Incidental lumbar durotomy—accidental tears in the dura mater that result in leakage of cerebral spinal fluid (part 2)

About the article: This article covers the second half of the webinar on “Accidental tears in the dura mater that result in leakage of cerebral spinal fluid”. The first part of the Expert Advice Forum discussion on Incidental lumbar durotomy is available here.
These articles are part of a series covering six less formal conversations from the AO Spine Clinical Expert Advice Forums. The articles can be read on their own or as a supplement when viewing the recorded webinar.
Download the related White Paper on Accidental tears in the dura mater that result in leakage of cerebral spinal fluid (June 2020).
Speakers are identified first by full name and then by their initials. The corresponding time in the video is included in parentheses.
Watch the recording of the full webinar:
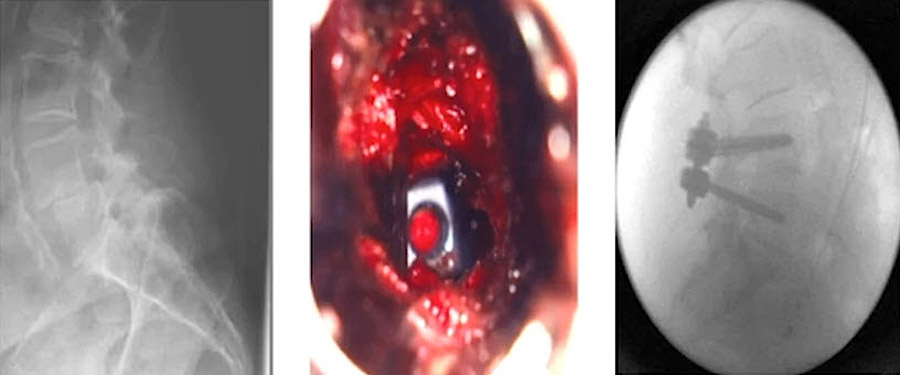
MIS TLIF—minimally invasive transforaminal lumbar interbody fusion
Bastian Storzer (BS) (36:50) introduced the topic of incidental durotomy (ID) in MIS TLIF with detailed slides.
BS (37:35): In MIS TLIF, the type of decompression is the key!
- You can do the decompression laterally, so you take out the outer part of the facet and leave the inner part, so you only see the root.
- Or you can do the inner part and decompress over the top.
- Or you can do a facetectomy and the inner part.
- Or you can go by the midline in MIS TLIF. It depends. That’s where you do your cage in as well.
- Do you do it from lateral by resecting the facet?
- Or do you do it medially, your TLIF? Then you have a higher incidence of durotomy in our experience.
BS (43:20): [Starts video of clinical case.] It’s in scar tissue, and unfortunately this was at the end of the suturing. But we have a Prolene here. If possible, we have watertight suturing. You see it’s really well decompressed. It’s in the midline of the decompression defect. And now we do a patching with TachoSil in this case. Sometimes if there are big defects, we use a bovine pericardium which holds really well. We have had no revision surgery for that up to now, after using it for one year. But I only use it in great defects. Otherwise, we do it with a patch.
S. Rajasekaran (SR) (44:45): What would you do if the dural tear is more anterior?
BS (44:50): That depends. Normally I would take a dural patch, let’s say TachoSil. Try to get it around the dura. In extreme cases you can open the dura from dorsally and go to anteriorly, but that’s pretty annoying.
How to avoid CSF leakage during decompression and cage placement
Asdrubal Falavigna (AF) (45:35) presented detailed slides on how to avoid CSF leakage during decompression and cage placement.
AF (47:15): By taking a far lateral approach, we stay away from the dura, and the dura mater is also protected by the yellow ligament. So here, I show just the exit root, the nerve crossing. And just to show some decompression and the cage placement, without seeing any dura, just yellow ligament.
Yoshiharu Kawaguchi (YK) (48:10): (When asked for helpful tips.) I think incidental durotomy frequently occurs in the large cage re-operation case. The re-operation is very difficult and very dangerous. So, if you remove the bone and the ligament […] between the dura and the soft tissue you must remove it very carefully.
