Beyond the portal wars: forging a new consensus in endoscopic spine surgery

Endoscopic spine surgery is progressing rapidly and expanding the options available for degenerative spinal pathology. As the clinical adoption curve steepens, however, the field has also become increasingly polarized, particularly around uniportal full-endoscopic techniques versus biportal endoscopic approaches (UBE/BESS). Polarization can drift from constructive comparison into entrenched “either–or” positioning. That shift does not serve patients or the broader field. With this article, I hope to launch a discussion and move beyond the debate towards consensus.
-
Read the quick summary:
- Prof Jin-Sung Kim discusses the debate between uniportal and biportal endoscopic spine surgery techniques and urges focus on consensus rather than rivalry.
- Both techniques are valuable tools; the field should adopt a pathology-driven, consensus-based approach to technique selection.
- Next steps include developing shared terminology, evidence-based indications, standard outcome measures and joint training frameworks worldwide.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Moving beyond the debate
Both approaches have demonstrated clinical effectiveness, and the discussion should reflect that reality. When technique identity starts to replace careful thinking about indications, outcomes, and patient-specific anatomy, the debate becomes less scientific. This can lead to fragmented research efforts, inconsistent training pathways, and confusion among early-career surgeons trying to choose a direction in a crowded educational landscape.
Endoscopic spine surgery remains young compared with open and microscopic surgery and the specialty should prioritize collaboration over competition. At this stage of development, cross-regional collaboration and shared learning, multicenter evidence generation, and shared standards will accelerate progress far more than rivalry.
Uniportal and biportal endoscopy are not competing philosophies. They are complementary tools, and our job is to use them well and appropriately.
Pathology-driven selection
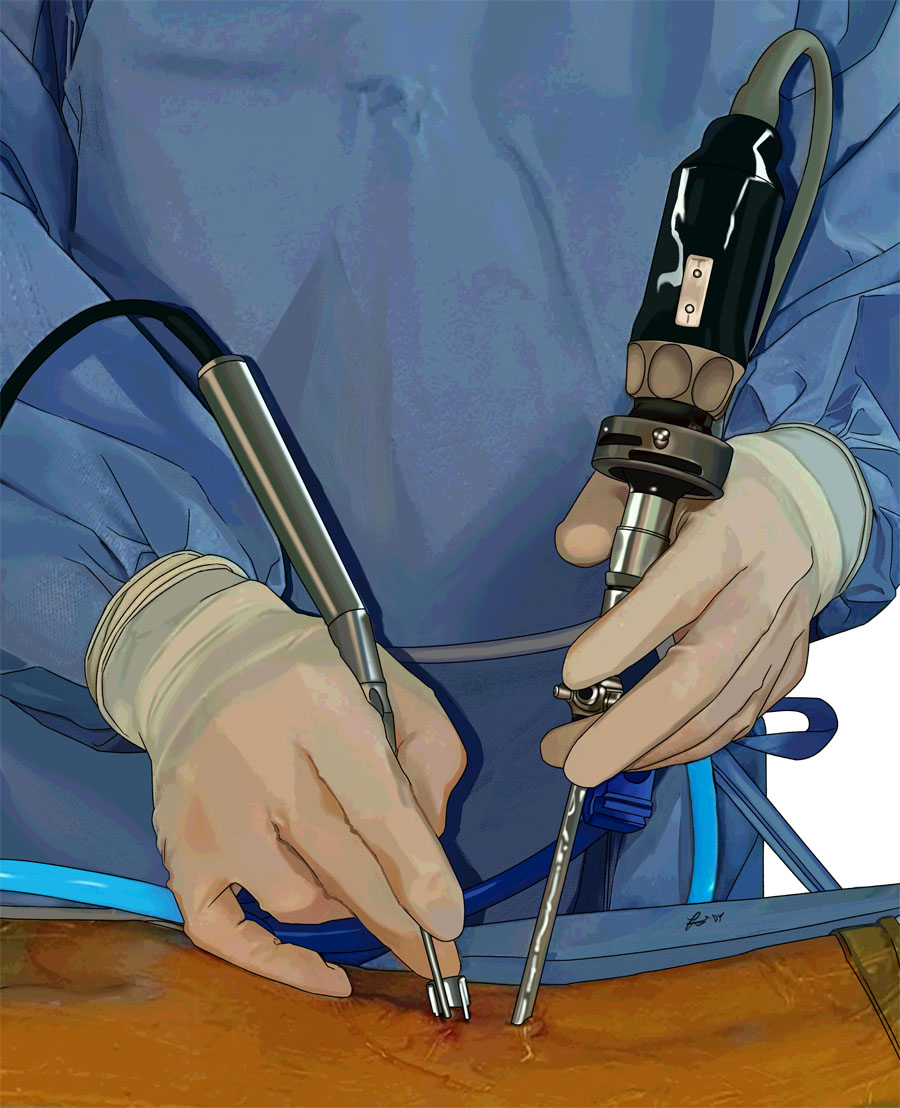
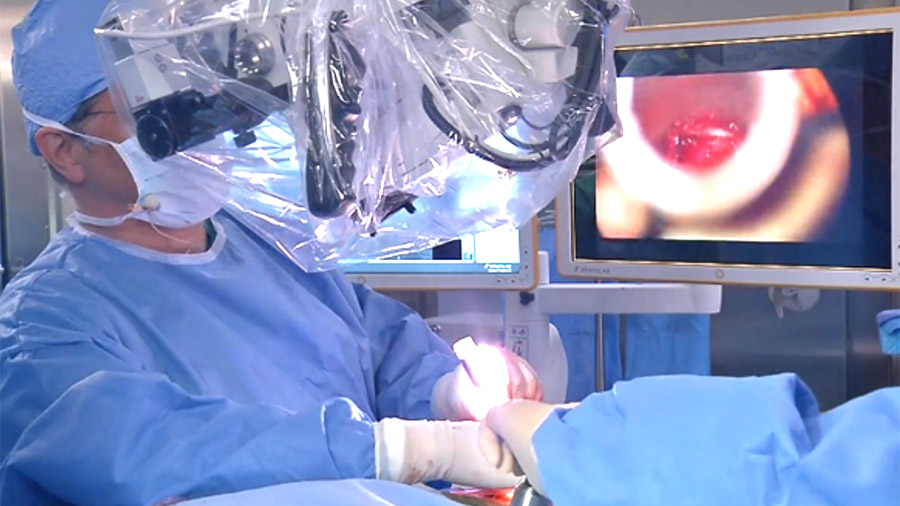
Uniportal full-endoscopic surgery provides strong magnification through a single working channel and can be advantageous in confined anatomical spaces. Many surgeons find endoscope-based visualization intuitive, particularly those with experience in arthroscopic disciplines. At the same time, the restricted corridor can limit instrument triangulation and increase the technical demands of broader or more complex decompressions.
Biportal endoscopic surgery uses separate viewing and working portals, which can improve instrument maneuverability and allow use of conventional spinal instruments. For surgeons transitioning from microscopic tubular surgery, this can feel more familiar and may reduce barriers during the learning curve. However, maintaining clear visualization, and managing irrigation can be technically challenging, especially in less experienced hands, so the apparent flexibility of instrumentation does not automatically make the procedure easier.
