Global insights on thoracolumbar burst fractures treatment

Thoracolumbar burst fractures (AO Spine A3, A4) without neurological deficit are a common but debated clinical challenge in spine care. Despite their high prevalence and socio-economic impact, global treatment approaches vary drastically, from routine surgery to conservative care, driven more by geography and surgeon preference than by evidence.
To bring clarity to this controversy, AO Spine Knowledge Forum Trauma and Infection conducted one of the largest prospective, multicenter observational cohort studies ever undertaken on this topic. The results provide crucial insights into outcomes, cost-effectiveness, and regional trends—equipping surgeons worldwide with the evidence needed to better inform shared decision-making and treatment planning.
-
Read the Quick Summary
- A global AO Spine study compares surgical vs non-surgical care for thoracolumbar burst fractures in patients with no neurological deficits.
- Both groups improved similarly in disability scores; surgery showed a trend towards faster recovery, though not statistically significant.
- The study offers solid evidence to guide shared decisions with patients, factoring in less time off work, recovery speed, and cost-effectiveness.
- In a separate cost-utility analysis, surgical management emerged as more cost-effective, mainly due to loss of productivity within the than non-operative care group.
- A related paper on gender affects on outcomes was recently published. Upcoming analysis will offer insight into A3 vs A4 outcomes, the impact of injury morphology on outcomes, and the role of bracing.
Dvorak MF, Öner CF, Dandurand C, et al. Surgical versus Non-Surgical Treatment of Thoracolumbar Burst Fractures in Neurologically Intact Patients: A Prospective International Multicentre Cohort Study. Global Spine Journal. 2025;0(0)
Understanding thoracolumbar burst fractures
Thoracolumbar (TL) burst fractures (AO Spine types A3 and A4) without neurological deficit are one of the most common spinal fractures encountered in clinical spine practice. Affecting the thoracic and lumbar regions, they are typically caused by axial load injuries. The importance of identifying disruption to the posterior ligamentous complex (PLC) is crucial.
It is estimated that more than five million individuals suffer thoracolumbar burst fractures around the world every year, accounting for a significant proportion of surgeon’s clinical practice. As a result, spine surgeons and trauma teams routinely face decisions about their management. Moreover, these types of fractures often occur during patients’ working years and are therefore associated with significant costs, not only related to the necessary medical care, but also to the affected individuals as well as society as a whole.
Dramatic regional treatment variations
In cases where thoracolumbar burst fractures coincide with neurological impairments, the treatment algorithm is straightforward: most surgeons tend to operate, no matter where they are based. However, when it comes to the question of how to best manage TL burst fracture patients who are neurologically intact, treatment approaches vary dramatically across the globe.
So, the real controversy arises when dealing with injured patients who are neurologically intact. Treatment approaches range from conservative management with simple observation, medication, or bracing to various surgical interventions ranging from minimal invasive approaches to more invasive 360° reconstruction techniques. It appears, that treatment decisions are often influenced more by geography, surgeons training, and local school of thought rather than by evidence-based practice.
“In some parts of the world, patients with thoracolumbar burst fractures are almost always taken to surgery, while in others, they are rarely operated on,” says Cumhur Öner, Co-PI of the study. “What is striking is that there is no solid evidence base to justify such wide variation in practice.”

“In some parts of the world, patients with thoracolumbar burst fractures are almost always taken to surgery, while in others, they’re rarely operated on. What’s striking is that there’s no solid evidence base to justify such wide variation in practice.”
Cumhur Oner, University Medical Centers, Utrecht, the Netherlands
Addressing the evidence gap with diverse surgeon and patient cohorts
This ongoing debate in the medical community is also supported by conflicting evidence with a few studies reporting inconclusive results. To address this controversy and find an answer to a problem that has been debated for over decades, the AO Spine Knowledge Forum Trauma and Infection under the leadership of Marcel Dvorak and Cumhur Öner completed one of the largest prospective, multicenter observation cohort studies.
