The role of telemedicine in spine surgery—AO Spine Task Force takes the lead
After the World Health Organization declared COVID-19 a pandemic in March 2020, health care professionals around the world suddenly found themselves communicating with patients through telemedicine, often without clear guidelines. AO Spine has taken a lead role in understanding how telemedicine has affected spine care, training, and research—publishing a series of peer-reviewed articles based on a May 2020 survey of spine surgeons from around the world. (*)
In February 2021, AO Spine research assembled a Telemedicine Expert Panel to reach consensus on Appropriate Telemedicine Utilization in Spine Surgery, resulting in a February 2022 publication in Spine. The expert panel consisted of 27 spine surgeons (22 orthopaedic, 5 neurosurgical), most from the United States but some from Asia, Europe, Latin America, and the Middle East. According to the 2020 AO Spine survey, utilization of telemedicine during the pandemic increased the most in North America, from <7% to >60% of all visits, compared to <10% to >39% for the larger survey group.
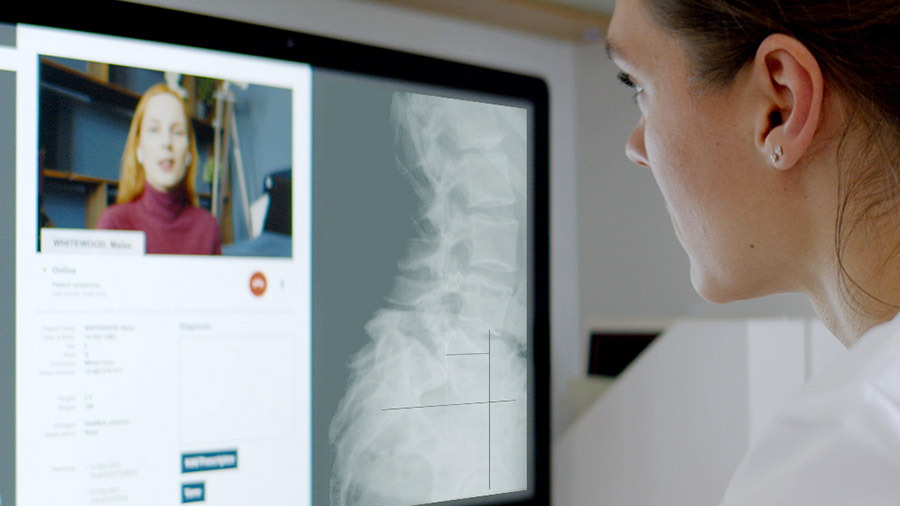
Contributing author Andrew J. Schoenfeld explains “Spine consultations with telemedicine can serve as a means to facilitate evaluation for patients who would otherwise have to travel great distances and can reduce barriers to access. This includes initial consultation as well as follow-up to review indications for surgery, discuss surgical management, review imaging, and look at postoperative wounds.”
Limitations of telemedicine and what is acceptable
The expert panel focused on five themes: (1) Impact of patient location, (2) Impact of patient diagnosis on assessment of new patients, (3) Utility and limitations of the telemedicine physical examination, (4) Need for in-person visits prior to surgery, and (5) Acceptable visit types using telemedicine. For each topic, the goal was to achieve a consensus (>75% agreement) or a strong agreement (>66 to 74% agreement), which was not always possible.
For topic (1), the consensus was that a patient’s geographic location does not significantly affect the surgeon’s ability to deliver safe and appropriate care through video-based telemedicine (VT). There was more uncertainty about using audio-based telemedicine (AT), which is consistent with previous research and recommendations.
For topic (2), the panel focused on 5 categories of diagnosis: lumbar stenosis, lumbar radiculopathy, cervical myelopathy, cervical radiculopathy, and spinal deformity. Co-author Sravisht Iyer explains, “For some of the most common problems we see in spine—things like lumbar stenosis, lumbar disc herniation (lumbar radiculopathy)—a lot of the surgeons felt that it was very possible to appropriately see, evaluate, and indicate patients for surgery using (video-based) telemedicine.”
For topic (3), consensus was reached for only 2 factors related to the remote physical exam: that it is possible to evaluate for gait abnormalities through VT, and that special tests for myelopathy are not possible through VT. There was no consensus regarding the measurement of upper and lower extremity strength, evaluation of neurological deficits, or special tests for other diagnoses. Previous studies also identified the physical exam as a weakness of telemedicine, which highlights the importance of continued research to optimize remote physical examination maneuvers.
When the initial patient consultation is through VT, the group consensus for topic (4) was that in-person evaluation prior to surgery is essential for cervical myelopathy and spinal deformity, and best practice for cervical radiculopathy. There was strong agreement that in-person evaluation prior to surgery is best practice for lumbar stenosis and lumbar radiculopathy. An in-person evaluation might involve a preoperative visit closer to the date of surgery, or evaluation in the holding area before surgery.