The key question is not “which is better,” but “which approach is most appropriate for this pathology in this patient, in this surgeon’s hands?” A pathology-driven approach requires moving beyond preference and building a neutral framework for decision-making. Relevant considerations include:
- Type and location of pathology (central stenosis, foraminal stenosis, recurrent disc herniation, extraforaminal pathology)
- Anatomical constraints and prior surgery
- Surgeon experience and technical proficiency in each approach
- Available equipment, team familiarity, and institutional support
- Patient-specific factors such as comorbidities, expectations, and risk tolerance
Consensus-driven technique selection does not mean techniques are interchangeable. It means we develop a shared understanding of where each method performs best, where it struggles, and when it should not be used.
A tool within minimally invasive surgery (MIS)
Minimally invasive spine surgery requires adaptable skills rather than dependence on a single technique. In practice, this means moving across microscopic tubular surgery, endoscopic techniques, MIS TLIF, LLIF, and deformity correction when indicated. The modern MIS surgeon cannot be defined by one method. The surgeon should be defined by decision-making quality, technical versatility, and measurable outcomes.
Endoscopic spine surgery is a powerful tool within MIS, but it cannot be the solution for every patient or every pathology. There is a risk with any emerging technology cycle and enthusiasm could outpace appropriate indication boundaries. When that happens, surgeons may expand a favored technique rather than selecting the best approach for the pathology.
A mature MIS practice places endoscopy in context. It is a valuable option, not a universal answer. Long-term credibility for endoscopic spine surgery depends on disciplined indication selection and transparent reporting, not on promotional narratives.
The question surgeons ask most
At international meetings, a recurring question is: “When should one choose full-endoscopic surgery, and when is biportal preferable?” This is often what surgeons early in their endoscopic journey want answered most. It is also one of the most difficult questions to answer cleanly because real-world pathology does not fit neatly into technique categories, and because both techniques have overlap.
Still, the question is important, because the absence of guidance creates a vacuum that is easily filled with anecdote, local training lineage, or online “technique branding”. Experience suggests substantial overlap in indications, with scenario-specific advantages influenced by pathology, anatomy, and surgeon experience, so guidance should be balanced and practical. The goal is to clarify decision logic, not to declare winners.
