Surgical simulation—monitoring the market for better learning outcomes
BY AO SPINE EDUCATIONAL STRATEGIES TASK FORCE

Surgical simulation technologies have become a standard feature of most courses delivered by AO Spine. They allow learners to practice their surgical skills at no risk to patients. But simulation also has its limitations. Therefore, AO is continuously assessing the available options and solutions in order to provide course participants with the best learning materials on the market. Here, the AO Spine Educational Strategies Task Force gives an overview of the current status of such tools and their pros and cons.
For orthopedic surgeons, and especially for those colleagues who are still in training or relatively new to their profession, practical experience and hands-on training at the surgery table are not just invaluable, they are indispensable. However, this carries an inherent dilemma: a fruitful learning process involves—and some would even say: requires—mistakes. As a result, training on real patients is out of the question for obvious reasons.
This is why surgical simulation has come to play a crucial role in terms of training. Through different means, simulation recreates as closely as possible situations that surgeons are likely to encounter when performing operations under real-world conditions. It allows them to practice and refine their surgical skills, hone their techniques, internalize correct procedures, and receive qualified feedback from supervisors. Perhaps most importantly, simulation technologies provide a safe environment for surgeons to learn from their mistakes—at zero risk and without any consequences to patients.
Simulation can also be utilized to prepare surgeons for less common situations that do not occur very often in clinical practice. And, apart from surgical procedures themselves, simulation can very effectively teach trainees about the roles they are to assume in the context of operating as part of a team and help them focus on important cognitive skills such as problem-solving, decision-making, or team behavior.
Among the simulation technologies most commonly in use today are dry bone models and enhanced versions thereof, synthetic anatomical models, human anatomical specimens (HAS), tele-mentoring, virtual reality (VR), and augmented reality (AR).
Surgical simulation in AO Spine courses
However, useful as it may be, simulation-based surgical skills training still has its limitations. For instance, most training courses delivered by AO Spine use dry bone models without any soft tissue or HAS. While dry bone models are anatomically correct, they do not mimic the soft tissue environment or provide realistic haptics, both of which are essential when it comes to learning how to correctly handle surgical instruments. HAS meanwhile are costly, vary in quality, and may not be available everywhere. Also, while trainees who practice on dry bone models or HAS will receive individual feedback from course faculty, neither of the two methods is equipped to collect data to enable more objective assessments.
More modern simulation options such as VR and AR may offer better ways to train surgical skills and to gather performance data. This may be especially the case when it comes to remote trainings through digital channels, which many people are now much more familiar with as a result of the COVID-19 pandemic. However, the current state and limitations of these options have not been examined thoroughly enough and more research is needed.
Assessing the status quo
We want our course participants to be able to acquire new skills as effectively as possible and are constantly striving to enhance our teaching as well as our learning methods. To this end, we are engaging in an ongoing process to identify and evaluate all available simulation technologies with the aim to answer the questions most relevant to trainings we provide.
In order to structure our assessment process as much as possible, we collect data and feedback in a dedicated template. This gives us an overview over the most relevant aspects of each type of simulation, such as main features, advantages, and limitations. For each option, we collect data on the procedures it covers, the degree of realism it offers, the opportunities it provides in terms of assessment and recording and the kind of feedback and performance data it provides. We also look at cost and scalability and examine the potential uses it could have in terms of our courses and curriculum. What follows is an overview over our initial findings.
Dry bone models and enhanced versions
Artificially produced dry bone models have long served as the standard simulation option for many basic practical exercises. They can be easily procured and transported and can be used to practice for a variety of procedures including spine fixation, ligamentotaxis, scoliosis derotation, and deformity correction.
Dry bone models are anatomically correct and can mimic certain fractures or pathologies. For more unusual pathologies, customized models can be 3-D printed in small numbers. Many of the models available offer a very high degree of realism, both in terms of patient tissue as well as with respect to the haptics of the surgical instruments.
