Controversies in treating complex spinal infections: case studies and expert insights
BY DR JONATHAN DALTON, DR GREGORY SCHROEDER, AND DR CHARLOTTE DANDURAND

Spinal infections are a worldwide problem that, until recently, have failed to receive the same amount of academic interest as other non-elective spinal conditions such as spinal trauma and spinal neoplasms. Because of this, there is substantial treatment variability not only across the globe, but also even within institutions.
The following cases highlight some of the challenges facing surgeons. Gregory Schroeder, MD who is an Associate Professor of Orthopaedic Surgery at Thomas Jefferson University in Philadelphia and the Chairman of the AO Spine Trauma and Infection knowledge forum and Charlotte Dandurand MD, MSc, FRCSC who is a neurosurgeon from the Combined Neurosurgical and Orthopaedic Spine Program at Vancouver General Hospital will review three challenging cases and explain their treatment strategies and rationale for management.
-
Read the quick summary:
- Gregory Schroeder and Charlotte Dandurand discuss complex spinal infections, comparing surgical vs. non-surgical management approaches.
- Spinal infection treatment varies widely due to limited research. Early surgery may be beneficial, but nonoperative management is often attempted first.
- A global classification system and evidence-based guidelines are needed to standardize spinal infection treatment and improve patient outcomes.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Case 1: A 56-year-old male with discitis osteomyelitis
Patient presentation
The first case involves a 56-year-old male with minimal past medical history, consisting solely of mild hypertension. He initially presented to the Emergency Department (ED) after one week of low back pain, that progressively worsened and woke him up from sleep the night prior to his ED presentation. He endorsed some radiation of the pain down the posterior aspect of his right lower extremity, but denied any motor weakness or decreased sensation. He denied any issues with ambulation and had no bowel/bladder symptoms. On the evening prior to his presentation to the ED, he had subjective fevers/chills, but denies any shortness of breath, nausea/vomiting, or any other constitutional symptoms.
Diagnostic workup
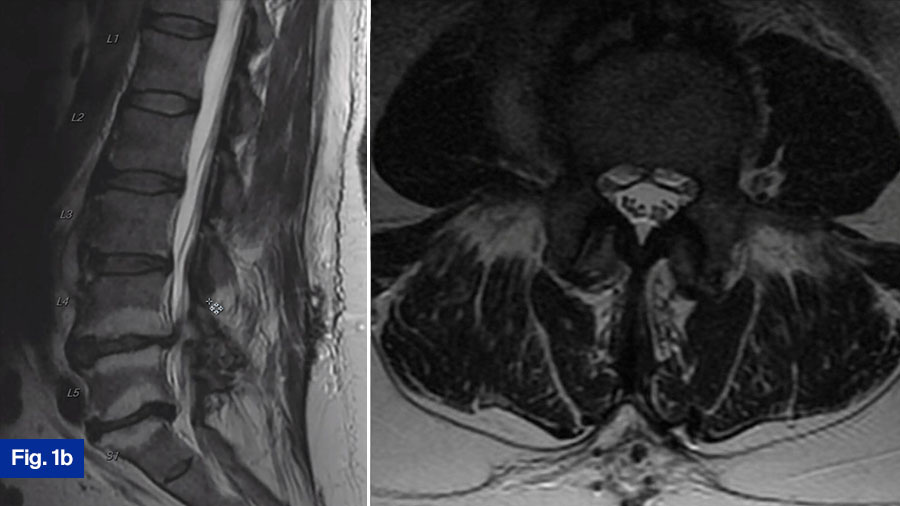
Upon presentation to the ED, he was initially treated with supportive measures/pain control for his back pain. His mention of fevers/chills prompted the ED staff to draw inflammatory labs, which were elevated. Additionally, blood cultures were draw, which eventually grew bacteroides. Due to the elevated blood cultures, and his unrelenting low back pain despite pain control efforts, advanced imaging was obtained. Noncontrasted computed tomography (CT) scan of his spine showed age-appropriate degenerative changes, but was negative for acute findings, and did not show any bony destruction (Figure 1a). A noncontrasted magnetic resonance imaging (MRI) scan of the spine was obtained, which demonstrated a small prevertebral collection without neural compression, and slight end-plate hyperintensity at the L3-L4 level. Additionally, there were L4-L5 and L5-S1 Modic changes (Figure 1b).