Here, a consensus mindset will help, and we should be teaching surgeons how to evaluate pathology and apply the right method. Over time, this approach will raise the overall standard of care and reduce the temptation to force a technique into every clinical scenario.
Common language first
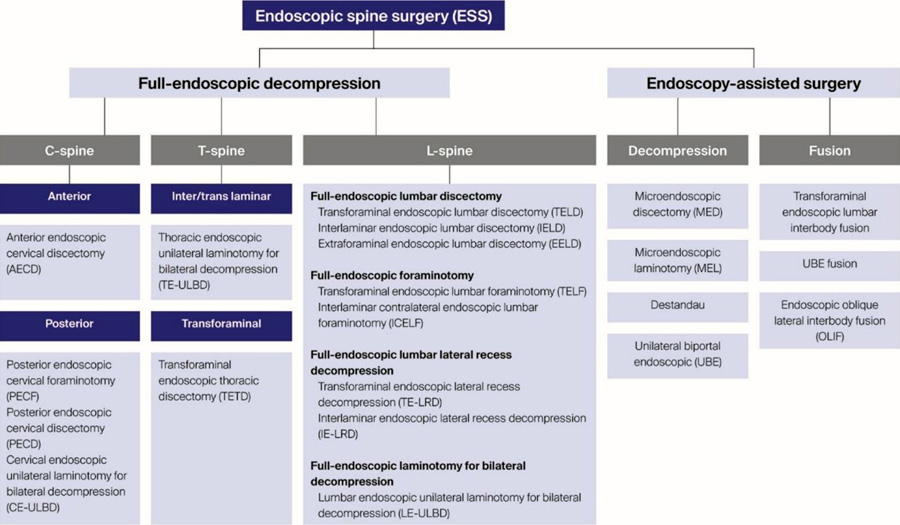
Meaningful comparison depends on consistent terminology. The Consensus Paper on Nomenclature for Working-Channel Endoscopic Spinal Procedures was an important first step toward a shared language. Standardized terms reduce confusion and make collaboration and data interpretation more reliable across borders.
Without unified language, the evidence base becomes distorted. Subtle differences in technique, indication definitions, and outcome reporting make it difficult to compare studies or pool data into high-quality analyses. Rivalry only amplifies this problem, because communities may adopt separate terms and classifications that reinforce division rather than shared learning.
Beyond nomenclature, consensus is needed around:
- Clear definitions of indications and contraindications based on evidence
- Agreed-upon outcome measures and follow-up intervals
- Reporting standards for complications, revisions, and reoperations
- Training milestones and competency thresholds
When surgeons agree on shared frameworks, research quality improves, clinical translation becomes more reliable, and patients benefit from more predictable decision-making.
Training and dissemination
Training remains a bottleneck, and one-technique pathways can unintentionally reinforce one-sided perspectives. This helps explain why opinions can harden after different learning-curve experiences. Many surgeons are trained exclusively in either uniportal or biportal techniques depending on regional trends, mentor expertise, or course availability. This focused training can produce technical excellence, but it can also introduce bias and reduce adaptability.
Surgeons who master only one technique may unconsciously expand its indications beyond optimal boundaries or dismiss alternative approaches without adequate evaluation. Structured exposure to both approaches—supported by frameworks such as the AO Spine MISS Curriculum—can promote accountability, safety, and more objective decision-making.
Endoscopic training should emphasize foundational principles that apply across approaches, while also developing technique-specific proficiency. Effective educational models should include stepwise skill acquisition, objective assessment of technical competency, and mentorship with ongoing peer review. Short workshops and industry-driven courses can be helpful, but they are rarely sufficient on their own for safe, reproducible adoption.
A unified vision
Progress will depend less on technique “teams” and more on shared principles: pathology-driven indications, standardized nomenclature, transparent outcome reporting, and training that reflects the true spectrum of MIS practice. An international consensus on indications and technique selection—built by experts with meaningful experience in both uniportal and biportal approaches—could standardize training, optimize outcomes, and support safer global dissemination.
Ultimately, the question is no longer whether uniportal or biportal endoscopy is better. The more meaningful question is how spine surgeons can best use all available techniques to improve outcomes for the patients they serve. A unified, evidence-based future for endoscopic spine surgery depends on that shift in mindset, from rivalry to responsibility, from branding to better care.
About the author:
You might also be interested in...
MISS Spectrum Series online course
A comprehensive learning experience for practicing surgeons.
AO Surgery Reference resource
Manage spinal trauma, deformities, tumors, and degeneration.
Family first—the best career decision
An interview with Jin-Sung (Luke) Kim on his career.