Sacral fractures: bridging spine and pelvic surgical expertise
BY DR ASHRAF N EL NAGA AND DR EMILIANO VIALLE

Sacral injuries are a highly diverse group of injuries, ranging from low-energy fragility fractures in elderly patients to devastating lumbopelvic dissociations seen in high-energy trauma. These injuries can involve only the sacrum or extend to the pelvic ring and the lumbosacral junction, creating complex treatment challenges. Accurate diagnosis, classification, and thoughtful treatment plans—whether nonoperative or surgical—are essential to optimizing outcomes and maximizing patient function.
-
Read the quick summary:
- Experts from spine and trauma surgery discuss collaborative approaches to managing complex sacral fractures.
- Combined expertise in spine and pelvis surgery improves alignment, stability, and neurologic recovery in sacral fracture care.
- Surgeons can apply the AO Spine Sacral Injury Classification System and minimally invasive fixation techniques to optimize patient outcomes.
- Future focus includes expanding spine surgeon roles, advancing minimally invasive methods, and evaluating new navigation technologies.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Sacral injuries are at a crossroads of specialties
The sacrum sits at the intersection of two major disciplines: the spine and the pelvis. From a global perspective, there is a high variability in whether patients with sacral fractures are assigned to orthopedic traumatologist or spine surgeons. However, it is no surprise that treating sacral injuries sometimes requires the combined expertise of both orthopedic traumatologists and spine surgeons.
Orthopedic traumatologists provide:
- Deep understanding of pelvic ring biomechanics
- Mastery in fracture reduction and fixation of anterior pelvic ring components
- Nuanced knowledge of injury patterns and fracture stability
- Emergency care and treatment in polytraumatized patients, including temporary stabilization techniques like external pelvic fixators
- Treatment planning and coordination of surgical timing in polytrauma patients
Spine surgeons provide:
- Expertise in lumbosacral stability and posterior spine-based instrumentation techniques
- Management of ongoing neurologic compression when present (e.g., acute cauda equina syndrome or nerve root injury)
- Correction techniques to address sacral kyphosis and complex deformity
- Understanding of advantages of enabling technologies such as CT based navigation and percutaneous spine instrumentation
Treatment goals and principles
The ultimate goal in treating sacral fractures is to facilitate and expedite a patient’s return to their pre-injury level of function. To achieve these goals, it is essential to promote healing in proper alignment while optimizing neurologic recovery and accelerating post-injury rehabilitation. Often, this means striking a balance between doing enough and doing no more than necessary.
Key objectives include:
- Fracture healing in physiological alignment
- Early mobilization and weight bearing when possible
- Minimizing the invasiveness of surgical techniques to achieve goals
Treatment decisions are guided not only by the injury itself but also by the patient’s specific bony anatomy (i.e. pelvic dysmorphism), associated injuries, comorbidities, functional status, and ability to adhere to weight-bearing restrictions.
When is surgery indicated?
When nonoperative care is insufficient, surgery typically aims to achieve three things:
- Decompress the neural elements
- Bring the sacrum and pelvic ring into physiologic alignment
- Provide stable fixation to promote early mobility and healing
This often involves interdisciplinary planning to ensure optimal timing, technique, and construct durability.
Modern classification: AO Spine Sacral Injury Classification System
Historically, a variety of sacral and pelvic fracture classification systems (e.g., Denis, Isler, Roy-Camille, Young-Burgess, Tile) have been used and each advanced our understanding of salient injury characteristics. However, until recently, no unified framework existed.
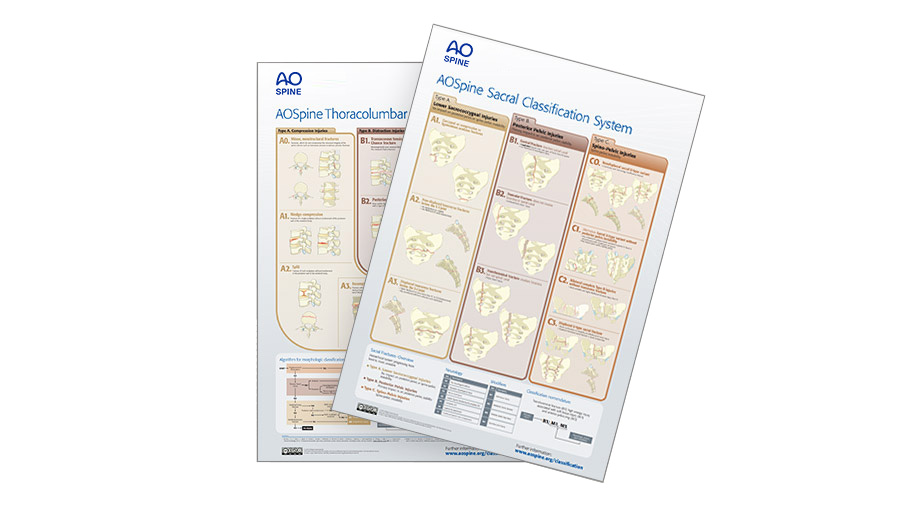
That changed with the AO Spine Sacral Injury Classification, a collaboration between AO Spine and AO Trauma experts. This system categorizes injuries into three hierarchical types—progressing from stable to unstable—to help guide treatment, research efforts, and prognosis.
Injury-specific considerations include:
- For vertical injury patterns (e.g. B type, C1, and C2 injuries): Recognition of L5-S1 facet involvement, vertical hemipelvis translation, transitional anatomy (e.g., sacral dysmorphism), and weight-bearing goals
- For transverse injuries (e.g. Type C0 and C3 injuries): Recognition of the degree of sacral kyphosis, neurologic status, and lumbosacral dissociation