Expert opinions
Gregory Schroeder:
In this case, the patient has an infection without any neurologic symptoms, and without any neurologic compression. Furthermore, the CT scan does not show any significant bony erosion that would raise the possibility of instability. Given that the bacteria has already been identified in blood cultures, I would recommend targeted IV antibiotics for 6 weeks. I would follow the patient with serial blood work including ESR, CRP and WBC. As long as the patient was clinically improving, and the lab markers were normalizing, I would not get any further advanced imaging studies. While I routinely recommend a trial of non-operative treatment, I think it is important to highlight that there is a growing body of literature suggesting that early surgical intervention may be beneficial. Recently Thavarajasingam et al (Sci Rep. 2023) published a systematic review of patients with pyogenic spondylodiscitis and reported that early surgical intervention led to a 40% risk reduction in treatment failure rate and a 39% decrease in mortality rates. Because of studies like this, I think that early surgery is becoming much more common. However, at this point I do not think there is a clear consensus on the benefits of early surgical intervention; at my institution a trial of nonoperative management would be attempted before surgery.
Charlotte Dandurand:
In summary, this neurologically intact 56-year-old man presents with a new diagnosis of discitis osteomyelitis based on the CT and MRI findings. I would most often obtain a contrast-enhanced MRI to confirm diagnosis and complete investigations. Typical surgical indications in these cases are 1) neurological deficits, 2) instability, and lastly 3) medical treatment failure. The patient is neurologically intact. The CT scan and MRI show his spine to be stable with preserved alignment and no significant bony destruction. This is a new diagnosis, and full medical management has not been attempted. Furthermore, a bacterial pathogen has been identified allowing for targeted antibiotic therapy. Given the aforementioned factors, I would treat this patient nonoperatively with a full 6 weeks of antibiotics. I would involve the infectious diseases team who would guide targeted antibiotics treatment. Inflammatory markers would then be monitored overtime to determine response to treatment. A growing body of literature suggests that early surgical intervention may lead to improve biological cure rates but given the good clinical status of this patient and the relatively benign appearance of the imaging, I would treat this patient medically.
Actual treatment
He was initiated on intravenous antibiotics with Unasyn and was discharged with this treatment for two months. He was seen at the most recent follow-up visit by the infectious disease team and was doing well overall with full pain resolution. His PICC line was removed, and he will continue on oral antibiotics with Augmentin for a year.
Case 2: A 57-year-old male with polysubstance abuse and spinal cord compression
Patient presentation
The second case involves a 57-year-old male with a history of polysubstance abuse, including intravenous drug use and recent methicillin-resistant staphylococcus aureus bacteremia. Additionally, he has a history of chronic pain and uses daily fentanyl patches. He initially presented to the ED due to several weeks of non-mechanical mid-back pain. He denied preceding fevers/chills. On exam in the ED, he was neurologically intact and denied bowel/bladder symptoms.
Diagnostic workup
- CT scan: Demonstrated bony destruction and increased segmental kyphosis at T11-T12 (Figure 2a).
