Supporting high-quality clinical and translational research in the spine field
AO Spine congratulates the winners of the first-ever AO Spine Knowledge Forum Associate Member Research Award

The five winners have been named of the 2022 AO Spine Knowledge Forum (KF) Associate Member Research Award. They are Marco Palanca (KF Tumor), Çağlar Yılgör (KF Deformity), Allan Martin (KF Spinal Cord Injury), Mohamed Aly (KF Trauma) and Carla Cunha (KF Degenerative).
The AO Spine KF Associate Member Research Award has been devised by the AO Spine Research Commission and is given out for the first time this year. It is designed to financially support and to engage AO Spine KF Associate members who have a desire to perform research projects complimentary to the priorities defined by the AO Spine Knowledge Forums.
The AO Spine Knowledge Forums are a set of five international study groups dedicated to the specialty fields of spine tumor, deformity, trauma, spinal cord injury, and degenerative disease. Consisting of scientists and clinicians from all over the world, their main goal is to create new knowledge in spinal health, to fill in blanks in the existing research, and ultimately to make a positive impact on patient care.
The award is open only to KF Associate members who propose to conduct clinical or translational investigations with direct relevance to their respective KF pathology. Eventually, they will be presenting their research outcomes at the Global Spine Congress.
Here, the five winners introduce their research projects:
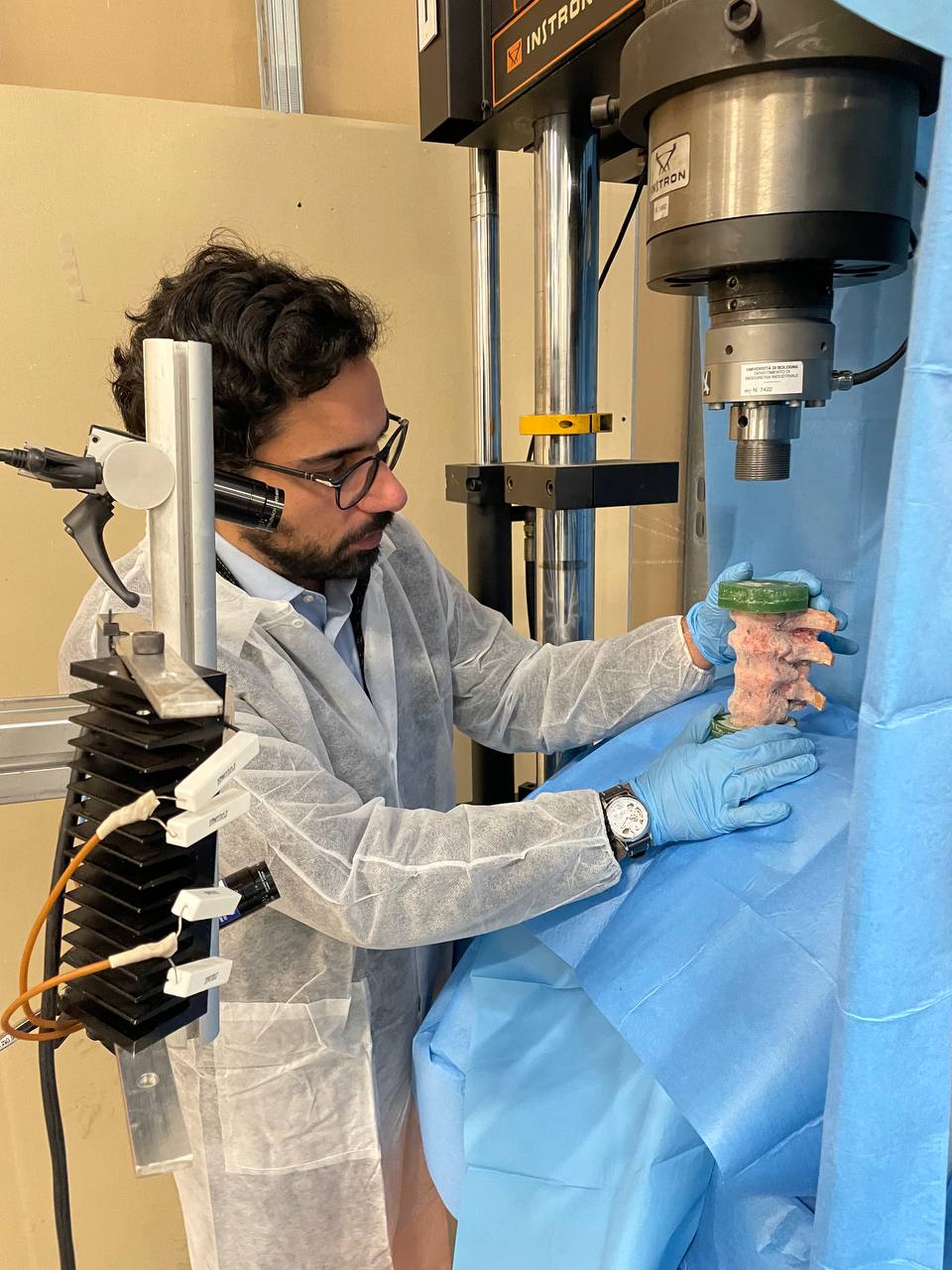
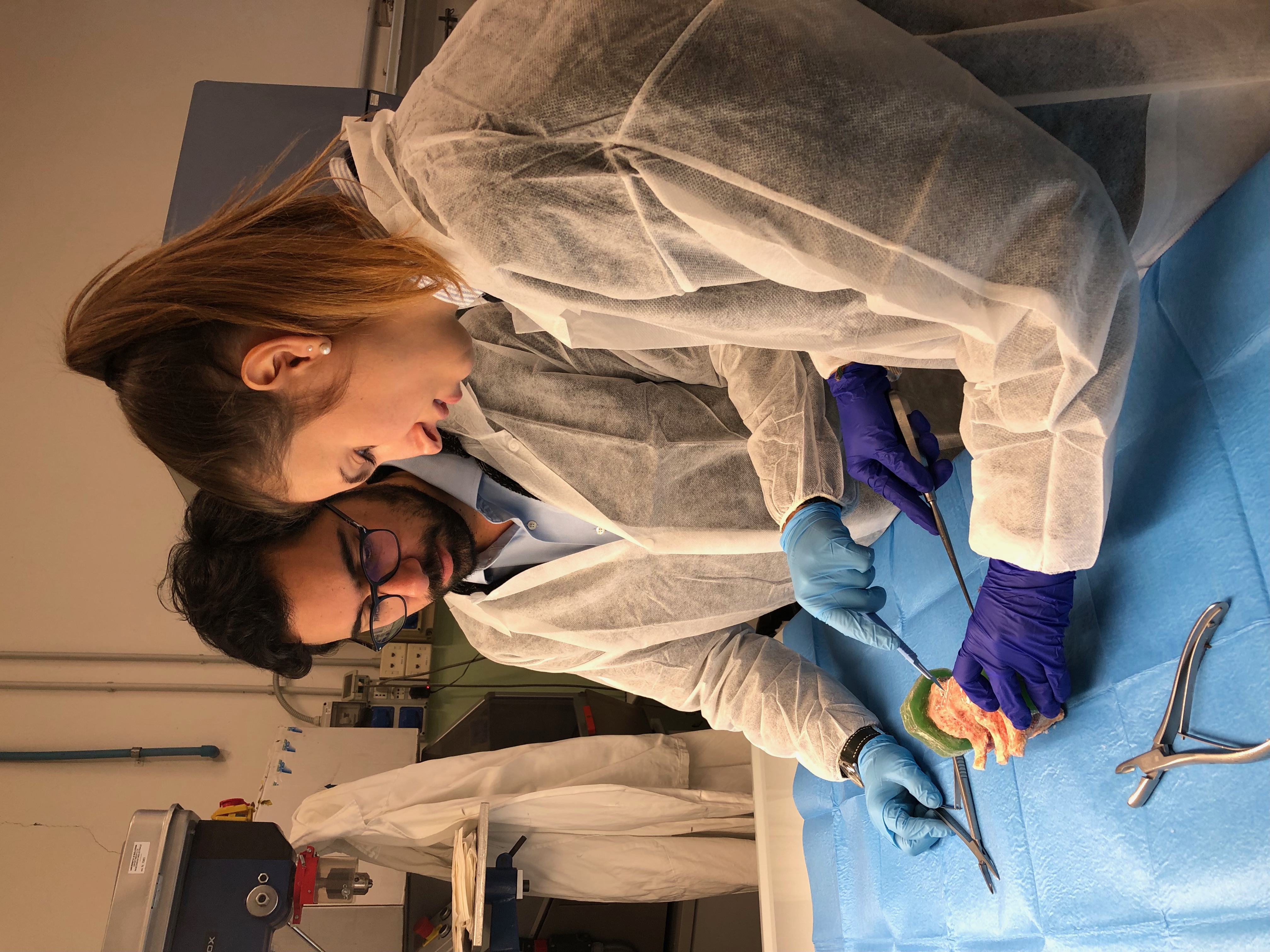
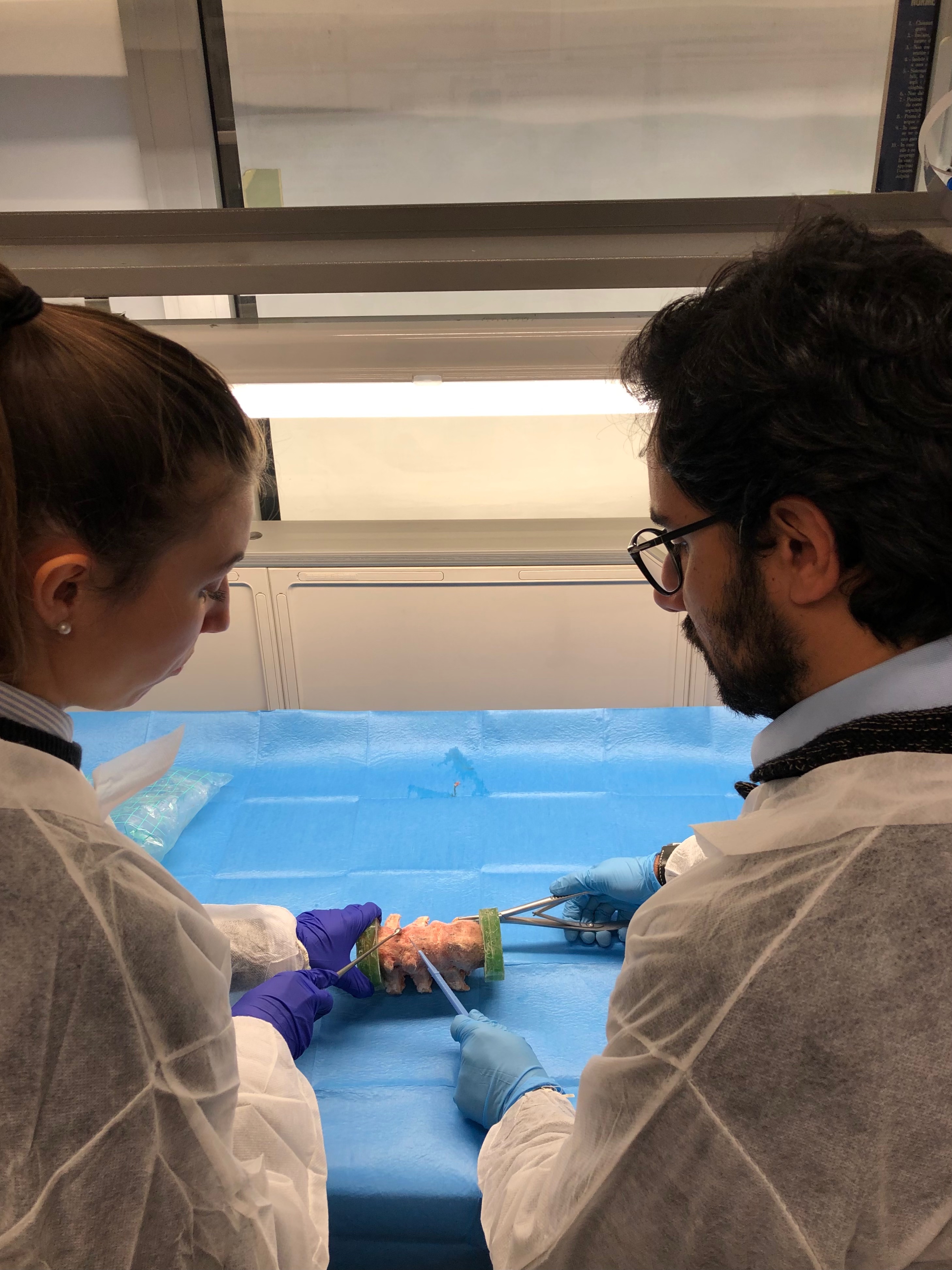
KF Tumor: Effect of the intervertebral disc conditions on the risk of vertebral fracture in metastatic patients
Marco Palanca, PhD; Research Fellow, Department of Industrial Engineering, University of Bologna, Italy
Cancer patients with metastatic vertebrae are at an increased risk of fracture. When evaluating this risk, we frequently look only at the bone—the actual vertebrae—without looking at the role played by the intervertebral discs (IVD). In this research project, we aim to evaluate what the IVDs contribute to the reduction, or increase, of the risk of fracture.
Right now, assessing the risk of fracture in patients with metastatic vertebrae is quite difficult. It relies to a large extent on the clinicians’ expertise. I hope that we can provide fundamental knowledge in order to improve the treatment of debilitated oncological patients. Deciding on the best prophylactic treatment for a patient is an unsolved challenge. I zoomed out from just the vertebrae to the spine and I hypothesize that the IVDs might help us provide better predictions.
