Classifying civilian thoracolumbar gunshot wounds: a step toward better treatment decisions
BY DR GUILLERMO RICCIARDI
Gunshot wounds to the spine are often assumed to be mechanically stable, but there is no consensus on how to define or classify unstable fracture patterns properly, so the assumption can mislead treatment planning. The key to better outcomes is not only recognizing when an injury is unstable but also having a reliable framework to guide decisions on surgical versus non-surgical management.
A recent systematic review Mechanical Instability After Civilian Thoracolumbar Gunshot Injuries in the Global Spine Journal highlights the absence of standardized definitions for mechanically unstable civilian thoracolumbar gunshot injuries and aims to support classification development. Notably, vertebral body comminution emerges as a consistent indicator of instability in these cases.
-
Read the quick summary:
- Civilian spinal gunshot wounds: focus on instability and treatment
- Instability is rare (<10%), but comminution + pedicle/facet fractures are key red flags
- Surgeons can use emerging classification patterns to guide stabilization decisions
- Next step: consensus-based classification integrating mechanical, ballistic, and biological factors
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Why instability matters in treatment
Most civilian thoracolumbar gunshot injuries are mechanically stable, meaning they can often be managed without surgery. However, in the small subset of unstable injuries—typically less than 10%—the risk of progressive deformity, neurological deterioration, and chronic pain is high. Recognizing these cases early is critical to avoid missed opportunities for stabilization.
The consistent red flag across the literature is severe vertebral body comminution, especially when combined with pedicle or facet fractures. These patterns, along with posterior ligamentous injury, can shift an injury from stable to unstable and change the treatment plan dramatically.
Why blunt trauma classifications fall short for spinal gunshot wounds
Spinal gunshot wounds require a specialized approach and classifications designed for blunt trauma, such as the AO Spine Thoracolumbar Injury Classification System, are not validated for penetrating injuries. Gunshot wounds have unique mechanical and biological features shaped by ballistics—projectile type, velocity, trajectory, fragmentation, and even lead toxicity.
Additionally, gunshot wounds can display distinctive injury patterns that are uncommon in blunt trauma, for example, bilateral pedicle or facet fractures, such as those caused by a gunshot with a lateral projectile trajectory. These factors not only influence the pattern of injury but also the choice of treatment, from stabilization techniques to monitoring for systemic complications.
Previous specific classifications of spinal gunshot wounds, like the one presented by Steverlynlk et al., lack validation and broad acceptance, highlighting the need for a more comprehensive system that addresses the mechanical stability gap.
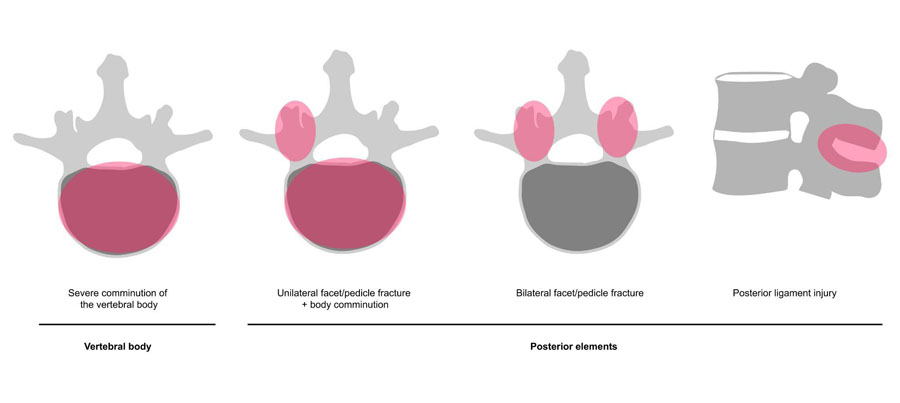
Four recurrent unstable patterns clinicians should know
The recurring unstable injury patterns provide insight into where instability is most likely to occur and highlight a potential foundation for building a classification framework.