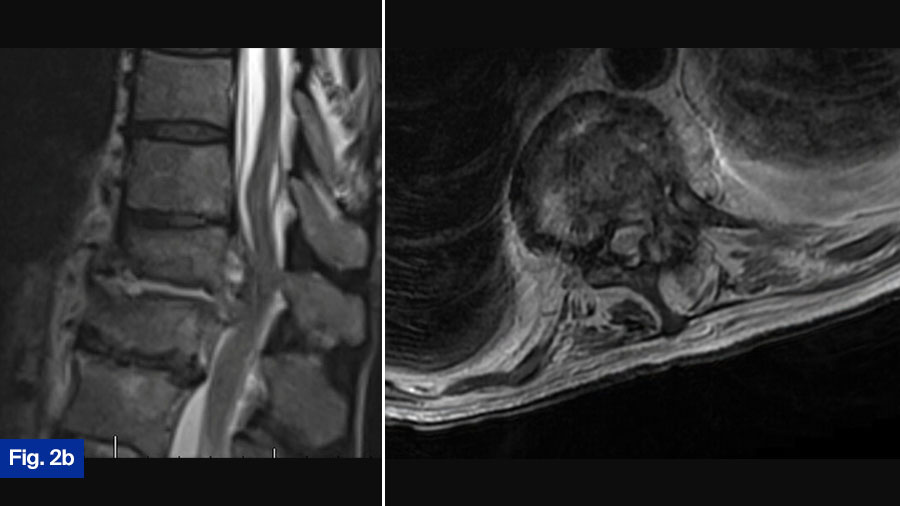
- MRI scan: Demonstrated a large ventral epidural phlegmon with moderate cord compression and thoracic hyperintensity with end-plate destruction (Figure 2b).
- Upright radiographs: Further evaluated spinal stability (Figure 2c).
Expert opinions
Gregory Schroeder:
This patient is the most controversial case. The patient is neurologically intact but has spinal cord compression from an infection. Furthermore, this patient has significant bony erosions. I would treat this patient with surgical intervention in an urgent manner. Significant infection around the spinal cord can cause a spinal cord injury from a mechanical mechanism, but it can also cause vasospasm and spinal infarction. When looking at cervical epidural abscess, Alton et al (TSJ 2015) found a 75% failure rate of medical management largely due to a progressive neurologic deficit. While undoubtably there is some difference between the thoracic and cervical spine, I treat all patients with significant spinal cord compression from an infection surgically. At my institution, this patient would routinely have a lateral partial corpectomy utilizing autologous iliac crest autograft, followed by an instrumented posterior decompression and fusion, The patient would routinely get 6 weeks of IV antibiotics, however the use of suppressive antibiotics after the completion of IV is often variable. While there can be significant debate about the best surgical treatment, I think this patient should undergo surgical intervention.
Charlotte Dandurand:
This case is certainly controversial. At my institution, when such a case is presented at rounds, the room is divided regarding best treatment (initial medical treatment versus initial surgical treatment). Interesting and lively debates occur. This patient presents with a new diagnosis of discitis/osteomyelitis with some bony destruction and epidural abscess. He is neurologically intact and upright radiograph show the segment to be stable. Given this, I would admit the patient and attempt initial medical management. I would monitor response to treatment clinically as well as via laboratory inflammatory markers. Often, in the context of infection that receives adequate medical treatment, we see fusion of the segment. However, this patient will need to be monitored closely once discharged from the hospital with regular clinical assessments with upright radiographs as well as close monitoring by the infectious disease team. It is still possible that this patient requires surgical intervention. Given the growing international academic interest in this disease and the possible growing evidence that initial surgical intervention is best, it is possible that my approach to these types of cases will change as we reach consensus on best treatment.