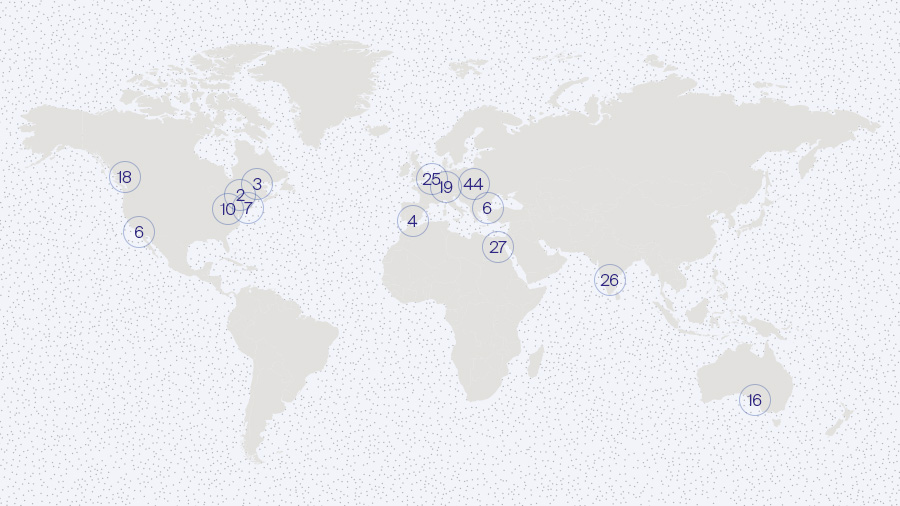
14 orthopedic and neurosurgeons from different regions enrolled 213 patients. These patients received either surgical or non-surgical treatments, depending on their local standard of care protocols. In the final analysis, 198 patients were included, with 122 receiving surgical treatment, while 76 patients were treated conservatively.
The primary objective was to assess whether surgery causes a more rapid improvement of disability as measured on the Oswestry Disability Index (ODI) within twelve months of the beginning of treatment. Patient satisfaction, time to return to work, and follow-up operations were also recorded. These outcomes were collected at discharge, 6 weeks, 3 months, 6 months, 1-year and 2 years.
The patient data was also used to perform a separate cost-utility analysis designed to compare the economic and social benefits of surgical and non-surgical treatment options at a global level.
This study was executed with support from the AO Innovation Translation Center (AO ITC). ClinicalTrials.gov Identifier: NCT02827214.
Participating investigators, sites, and patients enrolled:
Marcel F Dvorak, Vancouver, BC, Canada
Eugen Cezar Popescu, Iasi, Romania
Lorin M Benneker, Bern, Switzerland
S Rajasekaran, Coimbatore, India
Mohammad El-Sharkawi, Assiut, Egypt
Jin Wee Tee, Victoria, Australia
Jerome Paquet, Quebec, Canada
John C France, Morgantown, WVA, USA
Richard Allen, San Diego, California, USA
William F Lavelle, Syracuse, NY, USA
Miguel Hirschfeld, Marbella, Spain
Spyros Pneumaticos, Kifisia, Greece
Alexander R Vaccaro, Philadelphia, PA, USA
Cumhur F Oner, Utrecht, the Netherlands

“As with many acute injuries, the objective of treatment is to return patients to their pre-injury state of health and function as quickly as possible.
The results of the study provide the highest quality evidence for the treatment of thoracolumbar fractures in the literature to date and serve as a guide for treatment decisions to be made by surgeons and their patients with primary consideration given to patient preferences and a thorough understanding of the pros and cons of both treatment options."
Charlotte Dandurand, Vancouver General Hospital, BC, Canada
Key findings and clinical implications
The research results show no significant differences in terms of ODI improvement between surgical and non-surgical patients with thoracolumbar burst fractures without neurological injury—neither in the first year nor two years after their injury. Patients recovered well with both treatment options, with 85 percent reporting high satisfaction levels one to two years after sustaining the injury.
At the same time, surgical patients reported higher satisfaction earlier in their recovery. Differences between the two groups emerge as early as discharge and persist for up to one year, with non-surgical patients experiencing greater pain and disability. While a post hoc analysis of the data also suggests a trend towards more rapid improvement in surgical patients, this particular aspect was not statistically significant.
Overall, both treatment options led to patient recovery. It is therefore up to the attending surgeon to enable their patients to make more informed decisions by explaining the advantages and disadvantages of both treatment options based on the newly available evidence.
“Our results provide the highest quality evidence for the treatment of thoracolumbar fractures in the literature to date,” says Co-PI Charlotte Dandurand. “They serve as a guide for treatment decisions to be made by surgeons and their patients with primary consideration being given to patient preferences and a thorough understanding of the pros and cons of both treatment options. As with many acute injuries, the objective of treatment after all is to return patients to their pre-injury state of health and function as quickly as possible.”
Surgery emerges with long-term economic benefits
The separate cost-utility analysis considered the direct and indirect costs of treatment and was based on clinical data, patient diaries, peer-reviewed literature, and international healthcare cost guidelines and databases. The results show that, from a societal perspective, surgical management is more cost-effective within a two-year time frame than non-operative care. The main reason is a greater loss of productivity both among patients and caregivers within the nonsurgical group.
Within the first year after treatment, surgical treatment was not considered to be more cost-effective than non-surgical treatment. However, after two years, non-surgical patients had recorded more frequent visits to surgeons, general practitioners, physiotherapists, and other health professionals. They also had a higher reliance on pain killers and opioids, averaged more lost workdays, and caused caregivers to take significantly more time off work.