I am a mechanical engineer by training, and working on bones or with living tissues is far removed from the typical tasks of an engineer. On the other hand, it is really interesting to see how engineering know-how can be applied to approach medical problems. The AO Spine Knowledge Forum Tumor is the best place to share this kind of knowledge. As an engineer, I am something of an outsider in the group, as it is mostly made up of clinicians. But it is a great place to receive fresh input, to exchange new knowledge and challenges and to be inspired. I am really happy to be a part of this group.
If I was asked to give tips to younger colleagues, I would advise them to stop believing that there is only one way to solve a problem. Use different approaches, try out different strategies and find inspirations in other fields. You may sometimes head in the wrong direction, but in the long term, it works.
KF Deformity: Does vertebral body tethering cause disc and facet joint degeneration? A mid-term MRI study with minimum five years follow-up
Çağlar Yılgör, Acibadem Mehmet Ali Aydinlar University School of Medicine, Istanbul, Turkey
Vertebral body tethering (VBT) is a non-fusion surgical technique to treat adolescent idiopathic scoliosis. Non-fusion implies continued motion, so appropriate treatment strategies should preserve the discs and facet joints in order to be successful in the long term. Our research project aims to assess viability of the discs and facet joints of the intermediate and adjacent thoracic and lumbar levels for signs of degeneration, and to evaluate for signs of spontaneous fusion.
VBT is claimed to be a safe and efficient procedure that may, in a selected group of patients, provide substantial advantages over both operative delaying tactics and definitive spinal fusion. Plus, early clinical results look promising. As a result, VBT is becoming increasingly popular with demand from families on the rise. However, VBT is clearly not exempted from ‘classical’ mechanical complications: in a recent report, we have demonstrated screw migration and loosening in VBT applications as well as technique-specific complications such as tether breakage and overcorrection. Although disc health after various non-fusion techniques has been assessed in animal models, and tethering has been claimed to prevent degeneration due to its less rigid nature compared to other growth-friendly techniques, these results cannot directly be extrapolated to humans. Being able to determine in a clinical setting the medium- and long-term viability of discs and facets joints will therefore be a key aspect in the decision-making process.