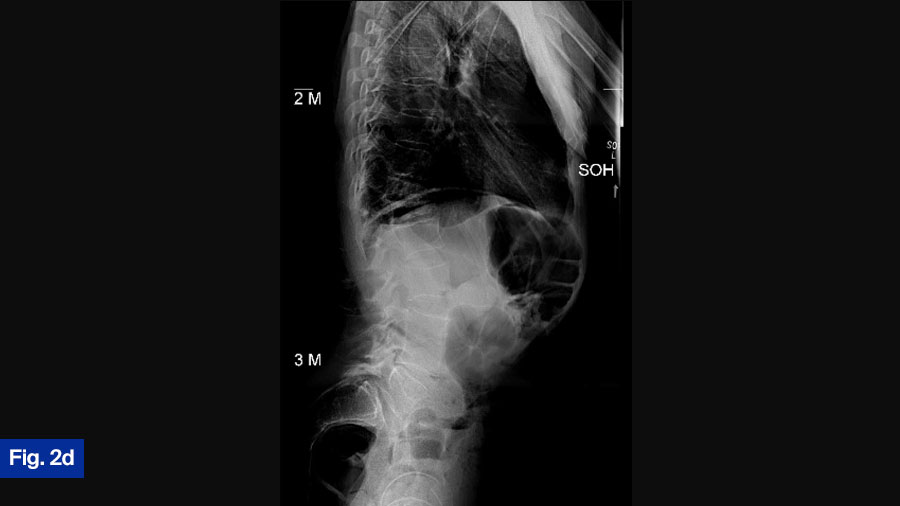
Actual treatment
Ultimately, the patient was treated with intravenous vancomycin for 8 weeks via PICC line—this included a 10-day inpatient stay prior to discharge. He was transitioned to oral antibiotics with Septra (sulfamethoxazole & trimethoprim) for 6 months. Standing films demonstrate adequate alignment (Figure 2D). Patient was doing well at the most recent follow-up and remained neurologically intact.
Case 3: A 63-year-old male with progressive neurologic deficits
Patient presentation
The third case includes a 63-year-old male with a past medical history that includes hyperlipidemia and uncomplicated hypertension. The patient experienced several months of neck pain, which was progressively worse in the week prior to their ED presentation. Additionally, within the week prior to their ED presentation, the patient started to experience progressive left-sided weakness. Upon arrival to the ED, the patient was unable to ambulate due to the left-sided lower extremity motor deficit. Incidentally, the patient also endorsed ~1 week of right-hand weakness that had resolved prior to showing up to the ED.
Diagnostic workup
- Inflammatory markers: Significantly elevated.
- Blood cultures: Grew MSSA (methicillin-sensitive Staphylococcus aureus).
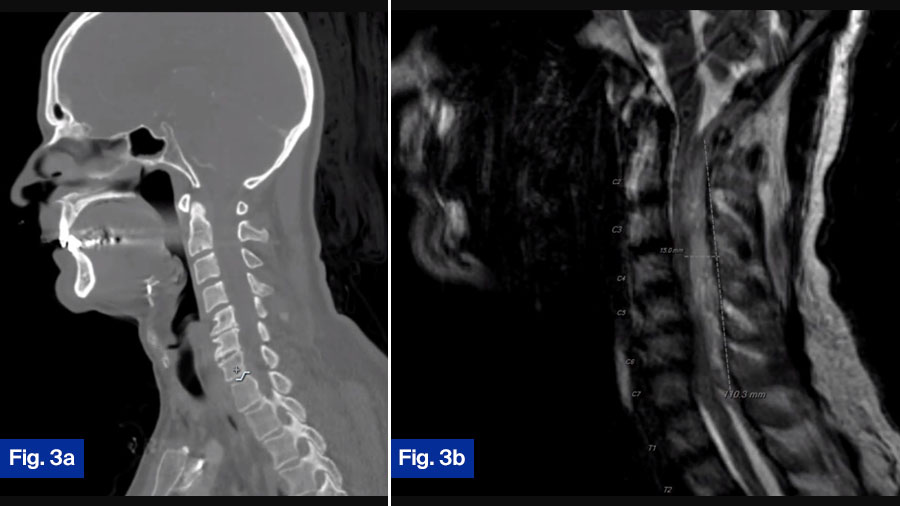
- CT scan: Showed minimal bony destruction (Figure 3a).
- MRI scan: Demonstrated a large dorsal epidural fluid collection spanning C2-T1 with substantial spinal cord compression (Figure 3b).
Expert opinions
Gregory Schroeder:
This patient has a large dorsal collection that is causing severe spinal cord compression and a neurological defect. This patient needs to go to the operating room emergently for a posterior cervical decompression and fusion. While there may, I think, be reasonable arguments for and against early surgical intervention in most patients with a spinal infection, I do not think there is any debate about patients with an acute neurologic deficit. All of these patients should go emergently to the OR.