Michael Wang (MW) (49:10): (When asked for helpful tips.) Fortunately, these are relatively uncommon injuries. We are seeing them more and more as people are coming lateral and oblique with OLIF and of course with ALIF. Since the approach is so small, we rarely see this. Which is fortunate since these are very difficult if not almost impossible to repair. Almost nobody has a video of this because we rarely use the microscope or endoscope for this type of approach.
BS (50:10): I totally agree. It’s really, really seldom as most of the time you leave the ligament intact
Dural sealants: types, uses, and cautions
André Castilho (AC) (50:45) presented detailed slides on dural sealants.
AC (52:50): I will highlight some of the particularities of these agents. In the hemostatic group (Tisseel, Evicel, TachoSil, Bioglue) we have to keep in mind that none of them are FDA approved for neurosurgery. They are all designed for cardiovascular or general surgery. The ones that have bovine protein in their bases—especially Tisseel that has a protein—can lead to allergic reactions and also anaphylactic shock. The ones that are human plasma-derived can be virus transmitters. There is no case in the literature reported, but we have to keep that in mind.
AC (53:40): We have something called burst pressure. That is the intradural pressure that leads to leakage in the sealant, that ruptures the sealant. With Tisseel, we have the lowest burst pressure. We have a high burst pressure with TachoSil. Bioglue has an intermediate burst pressure. We have to remember that the fiber content tells us it can be cytotoxic, especially neurotoxic.
AC (54:10): The Polyethylene glycol (PEG) group (Duraseal, TissuePatch) is FDA approved for use in neurosurgery. They have high burst pressure. They rapidly adhere to the dura. When we use Duraseal and Duraseal Exact, they have a fleshy color, so can easily see the covering of the defect. We also have a patch of PEG, which is TissuePatch. Baxter also developed one called Hemopatch, which is also PEG based.
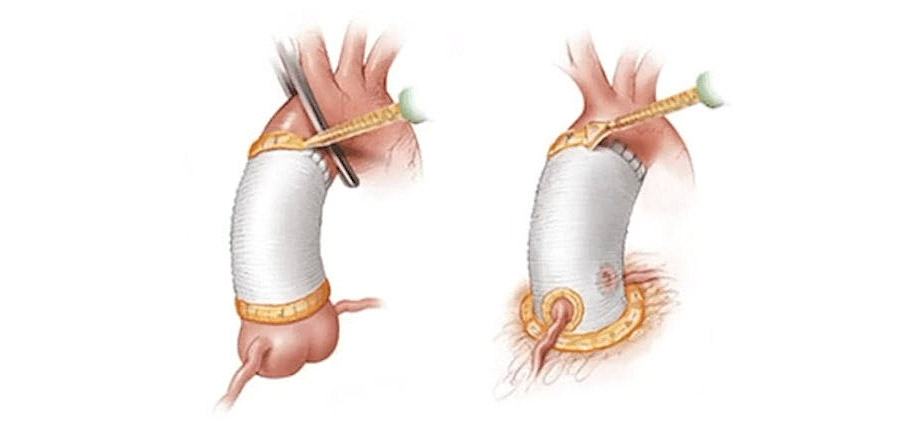
AC (54:55): In the collagen matrix, they are used as a dural substitute. We don’t have to suture most of them, just put it in and they conform to the complex surface of the dura. They also have a high burst pressure. But as a patch they don’t fit everywhere, every defect. So sometimes the glues are easier to fit.
AC (55:30): Another thing important to remember, is that the PEGs (the polyethylene glycol) can swell up to 40%. So in confined places we have to be careful, as they can lead to compression in the nerve root or the dura.
Reasons for postoperative CSF leakage unnoticed intraoperatively
On the video recording Karsten Wiechert (KW) (56:50) presents detailed slides on occult tears.
