Journey of the Smart Digital Solutions Task Force (SDSTF)
Formed as a key initiative of the AO Technical Commission, the Smart Digital Solutions Task Force (SDSTF) vision was to enhance the patient journey in trauma care through the integration of advanced digital technologies. From 2019 to 2024, the group (Fig 1) has transitioned from assessing existing digital technologies to establishing new strategies for wearable-based outcome measurement. This article highlights the key milestones and contributions of the SDSTF.
The group’s commitment to knowledge dissemination has resulted in numerous presentations at prestigious conferences such as ICORS, EORS, ORS, DKOU, OTA, and AAOS. Their work has also been published in prominent journals, such as Injury and EFORT Open, contributing significantly to the academic and clinical discourse on digital solutions in orthopedic trauma.
Fig 1 Members of the Smart Digital Solutions Task Force with guests at their final meeting in Hamburg during the EFORT Annual Meeting in 2024. From left: Sureshan Sivananthan (member), Andrew Hanflik (consultant), Bernd Grimm (member), Meir Marmor (member), Benedikt Braun (chairperson), Ursi Styger (AO TC Manager), and Boyko Gueorguiev (ARI guest). Peter Richter (member) is missing on the photo.
From assessing existing technologies
One of the first major goals of the SDSTF was to evaluate the available digital technologies and their potential applications in orthopedic trauma surgery. This effort culminated in the publication of the 2020 Finding NEEMO white paper, which outlined how current digital solutions could meet the needs of orthopedic trauma surgery. The NEEMO framework (Fig 2: Need, Ease, Environment, Modularity, Ownership) was introduced to guide the development and application of new digital technologies in the field [1].
Fig 2 Need Ease Environment Modularity Ownership (NEEMO). A guiding framework to aid developers, researchers, and clinicians when using digital solutions to address their needs.
To Analyzing: systematic review and survey
During the COVID-19 pandemic, despite the challenges of limited physical meetings and restricted research capabilities, the SDSTF undertook a comprehensive systematic review of studies on wearable activity monitors used in fracture management over the past decade. From more than 2000 identified studies, 136 were analyzed, focusing on technology, treatment, outcomes assessed, and general usability characteristics. This study was presented at the DKOU and SICOT annual meetings and published in the Indian Journal of Orthopaedics [2].
In addition, the SDSTF and AO Trauma conducted a survey with more than 400 respondents to analyze the current use and future needs for wearable technology in orthopedic trauma. This survey revealed that smartphones are the most widely used wearable system for measuring general patient activity. It also identified key outcome parameters, such as general patient activity, kinematic and kinetic gait parameters, and general gait analysis. The results of this survey were published in the journal Injury and presented at national and international conferences, highlighting the clinical relevance and potential of wearable technologies [3].
To defining: BYOD study and new strategies
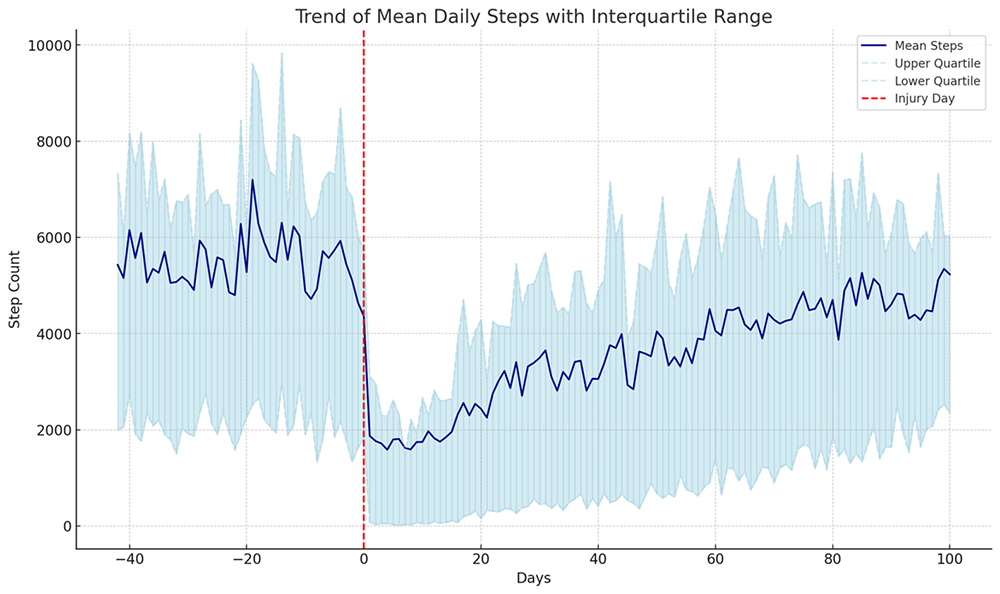
Building on insights gained from their initial assessments and surveys, the SDSTF launched a pioneering feasibility study known as the Bring Your Own Device (BYOD) study. This study aimed to evaluate the effectiveness of patient-owned smartphone and wearable technology in tracking functional recovery from pre-injury to post-injury. By analyzing daily step counts normalized to each patient’s pre-injury maximum, the study successfully visualized the recovery trajectory of patients from pre-injury to full recovery (Fig 3).