I have had a passion for research ever since my junior residency years in orthopedics. In the following years, becoming a spine surgeon was a new challenge with three-dimensional thinking, mechanics, physics, and tissue engineering incorporated into surgical art. To this day, I keep the passion alive by actively participating in several societies and their committees, and by being involved in various international study groups.
AO Spine is the perfect melting pot for multicenter clinical and basic science research. I have been an AO member since 2015 and I attended my first Global Spine Congress in 2016. I have served as an Associate Member in the Knowledge Forum Deformity since 2019 and took part in several AO endorsed studies such as PEEDS, SDIM and FLEXIS. I was a part of the project team for the AO Spine Adult Spinal Deformity Patient Profile and, currently, I am participating in the Next Big Project.
KF Spinal Cord Injury (SCI): The Degenerative Cervical Myelopathy—Subjective and Objective Score (DCM-SOS), a novel outcome measure
Allan Martin, MD, PhD; Assistant Professor, Complex Spine and Associate Program Director, Neurosurgery, University of California, Davis, USA
In this project, we seek to develop and validate a novel method to categorize the severity of degenerative cervical myelopathy (DCM) in patients. Our proposed DCM Subjective and Objective Score (DCM-SOS) will combine subjective questions with a brief objective scored neurological examination in a short assessment of up to ten minutes.
DCM is a common condition in which degenerative arthritic changes occur, causing compression and impairment of the spinal cord. Patients with moderate to severe neurological impairment can be treated surgically, as can patients with mild impairment that subsequently deteriorates. Currently however, categorization of DCM severity is based solely on the modified Japanese Orthopedic Association (mJOA) score. It is a simplistic and subjective tool that assesses four domains on ordinal scales using terms such as ‘mild’ or ‘severe’. We hope the DCM-SOS, which will be designed as an extension to the mJOA score, will allow us to assess DCM severity with more accuracy and detail.
I am passionate about making a difference in patient outcomes, and in spine surgery, DCM presents perhaps the greatest opportunity to do so. It is among the most common and treatable neurological disorders, but is grossly under-studied in comparison with traumatic spinal cord injury, stroke, multiple sclerosis, and central nervous system tumors. Furthermore, surgical treatment of DCM is safe and highly effective, not only to prevent further neurological deterioration, but to improve neurological status. However, DCM is infrequently covered in medical curricula and diagnosis is often delayed, even by some specialists. Furthermore, mild DCM is poorly understood, with a lack of diagnostic criteria and tools designed to measure mild impairment.
My involvement in the AO Spine Knowledge Forum SCI for the past two years has been a tremendously positive experience. It has linked me with global experts in SCI to produce meaningful research and allowed my own career to blossom. I have been involved in numerous systematic reviews, clinical practice guidelines, education projects, and incubators for the AO Spine RECODE-DCM project. I am very grateful to have received this award, and I believe it will allow the DCM-SOS project to succeed. I expect the KF will continue to produce impactful research over the coming years and I look forward to ongoing participation in it.
KF Trauma: CT criteria for diagnosis of thoracolumbar posterior ligamentous complex injury: a multicenter validation study
Mohamed Aly, MSc MD, PhD, MRCS; Associate Professor of Neurosurgery, Mansoura University, Egypt; Consultant Neurosurgery and Program Director Neurosurgery Residency, Prince Mohamed Ben Abdelaziz Hospital, Riyadh, Saudi Arabia
The main objective of my research project is to standardize computed tomography (CT) analysis in order to provide accurate and reliable criteria to diagnose posterior ligamentous complex (PLC) injury of the thoracolumbar spine without the need of magnetic resonance imaging (MRI).
