Dealing with a ureteral injury after anterior lumbar spine interbody fusion surgery (ALIF)
BY HENRI-ARTHUR LEROY AND PIERRE DE BUCK

Anterior lumbosacral interbody fusion (ALIF) surgery has gained a lot of popularity in the last few decades and has become a predominant approach in treating various indications, such as discogenic back pain, spondylolisthesis, degenerative lumbar scoliosis, intervertebral foraminal stenosis, or spondylolysis. In comparison with the conventional posterior approach, ALIF presents several advantages: direct access to the spine without muscle dissection, less blood loss, less postoperative pain, improved fusion rates, and shorter hospital stays. But rare intra- and postoperative complications—such as vascular or ureteral injury or retroperitoneal hematoma—still remain, and spine surgeons, as well patients, must be aware of the risks.
While vascular injuries are often the most dreaded complications in ALIF surgery, the adverse urological complications can also be life-threatening. The most often reported urological complications are lesions of the sympathetic hypogastric plexus with retrograde ejaculation and erectile dysfunction. Here, we will look closer at a case of urinoma to highlight the difficulties related to diagnosis and how the most severe complications could be avoided.
Fusion of L5-S1 segment by ALIF
The 35-year-old man in question had suffered from of chronic lumbar pain associated with alternating bilateral sciatica for more than ten years. The spine MRI showed a L5–S1 discopathy with grade 1 spondylolisthesis and bilateral spondylolysis. The patient’s situation wasn’t improving with conservative treatment, and he was eligible for an ALIF surgery to fuse the L5–S1 segment. In a second step, a posterior percutaneous screw fixation was also planned to obtain a 360° arthrodesis.
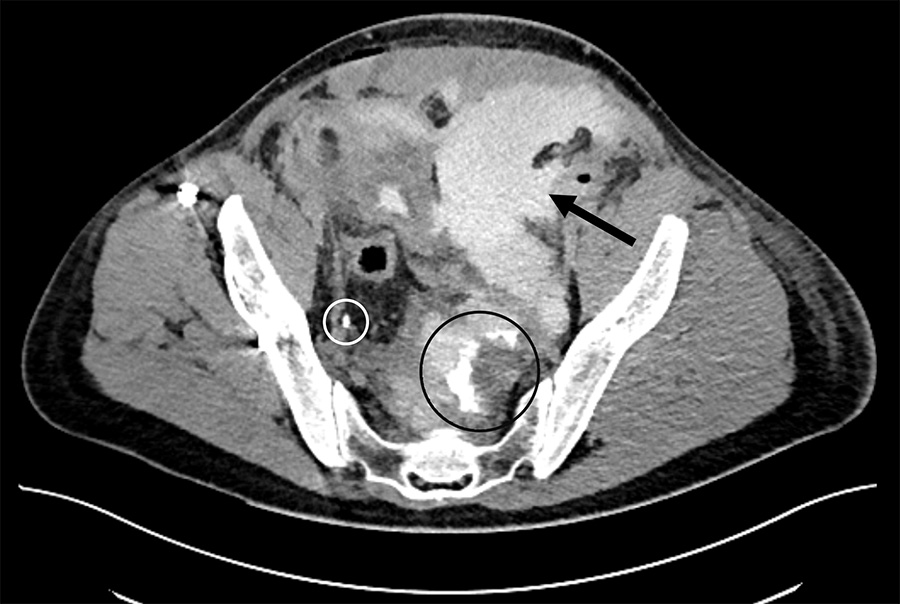
The surgery was performed as planned, but on day 4 after surgery, the patient started experiencing abdominal pain, nausea, and vomiting. At abdominal palpation, we found a boardlike abdominal wall in the left lower quadrant. The abdominal contrast-enhanced CT scan revealed a left retroperitoneal collection with intraperitoneal extension, interpreted as a hematoma that was compressing the ileum, and the urinary upper tract, responsible for moderate bilateral hydronephrosis (Fig. 1).
The first diagnosis was an intestinal occlusion secondary to the intraoperative site collection. Consequently—and after gastrointestinal surgery consult—a nasogastric tube was inserted. But the pain persisted on the following day, and his kidney function was deteriorating with an estimated glomerular filtration rate decreased from 100 to 60 ml/min.
A contrast-enhanced CT with urogram was then performed, reporting a leak of contrast-enhancement liquid from the left distal ureter inside the postoperative collection. The patient was diagnosed with a compressive urinoma due to a left distal ureteral iatrogenic injury.
Major differential findings to diagnose urinoma after ALIF
The major differential diagnosis of urinoma is a lymphatic system injury such as chyloretroperitoneum or lymphoceles. An injury of the lymphatic channels can induce a retroperitoneal collection, resulting in a lymphocele, with symptoms and CT findings very similar to those of ureteral injuries. The specific uroscanner findings in favour of a lymphocele is the absence of contrast extravasation.
If a drainage is performed, the creamy white aspect of the liquid, with no smell of urine, is pathognomonic of a chyloretroperitoneum due to the presence of chylomicrons. Moreover, fluid collection in the lymphocele seems to be much more abundant, and it can be distinguished from urine with laboratory examinations. It must be emphasized that these complications seem to be more frequent after thoracic or upper lumbar spinal procedures.
Another differential diagnosis could be cerebrospinal fluid (CSF) leakage. It must be thought of systematically in the case of a dural tear during the surgery. A major depletion of CSF could induce intracranial hypotension symptoms, such as postural headaches, neck stiffness, nausea, or vertigo. On laboratory examination, the beta-2-transferrin assay is the gold standard to detect CSF.