Fig 3 Example of the recovery journey as tracked with the individual patient step count from pre-injury (left of the red dashed line) to post-injury (right of the red dashed line). Mean step counts and interquartile range are shown for a cohort of more than 100 orthopedic trauma patients, providing a clear visualization of the recovery process.
The BYOD study demonstrated the feasibility of using personal wearable devices to assess functional recovery and showed significant potential for predicting recovery outcomes. In addition to tracking recovery, this approach enabled early identification of patients at risk for prolonged healing, as demonstrated by a logistic regression model used in the study. The results were published in an AO special issue of Medicina and further discussed in Injury [4; 5].
Challenges and future directions
The SDSTF identified several challenges to the widespread adoption of wearable technology. Key barriers included cost, data validity, patient compliance, and the need for standardized parameters for clinically relevant outcomes. The group emphasized the need for further research to resolve these issues, particularly in understanding baseline wearable data in relation to physical function and exploring the potential of different wearable systems from other medical fields. To address these challenges members of the group have begun collaborative projects together with the AO Technical Commission’s Upper Extremity Global Expert Committee (UEGEC), and the Elbow Task Force (EBTF) to advance the process of creating a comprehensive digital outcome parameter.
The SDSTF’s journey from 2019 to 2024 has been marked by significant achievements in the evaluation and application of digital technologies in orthopedic trauma [6; 7]. Their work has laid a strong foundation for future research and development and made substantial contributions to the field. Their experience will now culminate in and be transferred to the newly formed Trauma Digital Expert Group. So, the digital journey continues.
References
1. Braun BJ, Grimm B, Hanflik AM, et al. Finding NEEMO: towards organizing smart digital solutions in orthopaedic trauma surgery. EFORT Open Rev. 2020 Aug 1;5(7):408-20.
2. Marmor MT, Grimm B, Hanflik AM, et al. Use of wearable technology to measure activity in orthopaedic trauma patients: a systematic review. Indian J Orthop. 2022 Apr 9;56(7):1112-1122.
3. Braun BJ, Grimm B, Hanflik AM, et al. Wearable technology in orthopedic trauma surgery - An AO trauma survey and review of current and future applications. Injury. 2022 Jun;53(6):1961-1965.
4. Braun BJ, Histing T, Menger MM, et al. “Bring your own device”—a new approach to wearable outcome assessment in trauma. Medicina (Kaunas). 2023 Feb 19;59(2):403.
5. Braun BJ, Histing T, Menger MM, et al. Wearable activity data can predict functional recovery after musculoskeletal injury: Feasibility of a machine learning approach. Injury. 2024 Feb;55(2):111254.
6. Halm-Pozniak A, Lohmann CH, Zagra L, et al. Best practice in digital orthopaedics. EFORT Open Rev. 2023 May 9;8(5): 283-290.
7. Vogel C, Grimm B, Marmor MT, et al. Wearable Sensors in Other Medical Domains with Application Potential for Orthopedic Trauma Surgery-A Narrative Review. J Clin Med. 2024 May 27;13(11):3134.