Orthognathic management of facial deformities: why surgeons and orthodontists must collaborate
BY DR MARIUS BREDELL AND DR ROLAND MÄNNCHEN

When managing patients with facial deformities, it quickly becomes clear that a single profession does not hold all the answers. Orthodontists bring the expertise of aligning teeth and shaping occlusion, while craniomaxillofacial (CMF) surgeons provide the means to correct skeletal discrepancies and restore balance to the face.
On their own, each specialty can achieve much. But when combined in a true partnership, the results for patients are transformative.
-
Read the quick summary:
- Orthodontist Roland Männchen and CMF surgeon Marius Bredell share why collaboration is essential in orthognathic care.
- Best outcomes for facial deformities require both correct tooth positioning and precise skeletal surgery in a shared patient journey.
- Surgeons gain insight into orthodontic preparation, long-term planning, and patient communication strategies.
- AO’s interdisciplinary training and AO CMF’s new curriculum are now integrating orthodontists and surgeons.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
As an orthodontist and a maxillofacial surgeon working together in Winterthur, we have seen first-hand how essential this collaboration is. Over the years, we have treated many surgical orthodontic cases jointly. What we have learned is that the best results depend not just on individual technical skills, but on a continuous exchange of ideas, shared decision-making, and a unified approach to patient care.
This philosophy is now reflected in the new AO CMF Course—Orthognathic Management of Facial Deformities. For the first time, orthodontists are fully integrated into an AO CMF curriculum, acknowledging the central role they play in preparing and supporting patients who require orthognathic surgery.
How surgeons and orthodontists complement each other
Most patients begin their journey with the orthodontist. A child, teenager, or young adult presents with crowding, malocclusion, or a noticeable discrepancy in the position of the jaws. The orthodontist’s task is to determine whether braces alone can achieve an acceptable result or whether surgical correction is needed.
In many cases, braces alone can deliver a stable and functional occlusion. But when skeletal deformities are present—such as a pronounced underbite, open bite, or asymmetry—the limitations of orthodontics alone become obvious. This is where the surgeon becomes an essential partner.
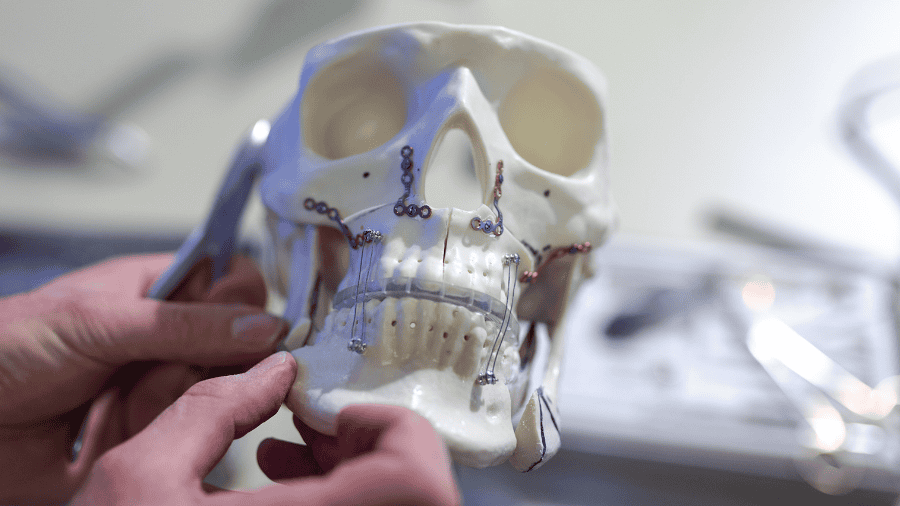
Our roles are complementary. The orthodontist ensures that the teeth are positioned correctly within the jaws so that when surgery is performed, the new skeletal alignment and the occlusion fit harmoniously. Without that preparation, the surgeon might have to choose between creating a pleasing facial profile and a functional bite—an impossible compromise. Equally, the orthodontist cannot overcome major skeletal imbalances without the surgeon’s contribution.
Only when both perspectives are integrated can we deliver a result that is both functionally sound and aesthetically satisfying.
Guiding patients through the journey
Convincing patients that combined treatment is the right path can sometimes be challenging. For those with very obvious discrepancies, the need for surgery is clear. A young patient with a significantly protruding lower jaw, for example, can see that braces alone will not correct the problem.
Other cases are less obvious. Patients may hope that orthodontic treatment alone will suffice, and it is our responsibility to explain our professional limitations and the potential consequences of not addressing the skeletal problem. Attempting to compensate with braces alone may result in unstable outcomes, compromised function, or even undesirable changes to facial appearance.
We also emphasize that surgery, while not without risk, is often less risky in the long term than leaving a deformity untreated. Malocclusion and skeletal discrepancies can lead to functional issues, pain, or aesthetic concerns that become more pronounced with age. Framing treatment as a long-term investment in health and quality of life helps patients and families make informed decisions.
Ultimately, this is a journey. Some of our patients first meet us in early adolescence, and we may not perform surgery until they reach full skeletal maturity years later. Throughout that time, it is essential that the orthodontist, the surgeon, and the patient all remain aligned and committed to the plan.