Read the full story:
PART A: Surgical versus Non-Surgical Treatment of Thoracolumbar Burst Fractures in Neurologically Intact Patients: A Prospective International Multicentre Cohort Study
PART B: Surgical versus nonsurgical treatment of thoracolumbar burst fractures in neurologically intact patients: a cost-utility analysis

“The study aims not only to guide individual clinical decisions but also to shape educational materials, inform health policy, and ensure that patients—regardless of where they live—receive care that is grounded in high-quality evidence and aligns with the patient’s values and yields the most acceptable overall benefit for them.
The AO Spine KF T&I will continue to collect evidence to support better decision making in treating thoracolumbar burst fractures without neurological deficits.”
Alexander Vaccaro, Rothman Orthopaedic Institute, Philadelphia, USA
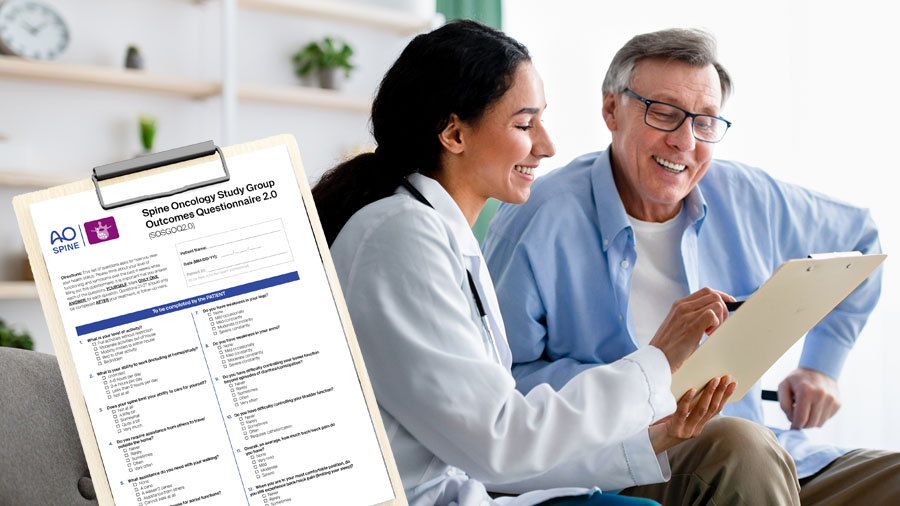
Lessons learned and the value of AO Spine PROST in spine trauma care
In acute trauma—unlike degenerative and other conditions—it is not possible to obtain a pre-injury baseline measurement, making it challenging to measure outcomes in terms of improvement or return to pre-injury status attributable to various treatments in this population.
Since the inception of the study, AO Spine PROST (Patient Reported Outcome Spine Trauma) was developed and validated as the first outcome measure specifically for trauma patients. Clinicians and researchers are encouraged to use this tool which will allow them, for the first time, to quantify the acute loss of functioning, and which treatment returns a patient more rapidly to its pre-injury functional status. The AO Spine PROST s available in 17 languages, including English, German, French.
Health economics is becoming increasingly important in clinical research. TL A3/A4 study shows the importance: while the primary outcome does not show a difference, the Health Economics analysis shows the social economic value of surgery.
This is the first study to provide a portrait of the existing international equipoise. Geographic variation exists in terms of treatment selection; Europe, Middle East and Northern Africa, and India preferred mainly surgical treatment, while North America and Australia have a tendency towards conservatively treated patients.
The global surgeon community can acknowledge the difference schools of thought existing currently worldwide creating worldwide equipoise even if there may not be local equipoise.
Shifting mindsets through global collaboration
This new research represents a significant contribution to a better understanding of why spine surgeons from different parts of the world manage similar injuries so differently. Although their outcomes are frequently excellent, significant practice variation exists among the 45 experts on the AO Spine Knowledge Forum Trauma and Infection. Oftentimes, their individual treatment preferences are based on personal beliefs, experience, training and local practice.
Throughout the study and subsequent discussions of its outcomes over the past several years, the members started to broaden their perspectives on different treatment options. They began to question long-held assumptions and became more open to accepting the benefits of other treatment opinions.
The reality is that there is no "one- size-fits-all"-guideline for these types of fractures. Instead, surgeons must strive to really identify the best treatment approach for each individual patient. “To that end, our study not only aims to guide individual clinical decisions,” says Alexander Vaccaro from the Rothman Orthopaedic Institute in Philadelphia, USA, a site investigator for the research. “It also aims to shape educational materials, inform health policy, and ensure that patients—regardless of where they live—receive care that is grounded in high-quality evidence and aligns with the patient’s values and yields the most acceptable overall benefit for them.”