For topic (5), there was consensus that VT could be appropriate for early (2-6 week), mid-term (3-6 month), and longer-term (>6 month) postoperative follow-up, as well as imaging review, and follow-up after an intervention such as physical therapy or epidural steroid injection. For postoperative wound issues, the consensus was that audio visits are not suitable, and strong agreement (but no consensus) that video visits could be suitable. Previous studies have supported the utility of VT for communicative tasks such as taking a patient history and formulating and communicating a treatment plan.
The way forward—What happens after COVID?
In the United States, the rapid adoption of telemedicine was facilitated by waivers which allowed remote care to be practiced across state lines and appropriately compensated. As these mandates expire and COVID restrictions are lifted, physicians and patients are again facing geographical constraints.
Corresponding author Melvin C. Makhni adds, “In addition to clinical barriers, there are significant technical, logistical, political, medico-legal, and financial challenges that limit the widespread usage of telemedicine. With continued investment in systems and technology, and a comprehensive overhaul of regional legislation, telemedicine may further deliver on its promise to revolutionize healthcare delivery.”
As COVID restrictions are lifted, many patients are still choosing telemedicine as a convenient way to receive care. Schoenfeld adds, “I think telemedicine is here to stay and is a vital and worthwhile piece of technology.”
Iyer believes that guidance on the use of telemedicine “needs to come from more than just spine. For example, the AMA (American Medical Association) could take a strong position on saying that telemedicine is safe and appropriate.” The research group also noted the need to establish a uniform standard to obtain medical licenses for physicians who practice telemedicine in multiple jurisdictions.
Iyer adds, “I think the next step is using telemedicine not just as another way to provide the same type of care, but as a way to enhance the care that we’re providing.” Perhaps telemedicine could be used in conjunction with wearable devices that give the surgeon a sense of “how well a patient is moving, how many steps per day.”
Furthermore, physicians and institutions need to be more deliberate about incorporating telemedicine into clinical education and research. The 2020 AO Spine survey found that only 21.6% of respondents had trainees present during telemedicine visits. Telemedicine could also facilitate patient involvement in clinical trials, which suffered during the pandemic.
Co-author Dino Samartzis concludes “Our project has highlighted some very important issues and best practices to help guide spine surgeons and their use of telemedicine. Moving forward, the spine community needs to coalesce to impact policy, not just in the USA but potentially worldwide. We thank AO Spine for their support and are confident that working together, we can continue to lay out future blueprints that can impact patient care.”

Andrew J. Schoenfeld

Melvin C. Makhni

Sravisht Iyer

Dino Samartzis
(*) References and additional reading:
Riew GJ, Lovecchio F, Samartzis D, et al. Telemedicine in Spine Surgery: Global Perspectives and Practices. Global Spine Journal. June 2021. doi:10.1177/21925682211022311
Iyer, Sravish, Bovonratwet, Patawut; Samartzis, Dino, et al. Appropriate Telemedicine Utilization in Spine Surgery, SPINE: April 15, 2022 - Volume 47 - Issue 8 - p 583-590 doi: 10.1097/BRS.0000000000004339
Riew, G.J., Lovecchio, F., Samartzis, D. et al. Spine surgeon perceptions of the challenges and benefits of telemedicine: an international study. Eur Spine J 30, 2124–2132 (2021). https://doi.org/10.1007/s00586-020-06707-x
Lovecchio, F., Riew, G.J., Samartzis, D. et al. Provider confidence in the telemedicine spine evaluation: results from a global study. Eur Spine J 30, 2109–2123 (2021). https://doi.org/10.1007/s00586-020-06653-8