CT assessments of PLC injuries are often said to be the least reliable part of current classification schemes. CT scans cannot not directly visualize PLC structures. PLC injury therefore is typically inferred based on indirect CT signs. However, in many cases the exact diagnostic value of these indirect signs still has to be validated by MRI.
We have previously shown that CT analysis can provide values that are sufficiently accurate to reliably rule in or rule out PLC damage. As a result, we have proposed criteria based on the number of positive CT findings: if there are two or more positive CT findings based on a high positive predictive value (PPV, 91%), the PLC should be considered injured. If there is a single positive CT finding (PPV 34%), it should be considered indeterminate, an if there are no positive CT findings (PPV 9%), it should be considered intact. The current study aims to externally validate our previous findings in multiple centers with different populations by independent reviewers.
I hope this study will provide clear guidelines for spine surgeons on when to obtain an MRI for PLC assessment in neurologically intact patients. As a result, fewer cases of PLC injuries would be missed. At the same time, unnecessary MRIs for thoracolumbar fractures would be reduced, along with the associated cost, effort, and, more importantly, treatment delay for such patients. I also fervently believe that this work could be a step toward developing a universal algorithm for thoracolumbar fractures.
I consider it a privilege to be a part of the AO Spine KF Trauma. This study endeavor was significantly strengthened by interactions with this group of expert spinal researchers. In addition, receiving the grant to assist my research through the KF has been a tremendous pleasure and privilege.
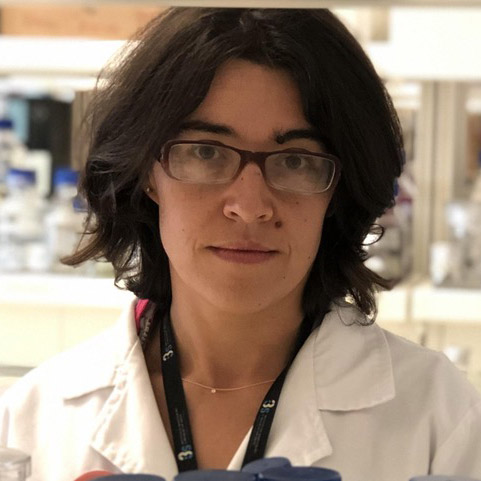
KF Degenerative: Pinpointing the specific macrophage phenotypes involved in intervertebral disc hernia regression
The goal of my research project is to identify specific macrophage phenotypes with a high potential to be used in a therapy to reverse intervertebral disc herniation in the lumbar region. Lumbar disc herniation (LDH) occurs when the outer, fibrous layer of an intervertebral disc tears, often as a result of trauma or degeneration. The soft substance in the center of the disc subsequently protrudes outward, often causing pain in the lower back or legs and severely affecting mobility and quality of life. It is an unmet clinical need, for which no physiological therapy is presently delivering consistent improvements.
Although we still have a long way to go regarding product development and clinical validation, what we propose in the long run is a therapy that will offer an alternative to invasive and costly surgery to remove the herniated tissue. Macrophages, a type of white blood cell, play a key role in hernia regression and we’re hoping to use them to provide a minimally invasive solution for patients under conservative treatment with highly uncertain prognoses. The ultimate goal is to improve patients’ quality of life.
The AO Spine KF Degenerative brings together spine experts from around the world and allows us to collectively discuss topics that are central to patient care. Since I am a researcher and a biologist by formation, the support from this network, which is composed mainly of clinicians, is extremely important to me: it better attunes my research towards clinical needs, and it will certainly be key in translating this line of research into the clinical world.
You could also be interested in:
AO Spine Knowledge Forums
The AO Spine Knowledge Forums are the engines of AO Spine clinical research, leading the way in global spine research
AO Spine Guest Blog
Hot topics around spine from the global spine community. Read the latest guest authored articles from the spine network around the world.
Clinical library and tools
A collection of open assets and membership benefits to develop your competencies and improve your patient care.