Charlotte Dandurand:
This 63-year-old man presents with severe progressive neurological deficits in the context of large cervical epidural collection causing cord compression. This patient undoubtably needs to be taken to operating room for emergent cord decompression. This patient would receive a posterior decompression and fixation. In such cases with neurological deficits, I think there is consensus within the spinal surgical community regarding proceeding to emergent surgical management.
Actual treatment
The patient was taken urgently for C2-T1 laminectomy, and C2-T1 posterior cervical fusion (Figure 3c). The patient was covered postoperatively with IV Nafcillin for 2 months, and then transitioned to oral antibiotics. The patient was doing well at final follow-up and was able to ambulate slowly, but without difficulty. Neurologic deficits resolved.
Conclusion: the need for a standardized approach to spinal infections
These three cases highlight the complexity of spinal infections, and the need for a globally accepted classification and treatment algorithm. There is such a paucity of high-quality literature available on the treatment of spinal infections, that the management is widely variable even for seemingly routine cases. It is the goal of the AO Spine Trauma and Infection knowledge forum to help develop a classification, as well as to perform prospective, multinational studies that will allow for the development of an evidence-based and globally accepted treatment algorithm.
About the authors:
Dr Jonathan Dalton is currently pursuing a two-year fellowship in spine surgery and spine research at the Rothman Orthopaedic Institute in Philadelphia, PA. Dalton completed his residency in Orthopaedic Surgery at the University of Pittsburgh Medical Center in Pittsburgh, PA and attended medical school at Washington University School of Medicine in St. Louis, MO. He has authored over 40 peer-reviewed manuscripts, and continues to actively produce research during his fellowship at the Rothman Orthopaedics Institute.
Dalton is a member of AO Spine and has particular research interest in outcomes following spine trauma and infections.
Dr Gregory Schroeder is a fellowship trained spine surgeon, who currently serves as Associate Professor of Orthopaedic Surgery at Thomas Jefferson University. Schroeder completed his residency in Orthopaedic Surgery at Northwestern University Feinberg School of Medicine in Chicago, IL. He followed with a fellowship in spine surgery and spine research at the Rothman Orthopaedic Institute in Philadelphia, PA.
Schroeder is the chairperson on AO Spine Knowledge Forum Trauma and Infection. He has authored hundreds of peer-reviewed publications, has edited numerous textbook chapters, and has presented both nationally and internationally on spine surgery research and techniques. He has chaired multiple international spine surgery meetings including the Cervical Spine Research Society, and the North American Spine Society’s summer meeting. He holds several editorial positions, including Editor-in-Chief for Clinical Spine Surgery in Philadelphia, PA. He has conducted extensive research in the field of spine surgery and continues to actively do so.
Dr Dandurand’s research interests concentrate on spinal trauma research and clinical outcomes of spine surgery. She is an associate member of AO Spine Knowledge Forum: Trauma, an international multi-disciplinary panel of experts pursuing innovative research into spinal trauma. She is also an active member of the Canadian Spine Society and North American Spine Society.
Dr Dandurand completed residency in neurosurgery at the University of British Columbia, in addition to a program of clinical effectiveness and Master of Science in epidemiology at Harvard University. Her fellowship in advanced spine surgery was completed at the University of British Columbia/Vancouver General Hospital.
You may also be interested in...
Primary spinal infections
Examining infections of the intervertebral disc, vertebral body, medullary canal, or adjacent paraspinal structures
AO Spine KF Trauma and Infection
Addressing the growing health care issues of spinal trauma and infection to improve patient care and advance knowledge
New Special Issue of Global Spine Journal
Exploring factors that influence decision-making in thoracolumbar burst fractures without neurological deficit
Global Spine Congress 2025, Rio, Brazil
Join us to exchange ideas, network with fellow spine professionals, and discover new research and technologies