At the same time however, one of the main disadvantages of many dry bone models is the fact that they do not simulate critical soft tissues. Some options therefore feature additional layers of artificial soft tissue, allowing them to simulate, to a certain extent, intraoperative conditions. Other models are specifically designed to simulate minimally invasive procedures and interventional procedures that depend on accurate imaging, for example x-ray. Some options also feature built-in sensors or cameras to enable objective, data-based performance assessments.
Full trunk models mimic the spine in its entirety as well as ligaments, dura, muscle, and skin. They allow for an even more realistic simulation.
Synthetic anatomical models and enhanced versions
Synthetic anatomical models achieve a close approximation of the bone structures of the spine. They can be used to simulate procedures including lumbar and cervical spine decompression and fusion, microdecompression, and dural tear repair.
Because they feature skin, muscle, ligaments, dura, and cerebrospinal fluid, the simulation experience fostered by synthetic anatomical models can reach high degrees of realism and fidelity. Some models can also be set up to simulate emergency situations. Some models also offer features for assessment and feedback options—however, these are typically more expensive.
Telementoring
Telementoring systems are used to establish video connections between remote locations and exercise rooms, laboratories, or even real operating theaters. They utilize a combination of hardware and software to allow tutors, expert surgeons, or faculty members to provide guidance to trainees and share skills and knowledge with them from anywhere in the world in real time.
Some telementoring solutions rely on virtual reality headsets, while others use augmented reality technology. Telementoring is potentially less costly than other simulation technologies. The main disadvantage is the fact that the approach offers only a limited degree of realism. In terms of assessment options, all sessions can be video recorded to allow for subsequent visual feedback.
Virtual reality (VR)
VR technology combines software and hardware to provide an immersive simulation experience. Trainees wear a headset and hand controllers, which provide visual and aural cues as well as force feedback. Studies have found that surgeons with previous VR training potentially perform faster on some procedures than those without. Some surgeons also show higher post-intervention scores on procedural checklists and can place implants more accurately.
VR training is generally received positively by trainees and is less costly than many other simulation options. It can also be transported relatively easily. A wide variety of applications allows trainees to practice procedures, train on anatomical models or convene and learn together in a virtual classroom, independent of their actual locations in the real world.
The disadvantages include the fact that VR is somewhat lacking in terms of realism. The haptic feedback is also still very basic and can hardly be compared to the haptics provided by dry bone or synthetic anatomical models or specimens.
VR technology can be a very useful tool for early learners. It is also effective in terms of introducing procedures to trainees or new procedures to groups of experienced online learners.
Augmented reality (AR)
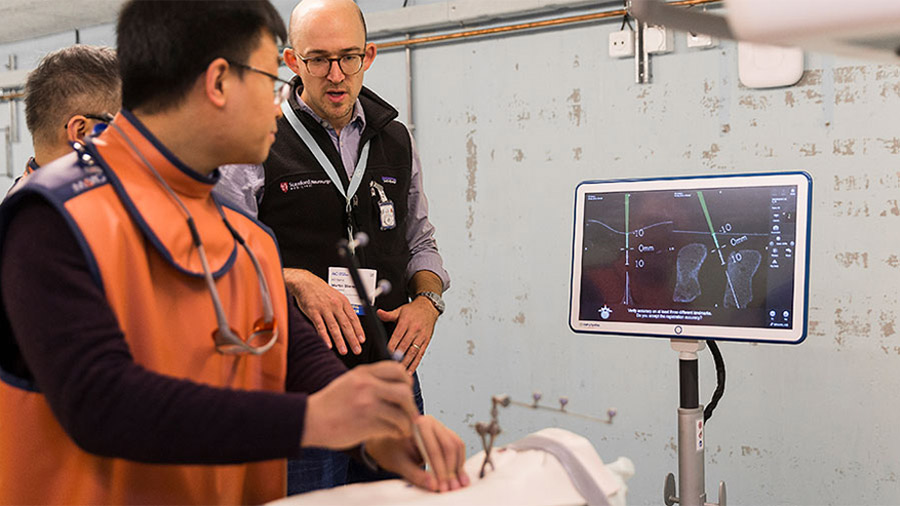
AR employs digital technology to project virtual images onto a person’s view of the real world, thereby adding computer-generated details to what is physically present. For example, it can be used to teach trainees how to navigate the placement of implants onto the spine in real time.