The role of bed rest, lumbar drainage, and prophylactic antibiotics
Avelino Parajón (AP) (1:02:00) presented slides on CSF leak treatment strategies.
AP (1:03:00): To put the patient on bed rest is probably the easiest way to treat a CSF leak. I think this is probably the first part of our treatment, always […] (1:03:35) However, in the literature there’s no real consensus on how long the patient must stay in bed.
AP (1:07:00): Lumbar drain should be set up to drain as much volume as the patient can tolerate […] Most patients have a slight headache, but is not a big problem, and can be treated with first step pain killers.
AP (1:08:20): Radicular pain can be caused by mechanical irritation from the catheter. We can see also some severe complications like this potential Pneumocephalus […] One of the best ways to prevent complications from lumbar drains is adequate training of the nurses […] If something is not going well, you can try to open it or probably you should go for re-operation.
AP (1:09:45): Another very controversial point in the treatment of CSF leaks is the use of antibiotics. We are all worried about the potential complication of meningitis. But only 11% of USA neurosurgeons consider prescribing antibiotics, even when using a lumbar drain.
Large, closed CSF collection—symptomatic and asymptomatic
KW presented (1:12:15) detailed slides on the extradural collection of CSF.
KW (1:14:20): (Shows diagnostic images.) The MRI can be quite impressive. That’s one of the cases I found in our collection here with epifascial, subcutaneous, and subfascial CSF collections. This is really up for discussion, what to do. I think the vast majority of surgeons would say “Well, if I diagnose this for some reason, then I need to take care of it.”
KW (1:14:50): However, there are patients that have been running around for quite a long time. And if you for some other reason do an MRI postoperatively and you discover a significant CSF collection, there’s a reason to go in and do another surgery. This is fine. You can also wait. But this really can be discussed.
KW (1:15:20): The surgical treatment here is obviously the most definitive way, and at least reduces the risk of complications such infections, spinal headaches, recurrence, etc. If you have an early post-operative diagnosis—I’d say within the first three months—you can drain that. But usually, the surgical treatment is something which I personally would prefer here.
Final questions:
AF (1:16:20): When we have a durotomy, do we systematically need surgical revision? How do you decide whether to do an open revision or stay in minimally invasive and try to close the dura?
AP (1:17:00): Usually you have a small dural tear when you’re using tubes. Usually, we just need a patch and don’t do anything else. It’s very uncommon to have a CSF leak outside, to have a big collection. Usually, most of the time it solves quite easily. But if you have a very big hole and you are not able to put the roots inside, probably in these cases you should convert into an open surgery. But this is quite uncommon when you’re doing MIS.
AF (1:17:55): What’s your opinion about bed rest? I usually leave the patient 24 hours.
KW (1:18:10): It depends on the size of the defect and my trust in the closure. But two days (one day flat, one elevated), up to three days depending on the sufficiency of the closure.
NT (1:18:40): Usually in an MIS approach, only 24 hours in bed rest and the next day the patient can walk. In revision, only in symptomatic patients, if medical treatment has failed. Usually if the previous surgery was MIS, maybe the revision is MIS or open. If the previous surgery was open, the revision is always open.
AF (1:19:20): Some of you use acetazolamide to reduce CSF production. I never use it. What about intravenous antibiotic when you have CSF leakage or during lumbar CSF drainage?
BS (1:19:45): Normally we use it 24 hours if we have durotomy. If we have a CSF drain, we use it while the drain is in.
AF (1:20:00): It is important every time that we use some DuraGen, open near the nerve roots. If it expands—like AC told us—sometimes it expands, and then you have this nerve root compression. I usually try to remove all things I left over the nerve root. What you’re opinion, MW? How to do a nerve root compression, while trying to close CSF leakage?
MW (1:20:45): It’s very difficult. You see it in our video. You’re distracted by all these nerves in the way, and usually you’re having to drill a lot. That’s the really unfortunate thing […] The dural tear happens at the worst possible time when you’re at the most maximal stenosis and you haven’t really got enough clearance with the bone.