The collaborative workflow in practice
Our workflow reflects the need for seamless collaboration. Most patients arrive at the orthodontist’s office through a referral from their dentist. After an initial assessment, if surgical correction is likely to be required, we discuss the case jointly. Often this discussion happens even before the surgeon has met the patient.
The orthodontist contributes insight into tooth position and dental alignment, while the surgeon evaluates skeletal relationships and facial proportions. Together, we construct a treatment plan that integrates both perspectives.
Equally important is how we communicate with the patient. Presenting a unified message builds confidence and helps patients understand that we are guiding them along the same path, not offering competing alternatives. Cases often extend over many years, and continuity of communication is crucial in maintaining trust.
Mutual learning expands understanding
One of the most rewarding aspects of our partnership has been how much we have learned from each other. Orthodontic education, like surgical training, evolves over time. Techniques, tools, and philosophies shift, and without constant exposure to new developments, it is easy to fall behind.
By working side by side, we have both expanded our understanding. The orthodontist has gained a deeper appreciation of surgical techniques and their potential, while the surgeon has developed greater insight into orthodontic preparation and limitations. This mutual knowledge not only improves our own practice but also enables us to anticipate each other’s needs and plan more effectively.
Above all, constant communication reinforces the fact that the patient benefits most when both professions are pulling in the same direction.
Bringing professions together in AO CMF education
This collaborative ethos is precisely what the AO CMF Course—Orthognathic Management of Facial Deformities seeks to foster. For many years, orthodontists and surgeons have trained separately, each focusing on their own discipline. By bringing both professions together in a structured learning environment, the course reflects the way real-world practice should operate.
The program combines lectures, small-group discussions, practical exercises, and skills stations. Participants practice facial analysis and treatment planning, engage in interactive discussions, and learn techniques to avoid complications. The blended format also includes online precourse activities, ensuring that the face-to-face sessions can focus on deeper engagement and practical skills.
Key topics include:
- Fundamentals of decision-making in orthognathic treatment
- Multidisciplinary treatment planning
- Core treatment processes and workflows
- Patient communication and expectation management
- Strategies for avoiding complications
For orthodontists, this is a unique opportunity to explore surgical principles directly. For surgeons, it provides valuable insight into orthodontic preparation and thinking. For both, it creates a platform to build the mutual understanding that patients depend upon.
Future potential in interdisciplinary education
As we look to the future, we see enormous potential in expanding interdisciplinary education. This program is the first in AO CMF to formally involve orthodontists and orthognathic surgeons together as faculty, and we hope it will be the beginning of a broader trend.
Orthognathics and orthodontics cannot function as isolated professions. Each of us is limited when working alone. Together, however, we can achieve outcomes that truly transform patients’ lives.
The management of facial deformities is never a quick fix. It is a long journey, requiring careful planning, patient guidance, and teamwork over many years. By learning from each other and teaching side by side, orthodontists and surgeons can ensure that this journey leads to the best possible results—functional, esthetic, and lasting.
The AO CMF course represents an important step in that direction, and we are proud to be part of it.
About the authors:
Dr Roland Männchen is a private orthodontist based in Winterthur, Switzerland, where he has built a practice dedicated to comprehensive orthodontic care with a strong focus on interdisciplinary collaboration. A member of the prestigious Angle Society of Europe, he currently serves as president of the Swiss Board Examination Committee.
With decades of clinical experience, Roland has treated numerous patients requiring surgical-orthodontic management, working closely with CMF surgeons to achieve both functional and esthetic outcomes. His commitment to education and advancing best practices has led him to faculty roles at AO CMF courses, where he shares his expertise in orthodontic preparation and interdisciplinary treatment planning.
Dr Marius Bredell is a maxillofacial surgeon in private practice and at the Cantonal Hospital of Winterthur, Switzerland. He specializes in orthognathic surgery and reconstructive procedures, with a particular interest in improving quality of life for patients with facial deformities.
In his daily work, Marius collaborates closely with orthodontists to design and deliver treatment plans that combine skeletal correction with precise dental alignment. His dual commitment to clinical excellence and medical education is reflected in his long-standing involvement with AO CMF, where he contributes to international courses and promotes closer integration between orthodontics and surgery.
You might also be interested in...
AO CMF Course—Orthognathic Management of Facial Deformities
This 2-day face-to-face course—complemented with online precourse activities—provides a comprehensive introduction to the principles and core concepts of orthognathic surgery for dental and skeletal deformities.
AO resources for orthognathic surgery
Explore AO's resources on craniomaxillofacial orthognathic surgery (corrective jaw surgery). From structured curricula and educational events to clinical tools, videos, blog posts, and research.
AO CMF Global Study Club
A dynamic platform for AO CMF members to discuss cases, share experiences, and network effectively.
AO Davos Courses
Unparalleled opportunities for professional development and personal growth: enrich your knowledge, expand your professional network, and immerse yourself in the AO’s pioneering spirit at our organization’s home in Davos, Switzerland.



.png?h=506&iar=0&w=900&rev=3943d394deb34ce08765783f139a9711)