The realism of the method is directly dependent on the kind of materials used to represent patient tissue. At the same time, AR is capable of providing very good real-time feedback in terms of placement trajectory: trainees are able to see instantaneously where they are placing the implants. At the same time, data on implant placement accuracy is recorded for subsequent review.
AR technology has also previously been applied in real-world spine surgery in the form of a heads-up display in the positioning of pedicle screws. It has also been used in deformity surgery, kyphoplasty, and vertebroplasty. Studies suggest that the approach has certain benefits in terms of improving surgical outcomes.
Studies suggest that the use of AR technology in motor skills training makes either no difference or improves performance in comparison with traditional techniques. Regarding procedural time, the data tends to suggest that the use of AR is slower than traditional techniques.
AR is a promising technology that could potentially feature more prominently in AO Spine courses in the future. However, several aspects remain to be defined in this regard.
Looking ahead
To provide a structured approach to the assessment of new simulation technology and products, the authors are continuously collecting a range of new information about various products, including procedures covered, realism regarding patient tissue, instruments, and imaging and potential uses at AO Spine events and in the curriculum. Results of this ongoing effort will be published in a White Paper in due course.
About the AO Spine Educational Strategies Task Force:
The Educational Strategies Task Force allows AO Spine to develop and offer innovative educational programs on a variety of platforms to meet the changing needs of our members. The above article is based on the work of task force members Steven Theiss, Alaa Ahmad, Alpaslan Şenköylü, Muzahem Taha, Luiz Gustavo, Jose Manuel Ignacio, and Harry Gebhard who recently collated information on current options and trends in simulation along with the current evidence. A white paper examining the types of simulation technology has been published to support the work of the AO Faculty.
Find out more about the AO Spine Education Task Forces here.
Further reading and resources:
- Yanni DS, Ozgur BM, Louis RG, Shekhtman Y, Iyer RR, Boddapati V, Iyer A, Patel PD, Jani R, Cummock M, Herur-Raman A, Dang P, Goldstein IM, Brant-Zawadzki M, Steineke T, Lenke LG. Real-time navigation guidance with intraoperative CT imaging for pedicle screw placement using an augmented reality head-mounted display: a proof-of-concept study. Neurosurg Focus. 2021 Aug;51(2):E11. doi: 10.3171/2021.5.FOCUS21209. PMID: 34333483.
- Cofano F, Di Perna G, Bozzaro M, Longo A, Marengo N, Zenga F, Zullo N, Cavalieri M, Damiani L, Boges DJ, Agus M, Garbossa D, Calì C. Augmented Reality in Medical Practice: From Spine Surgery to Remote Assistance. Front Surg. 2021 Mar 30;8:657901. doi: 10.3389/fsurg.2021.657901. PMID: 33859995; PMCID: PMC8042331.
- Bernardo A. Virtual Reality and Simulation in Neurosurgical Training. World Neurosurg. 2017 Oct; 106:1015-1029. doi: 10.1016/j.wneu.2017.06.140. PMID: 28985656.
- Williams, M. A., McVeigh, J., Handa, A. I., & Lee, R. (2020). Augmented reality in surgical training: a systematic review. Postgraduate medical journal, 96(1139), 537–542.
You might also be interested in:

Upcoming AO Spine courses
Check out all upcoming AO Spine courses in your Region and beyond. Use the filters and free word search (e.g., “simulation”) to find courses that match your interests.
About AO Spine Education
Explore the various educational programs and resources available to our community and find out more about the three educational task forces.
Improving skills and confidence
How high-fidelity training simulator for minimally invasive lumbar decompression increases working knowledge and technical skills among orthopedic and neurosurgical trainees.