Nail fixation of unstable trochanteric fractures with cement augmentation is cost-effective in different healthcare settings
Proximal Femoral Nail Antirotation (PFNA), an intramedullary implant for the treatment of unstable trochanteric femoral fractures, can be augmented with Traumacem™ V+ Injectable Bone Cement and has been the subject of recent studies. In the original publication of a large, multicenter randomized controlled trial (RCT), PFNA with cement augmentation had comparable clinical outcomes to PFNA without augmentation, although a trend toward a lower risk of mechanical complications with cement augmentation was observed [1]. To understand whether this lower risk might translate into potential cost savings, a cost-effectiveness analysis was conducted in collaboration with Christian Kammerlander, MD, Julia Schneller, MD, AO ITC Clinical Science, and DePuy Synthes. PFNA with augmentation compared to PFNA without augmentation was shown to be cost-effective in the German healthcare setting, as published in 2022 [2].
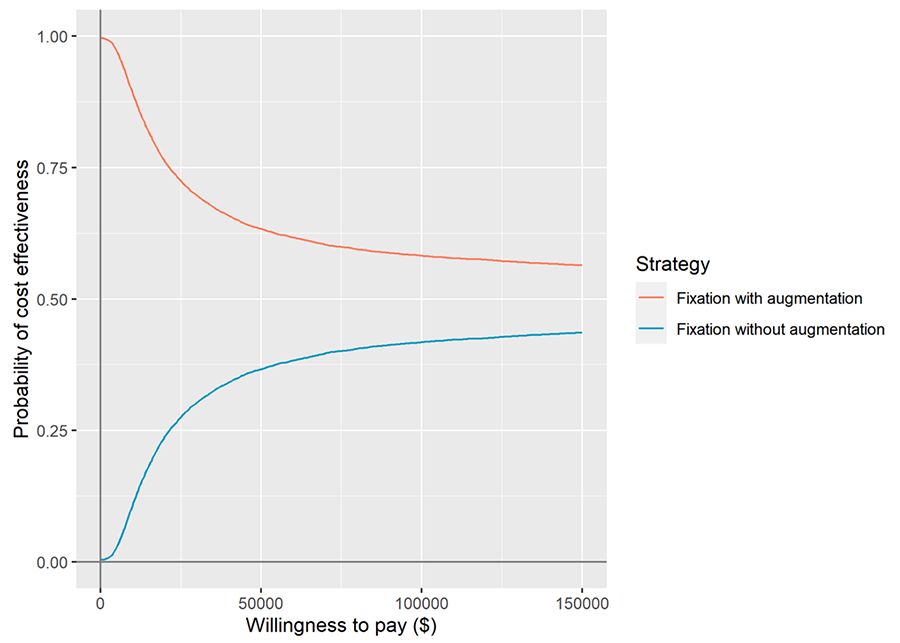
Whether similar results existed in other settings was the question that led the authors to perform a cost-utility study for the US healthcare setting, published in February 2024 [3]. The short-term decision tree model and long-term Markov model used in the German setting and the cost data were adapted to the US healthcare setting, with clinical data taken from the original RCT. Based on those data, both in the German and the US healthcare setting, fixation with cement augmentation was more cost-effective. In the US healthcare setting, a cost savings of $130,765 per quality-adjusted life-years (QALY) was demonstrated, and in the German healthcare setting, €8,821 per QALY. The cost savings in both healthcare settings were mainly driven by the prevention of additional costs due to treatment-related complications (mechanical failures).
With the current growing emphasis on value-based medicine, the results of these two recently published studies may help support surgeons in their medical decision-making and be informative for policymakers when it comes to coverage and reimbursement.
- Kammerlander C, Hem ES, Klopfer T, et al. Cement augmentation of the Proximal Femoral Nail Antirotation (PFNA) - A multicentre randomized controlled trial. Injury. 2018 Aug;49(8):1436-1444.
- Joeris A, Kabiri M, Galvain T, et al. Cost-Effectiveness of Cement Augmentation Versus No Augmentation for the Fixation of Unstable Trochanteric Fractures. J Bone Joint Surg Am. 2022 Nov 16;104(22):2026-2034.
- Joeris A, Kabiri M, Galvain T, et al. Nail fixation of unstable trochanteric fractures with or without cement augmentation: A cost-utility analysis in the United States: Cost-utility of cement augmentation. Injury. 2024 Apr;55(4):111445.