Patient is on the mend following first-in-human application of Biphasic Plate
A 64-year-old German patient is on the path to what his surgeon believes will be fast, robust bone healing, after having the newly CE-marked Biphasic Plate DF (distal femur) implanted to repair a complex floating knee injury.
The Biphasic Plate DF—made possible by the AO Innovation Translation Center (AO ITC) Technology Transfer—is a new solution devised by the AO Research Institute Davos (ARI) in Switzerland, Queensland University of Technology (QUT) in Brisbane, Australia and 41medical AG as manufacturer. With Development Incubator resources from AO ITC, the development phase of the distal femur version started in 2018; CE certification as a class IIB medical device was granted in April 2021.
The first-in-human application of the device took place on March 9, 2022, by Christoph Sommer, MD, chief trauma surgeon at Kantonsspital Graubünden in Chur, Switzerland. Sommer is chairperson of the AO Technical Commission’s Lower Extremity Global Expert Committee and is an AO faculty member for more than 30 years.
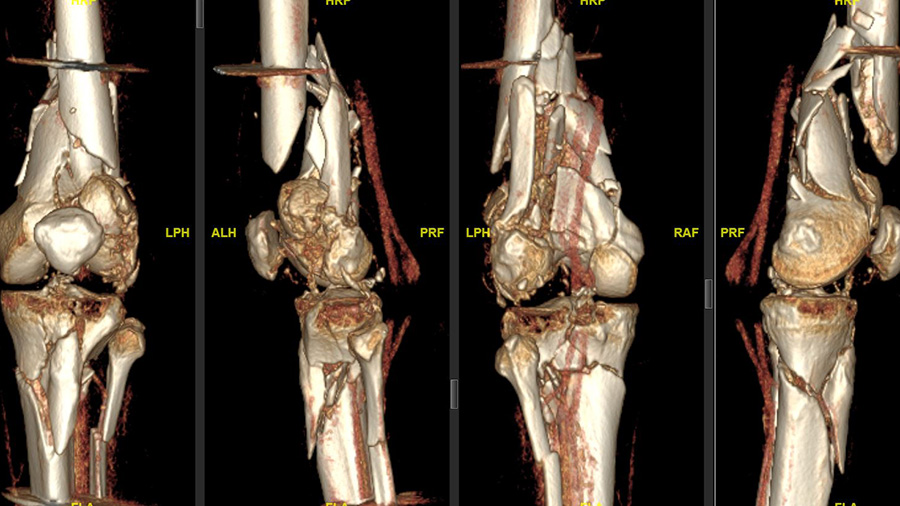
“The patient was driving a car while on holidays in Mexico and was hit from the left side. He had serial rib fractures, a nasty, open fracture of his left elbow, and an open, complex floating knee injury, a comminuted distal femoral fracture, and a proximal tibial fracture on the left side as well as a proximal tibial fracture on the other side,” Sommer explains, noting that after about two weeks of care in Mexico, the patient was flown back to Switzerland by Rega Swiss Air-Rescue. “He arrived at our hospital with an external fixator on his left knee and elbow, and was in generally good shape. First, my colleague fixed his elbow and right tibia; and, unfortunately, the patient had also an injury to his left radial nerve that had to be reconstructed.”
Strong and durable—allowing optimal motion
It was immediately clear to Sommer that the left knee injury required open reconstruction and plate fixation.
“The knee needed better reduction and stronger fixation than just this joint-bridging external fixator, which was quite clear. I think the biggest risk without this surgery would have been intra- and extraarticular nonunion of the femur because it was a multi-fragmented and open fracture,” Sommer says. “The goal, of course, was to stabilize both legs and bring all fractures back to healing and functioning as well as they were before the accident: intraarticular congruency with well-aligned bones (correct length, rotation, and axis), and a moveable, stable, and hopefully pain-free joint.”
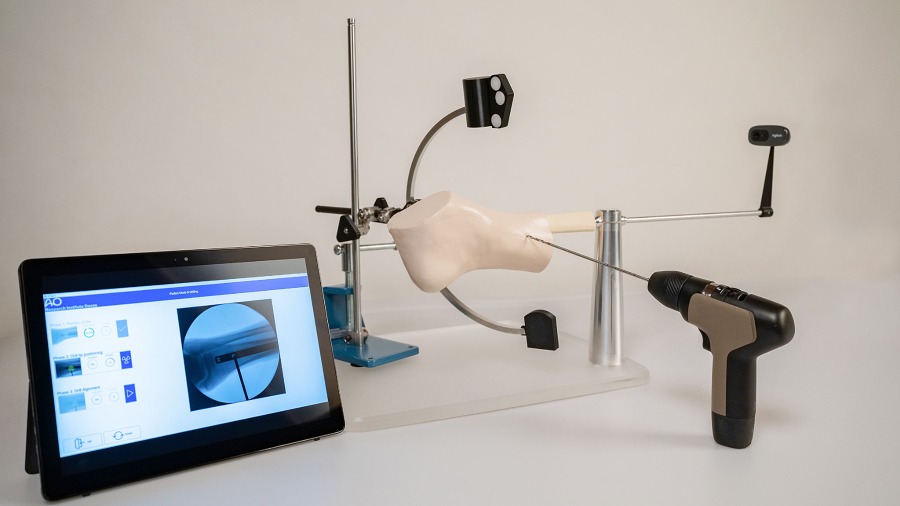
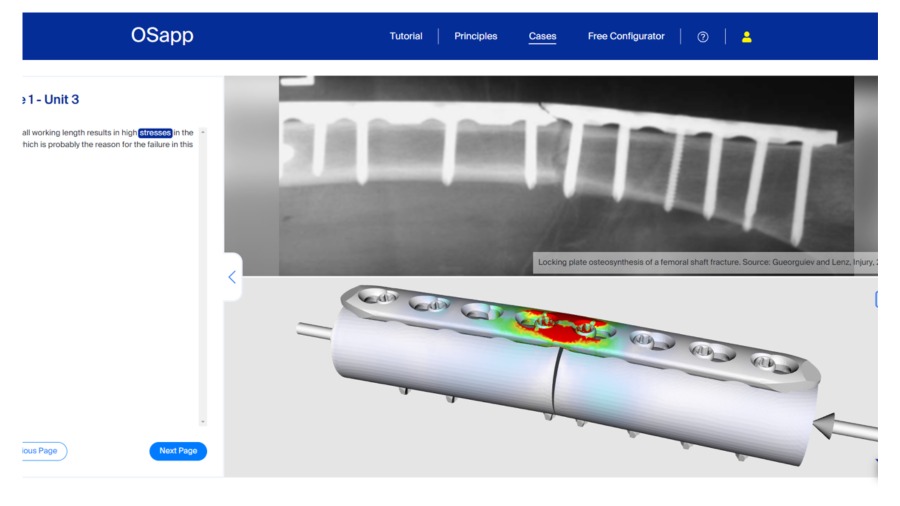
Sommer says he chose the Biphasic Plate DF because it not only allows bridging between the joint and the shaft, but also seems to be a durable implant without plate failure before bone healing
“The bridging construct has been proven by animal experiments, and the plate is strong and durable,” he says, noting that at the same time the Biphasic Plate DF allows for a certain degree of motion, which is an advantage and promotes the callus formation essential to fracture stabilization. In contrast to conventional plates, the biphasic plate due to its specific design allows for a defined motion of the fractured site while avoiding too much motion by loading. Overloading should not occur.
“That’s why I think it’s a good implant, especially for this case, where I expect a long healing time due to the high impact by the initial trauma and the delayed presentation to us” says Sommer.
Following the four-hour and 15-minute surgery and a second surgery a week later to correct a valgus misalignment at the tibia level, the patient was at the Kantonsspital Graubünden for 11 additional days before being transferred to a rehabilitation center near Zurich.