MW (1:21:10): You try to clear the nerves out of the way, either with a cottonoid or a patty, and work around it. Usually trying to go lateral. Usually trying to get more facet joint off, yet not destabilizing.
AF (1:22:00): Have you had treated nerve root patients by using sealants? You try to close the open dura and you have glue. Then after surgery, patient still has nerve root irritation.
MW (1:22:35): In the USA, all the products that are on the market technically are safe for that. So, there shouldn’t be irritation. But of course, we do know that when you’re using cyanoacrylate—which is what DuraSeal is—there is a risk. And of course, there’s mechanical risk. You could stick the nerve to something else and create scar tissue. I’ve even seen cases where people sewed the nerve in with the repair. So, anything can happen. You’re absolutely right.
MW (1:23:05): But it does become this push-pull. If you remember the trials of trying to prevent scar tissue. Scar tissue is healing, fibroblast action. So, all those products that try to limit scar also limit healing. So, we really are stuck at this homeostatic plus/minus. The stronger something scars or irritates, the better the sealing. Then the weaker it is for that, the weaker the repair.
MW (1:23:30): The classic example is when you use GORE-TEX, very synthetic, that is very non-reactive, not very biologic. It doesn’t irritate the nerves on contact or anything. But on the other hand, to get it to heal to the dura—to scar down—is the most difficult. This is this classic spine problem. It’s all push-pull. You want the stuff that doesn’t irritate, but you want the stuff that irritates enough, or creates enough inflammation, so that you do get fibroblast growth.
MW (1:23:57): I think it’s an opportune area. I’m curious to see what Baxter’s coming out with, with this new […] it’s like a glue. You just glue and then stick the membrane down and hopefully it holds. We’ll see. I don’t know. So far, we don’t have an ideal solution.
AF (1:24:10): What’s the panel opinion about using a drain? Postoperative if you have CSF leakage? 2 or 3 days? Or not?
YK (1:24:35): I usually put the drain for 2 days after surgery. Gravity, no pressure. In case of CSF leak.
AC (1:25:10): I also leave it for 48 hours without any pressure. So, there is no dead space. And the liquid doesn’t impede the dura to heal.
KW (1:25:30): If possible, I would refrain from using the drain altogether. Sometimes, if there’s still a lot of oozing, then yes it helps. And then no suction, gravity only. But, if possible, omit the drain.
AF (1:25:50): How much CSF can you drain in one hour or in one day?
AP (1:26:20): Usually for CSF leaks, we don’t have to pay much attention to the amount. Some say 15-20ml per hour, something like that. I think you have to drain as much as the patient can tolerate. If the patient only has a slight headache and can easily handle that, that’s the perfect situation. Because obviously, you are going to use if for just a few days.
AF (1:27:00): Thank you. I think we’re going to wrap up this webinar.
The first part of the Expert Advice Forum discussion on Incidental lumbar durotomy is available here.
Download the White Paper on Accidental tears in the dura mater that result in leakage of cerebral spinal fluid (June 2020).
Find more Clinical Expert Advice Forums titles here.
About the authors:
The AO Spine Clinical Expert Advice Forums address clinical situations where clinicians can benefit richly from the experience of experts, but rigorous scientific research may not be possible. These forum rounds resulted in six White Papers and webinars in 2020 –2021. The webinars include detailed slides to support the conversations.
The Clinical Expert Advice Forum for “Incidental lumbar durotomy" are Asdrubal Falavigna (Brazil), André Castilho (Brazil), Yoshiharu Kawaguchi (Japan), Bastian Storzer (Germany), Karsten Wiechert (Germany), Nestor Taboada (Colombia), Jason Ilias Liounakos (USA), Michael Yung-Shun Wang (USA), Avelino Parajón (Spain), and S. Rajasekaran (India).
Disclaimer
The articles included in the AO Spine Blog represent the opinion of individual authors exclusively and not necessarily the opinion of AO Spine or AO Foundation.