Solidly scientific global data collection that can be tailored to various regional contexts as required is essential to enable healthcare practitioners to make nuanced recommendations. As a global organization with expert members around the world, AO Spine is ideally placed to provide this.
Ongoing analyses and future publications:
The Knowledge Forum Trauma and Infection continues to analyze data from this global multicenter study to address several important topics, including gender differences in patient outcomes, comparisons between A3 and A4 fractures, return to work, adverse events, the role of bracing.
Notably, access to radiographic imaging has provided a unique opportunity to examine how surgeons translate radiographic findings into clinical decisions.
The first focused publication—exploring the factors that influence treatment decisions based on baseline imaging—has already been published, offering valuable insight into why surgeons may recommend entirely different treatment approaches despite viewing the same radiographs. Analysis of follow-up imaging is currently underway, aiming to identify radiographic parameters that may help predict unfavorable patient outcomes.
The discussion is far from over. Stay connected with the Knowledge Forum Trauma and Infection as they continue to produce high-quality evidence to inform some of the field’s most pressing controversies on thoracolumbar (TL) burst fractures (AO Spine types A3 and A4) without neurological deficit with or without disruption to the posterior ligamentous complex.
References and further reading:
- Reinhold M, Knop C, Beisse R, Audigé L, Kandziora F, Pizanis A, et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J. 2010.
- Rajasekaran S, et al. Current Concepts in the Management of Thoracolumbar Burst Fractures Without Neurological Deficit. J Orthop Surg (Hong Kong). 2010.
- AO Spine Knowledge Forum Trauma. [Study protocol for TL A3/A4 Burst Fracture Comparison Study], AO Foundation, ongoing research.
- Special Issue: What Motivates Treatment Decisions in Neurologically Intact Thoracolumbar Burst Fractures? GSJ Vol. 14 (1S) February 2024.
- Dvorak MF, Öner CF, Dandurand C, et al. Surgical versus Non-Surgical Treatment of Thoracolumbar Burst Fractures in Neurologically Intact Patients: A Prospective International Multicentre Cohort Study. Global Spine Journal. 2025;0(0).
- Dandurand, Charlotte et al. Surgical versus nonsurgical treatment of thoracolumbar burst fractures in neurologically intact patients: a cost-utility analysis.
The Spine Journal, Volume 25 (7) 1494-1507.
You might also be interested in...
Global Spine Journal Focus Issue
What Motivates Treatment Decisions in Neurologically Intact Thoracolumbar Burst Fractures? A popular GSJ Focus issue by Knowledge Forum Trauma and Infection.
AO Spine outcome instruments
Disease-specific outcome tools developed and validated by AO Spine. Download and start using the AO PROST and AO CROST for spine trauma patients and clinicians treating them.
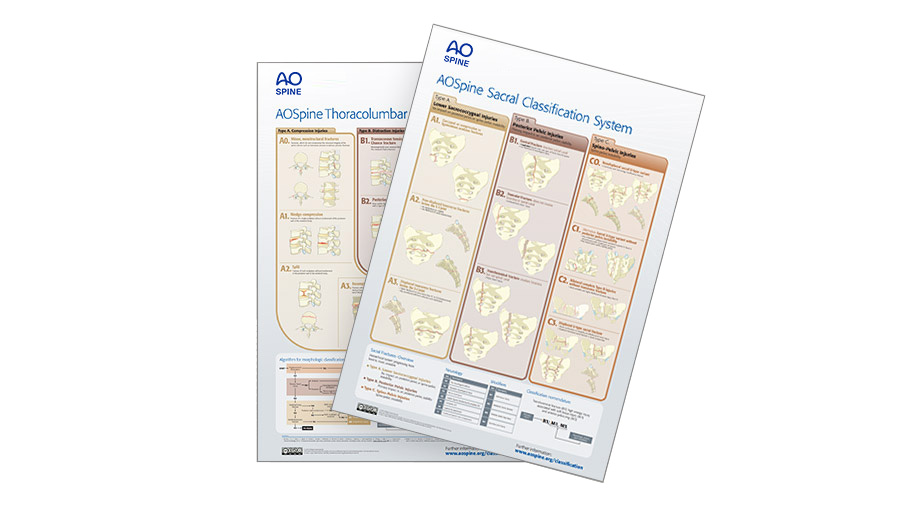
AO Spine Injury Classification Systems
Download the toolkits and watch the videos for new and trusted classification systems developed and validated by the AO Spine Knowledge Forum Trauma and Infection.
AO Spine Knowledge Forum Trauma and Infection
Dedicated to improving patient care, advancing knowledge, and developing reliable classification systems plus diagnostic and therapeutic algorithms.