Foundation India – Dr Malcom Pestonji
Unilateral Biportal Endoscopic Spine Surgery
Basic and Advanced Technique-Dong Hwa Heo, Cheol Woong Park, Sang Kyu Son, Jin Hwa Eum
Unilateral Biportal Endoscopy of the Spine
An Atlas of Surgical Techniques – Javier Quillo-Olvera, Diego Quillo-Olvera, Javier Quillo- Reséndiz, Michael Mayer
You might also be interested in:
AO Surgery Reference
The latest AO Surgery Reference module covers MISS treatments for degenerative disorders—disc herniation, stenosis, and spondylolisthesis with definitions, indications, practical guides, and a range of microscopic and endoscopic techniques for cervical and lumbar disc herniation.
AO Spine MISS Spectrum Series
A comprehensive online learning experience for practicing surgeons who have little to no skills in MISS, fellows in an orthopedic or neurosurgery spine program, and residents in their final years who will specialize in spine surgery.
AO Spine Guest Blog
The AO Guest Blogs publish articles directly from the community. What else are surgeons talking about today, what are the latest trends affecting their careers? Submit a proposal to publish your own post and share with the network.