C0
This is a nondisplaced sacral U-type fracture, typically resulting from low-energy injuries. These injuries are most commonly seen as insufficiency fractures in patients with metabolic bone disease.
Source: AO Surgery Reference

C1
This is any unilateral B-type fracture involving a fracture of the ipsilateral L5-S1 joint. This fracture type may impact spino-pelvic instability and is therefore classified as a C fracture.

C2
This is a bilateral B-type fracture without a transverse component. These fractures are more unstable and have a higher risk of neurological injury than C1.

C3
This is a displaced U-type fracture. It has a similar instability profile as C2, but due to the transverse fracture displacement it has a higher likelihood of neurological injury.
How to formulate a surgical plan?
Treatment options for this diverse set of injuries ranges from percutaneous iliosacral screw fixation to open lumbopelvic techniques. For surgeons, a structured approach to planning is essential with consideration given to the following questions:
- Is neurologic decompression needed?
• This is reserved for cases with ongoing symptomatic neural element compression - How will the fracture be reduced?
• Typically, progression is from closed and percutaneous methods to open techniques in order to achieve an acceptable reduction while weighing the risks and benefits of increasing surgical invasiveness - Is lumbosacral fusion required?
• Primary lumbosacral fusion is considered when there displaced L5/S1 facet articulation - What instrumentation technique is best suited?
• This is based on a patient’s injury and underlying anatomy and available bony corridors for instrumentation
• Consideration is preferentially given to percutaneous instrumentation/or minimally invasive methods - Is fixation of the anterior ring required?
- Will the fixation allow for early weight bearing?
- What is the optimal timing of the surgery considering a patient’s global picture and associated injuries?
Answering these questions helps tailor treatment to both the injury and the individual.
Looking ahead: the role of minimally invasive techniques
We’re entering a new era of sacral fracture management. Minimally invasive sacropelvic techniques allow for earlier mobilization, less morbidity, and quicker recovery.
While spinopelvic fixation has traditionally been reserved for complex transverse injuries, its use in vertically oriented fractures is gaining interest. There’s untapped potential in expanding spine surgeon involvement—even in cases previously managed solely by trauma teams with their expertise being instrumental in achieving biomechanical goals and facilitating earlier weight bearing and recovery.
Further, there is interest in evaluating the utility of enabling technologies such as navigation, robotics, and augmented reality.
Final thoughts
Historically, sacral fracture management has been the domain of orthopedic traumatologists. But as treatment strategies and options evolve, the involvement and insights of spine surgeons can bring significant value. Together, a collaborative, multidisciplinary approach ensures patients receive the best possible care—bridging the gap between pelvic trauma and spinal injury for optimal patient recovery and outcomes.
About the authors:
You might also be interested in...
AO Spine Injury Classification Systems downloads
The most comprehensive classification system devised for thoracolumbar spine.
AO Spine Knowledge Forum Trauma and Infection
Leading the globe in generating the knowledge that improves patient care after suffering from spine trauma and infection.
Minimally Invasive Spine Surgery (MISS)
AO Spine educational material and courses cover all types of MISS operations through tubular/microscopic, endoscopic, and instrumented procedures.
Sacral trauma on AO Surgery Reference
A classification system describing injuries based on three criteria: morphology of the injury, neurologic status, and case-specific modifiers.