“So far, his rehabilitation is going well. He starts walking with American crutches,” the surgeon reports, stating that he highly values innovations, like the Biphasic Plate DF, which improves patient outcomes. “Innovation is very important. Twenty years ago, I thought, ‘Oh, we can fix everything. We have our implants, so we don’t really need new solutions,” he says. “But now we have completely different implants than we had 20 years ago. Innovation, for me, is a new product or technique that adds value for our patients—and that value is what makes the difference. The AO's Development Incubator is a valuable resource for people around the world to find support for their really innovative ideas and bring them to market.”
‘The reason I do this work’
For ARI’s Markus Windolf, coinventor of the Biphasic Plate DF, the first-in-human application of the solution was an exciting event.
“The prospect that this solution could speed up patient recovery and restore the quality of life is really the reason I do this work,” says Windolf, ARI’s Deputy Program Leader Biomedical Development, Focus Area Leader Concept Development, and inventor of 16 international patents.
“It has always been my wish for an idea that came out of my head to reach clinical practice—reach the patient—and this is the first time that has happened with the Biphasic Plate DF. It was a long journey and the first-in-human application is very satisfying for me. This is what I always wanted to achieve when I went into health care as an engineer,” he says. "Nonetheless, we have to remain realistic here. This is only the first patient. Time will show if the Biphasic Plate can create a real benefit in trauma care."
Windolf visited the patient during his stay at Kantonsspital Graubünden.
“The patient was pleased that I had visited to ask how he was doing,” Windolf says. “I had the chance to explain the principle of the plate to him. He seemed proud to be the first patient in the world to have had this plate implanted. After explaining it to him, he sounded pretty confident that it could do some good in his case.”
Biphasic Plate DF coinventor Devakar Epari echoes Windolf’s sense of satisfaction that—years after he and Windolf first discussed the plating concept during their 2014–2015 fracture healing research collaboration at QUT—the plate is now contributing to a patient’s recovery.
“It feels amazing, and it is certainly the most significant professional contribution that I’ve made which spans teaching, research, and innovation,” says Epari, an associate professor of biomedical engineering at the QUT School of Mechanical, Medical and Process Engineering. “I feel a great sense of satisfaction that my work, and not only the Biphasic Plate DF but the many years of research before it, is having a real impact.”
Going forward, the development team will continue to support clinicians in using the Biphasic Plate DF to collect data to determine the extent of benefits it provides to patients, with an eye to scaling up and demonstrating that the concept can address other anatomical areas, such as the lower tibia or the upper arm.
“We are proud to support this project and the excellent project team with the AO's Development Incubator,” says Roland Herzog, Head of the AO ITC’s Technology Transfer. “It is by innovations like the Biphasic Plate DF that we can support the AO mission of promoting excellence in patient care and outcomes in trauma and musculoskeletal disorders."
Can your idea improve patient care or surgeon education?
References
1. Hofmann-Fliri L, Epari DR, Schwyn R, et al. Biphasic Plating—in vivo study of a novel fixation concept to enhance mechanobiological fracture healing. Injury. 2020 Aug;51(8):1751–1758.
2. Epari DR, Gurung R, Hofmann-Fliri L, Schwyn R, Schuetz M, Windolf M. Biphasic plating improves the mechanical performance of locked plating for distal femur fractures. J Biomech. 2021 Jan 22;115:110192. doi: 10.1016/j.jbiomech.2020.110192. Epub 2020 Dec 24.