Management of urinoma
Once we established the adverse event as urinoma, the patient was transferred to the urology department to undergo a percutaneous CT guided urinoma drainage with drain insertion, along with an endoscopic approach with a ureteropyelography, a double J and a urinary catheter insertion. At the same time, IV antibiotics were prescribed.
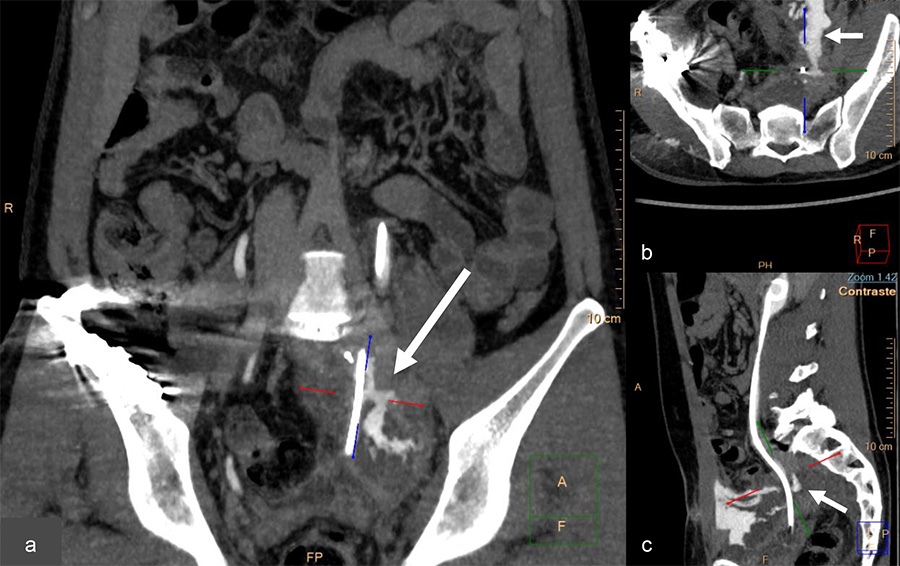
The uroscanner confirmed a left distal ureteral punctiform injury, detecting a filiform leakage (Fig. 2).
On postoperative day 12 after the ALIF procedure, the patient was discharged with no symptoms—no pain, no fever, and normal micturition and biology. But on day 20 after the ALIF procedure, the patient again came back to the ER because of suspect ted leakage through the abdominal cutaneous scar.
A new uroscanner reported a pelvic ureter fistula associated with a large recurrent subperitoneal urinoma (Fig. 3). This time he underwent a left ureterovesical reimplantation by a laparotomy approach, associated with IV antibiotics.
The postoperative period was unremarkable, and he remained apyretic. Bowel movement resumed quickly, and the drain was removed two days following the surgery. Finally on day 26 after ALIF surgery, the patient was definitely discharged from the hospital.
Systematic ureter identification and collaborative approach needed
As mentioned, anterior approaches to the lumbosacral spine have gained popularity in the last few decades and have become a versatile surgery used in various indications. ALIF approach can provide several advantages over posterior approaches, such as muscle sparing, blood loss reduction, and earlier patient discharge. However, as we also experienced, the potential for complications remains.
While ureter injuries during ALIF remain isolated cases, their consequences can be life-threatening, and spine surgeons and patients should be aware of this specific risk. We advocate for systematic ureter identification during the procedure to avoid excessive traction or sharp instrument dissection. A preoperative ipsilateral ureteral stenting of the homolateral ureter could be helpful, especially in patients with previous abdominal surgery. It could facilitate its identification, through palpation, avoiding any excessive traction or aggressive dissection around it. The management of such ureteral injuries should imply a collaborative approach including the urology team. Long term outcomes are optimal if the complication is identified in a timely fashion.
References
- Leroy HA, De Buck P, Marcq G, Assaker R. How to manage a ureteral injury after anterior lumbar spine interbody fusion surgery. Neurochirurgie. 2023 Nov;69(6):101503.
About the authors:
Henri-Arthur Leroy MD, PhD, is an associate professor at the University Hospital of Lille, dedicated to spine disorders. He followed an international curriculum in France, Switzerland (CHUV) and USA (Weill Cornell NYC, Miami University). Henri-Arthur is specialized in minimally invasive approaches, endoscopy, and robotic assisted surgery. He operates on degenerative spinal conditions (herniated disc, narrow spinal canal, osteoarthritis), tumors (metastases, chordoma, schwannoma, meningioma), trauma (fracture/compression), and deformities (scoliosis). Leroy’s research topics include intraoperative imaging in neurosurgery, advances in spinal surgery, such as minimally invasive, robotics, and artificial intelligence
Pierre De Buck is currently a 5th-year medical student at the Catholic University of Lille in France. Since his first steps in an OR at the age of 15, he has become passionate about surgery.
Between his books and training periods in the hospitals, he is currently devoting himself to his studies, preparing for the competitive examination that will enable him to choose his future specialty. By October 2025, he should become a resident in surgery.
You can find out more about his past and ongoing projects here.
You might also be interested in:
AO Spine Guest Blog
More insights directly from the community in the latest in spine care and in spine research.
AO-GO Guideline for using osteobiologics
The new AO Spine Guideline for using Osteobiologics in Spine Degeneration (AO-GO) in Anterior Cervical Discectomy and Fusion Surgeries (ACDF) helps overcome barriers associated with osteobiologic use.
ALIF, LLIF or OLIF?
Watch the interactive webinar recording about ALIF, LLIF, and OLIF with Pedro Berjano.

AO Spine Courses and Events
Use the practical AO Course Finder to select your next AO Spine educational event.