Across reported cases, four injury patterns stand out as warning signs for mechanical instability:
- Severe vertebral body comminution
- Unilateral pedicle or facet fracture with comminution
- Bilateral pedicle or facet fractures
- Posterior ligamentous injuries
Identifying these patterns on CT or MRI provides practical guidance in deciding when surgical stabilization is warranted.
Towards a dedicated classification for clinical use
A classification system tailored to gunshot injuries could help standardize treatment decisions and improve outcomes. We aim to identify risk factors associated with mechanical instability in civilian thoracolumbar gunshot wounds, providing evidence to support the development of a new classification system for these injuries.
Following PRISMA 2020 guidelines, we reviewed 2,400 records and included 33 studies involving 3,195 civilian thoracolumbar injuries (T1–L5). Building on the AO Spine framework, a proposed adaptation integrates the findings:
• Mechanical factors (degree of comminution, ligamentous disruption)
• Ballistic factors (weapon type, muzzle velocity, projectile location)
• Biological considerations (viscera perforation, lead levels, cord transfixion)
Such a system would allow surgeons to assess risk consistently, communicate clearly across teams, and align treatment with the specific challenges of penetrating injuries.
While the AO Spine system was designed for blunt trauma, its hierarchical framework offers a flexible platform for penetrating injuries if expanded with relevant modifiers. The injury patterns associated with these cases may fit within the hierarchical structure. A preliminary proposal is shown in Table 1 as an adaptation of the AO Spine system for civilian thoracolumbar gunshot injuries.
| Table 1. Thoracolumbar Gunshot Wound Classification Framework | |
| Type and Description | |
| A0 | Isolated fractures of the posterior arch, spinous process, and transverse process |
| A1 | Fractures involving the vertebral body—One endplate involved |
| A2 | Fractures involving the vertebral body—Both endplates involved |
| A3 | Fractures involving the vertebral body—One endplate and posterior wall involved |
| A4 | Fractures involving the vertebral body—Both endplates and the posterior wall involved |
| B1 | Fractures involving the pedicles and/or the facets, whether unilateral or bilateral |
| B2 | Fractures in which there is evidence of posterior ligamentous complex disruption |
| B3 | Fractures in which there is evidence of anterior tension band disruption, with or without a projectile lodged in the disc |
| C | Injuries indicative of displacement or dislocation |
| Potential modifiers |
|
Practical impact for care of civilian patients with gunshot wounds
For most patients, conservative management of gunshot wounds remains safe and effective. But for those with the identified unstable patterns, early recognition and stabilization can:
- Prevent late deformity and chronic pain
- Reduce risk of secondary neurological decline
- Provide a structured pathway for surgical planning
- Support rehabilitation with greater confidence in spinal stability
The current evidence base is heterogeneous, but progress is underway toward consensus through morphology-based studies and Delphi methodology. The ultimate goal is an evidence-driven classification that bridges radiology, surgery, and rehabilitation—bringing clarity to a complex area of spine trauma and, most importantly, improving patient outcomes.
About the author:
Dr Guillermo Ricciardi, MD, MSc, is an orthopedic spine surgeon at Centro Medico Integral Fitz Roy, Sanatorio Guemes, and Hospital Alvarez in Buenos Aires, Argentina.
Dr Ricciardi is a member of the AO Spine Trauma Latin America Study Group.
Acknowledgments
This study was organized by the AO Spine Latin America Trauma Study Group. Study support was provided directly through AO Spine Latin America regarding data collection, data analysis, and proofreading. The authors would like to thank Idaura Lobo and Carla Ricci (AO Spine) for their administrative assistance. Additionally, a thank you is directed towards the members of the AO Trauma Study Group, including Charles André Carazzo, Dr. Alfredo Guiroy, Guisela Quinteros, Jose Rafael Dangond, Juan Ignacio Cirillo, Juan José Zamorano, Juan Pablo Cabrera, Ratko Yurac, and Joana Guasque.
The authors also extend their gratitude to all investigators and healthcare professionals involved in the management and study of spinal gunshot wounds, whose valuable contributions were essential to the completion of this research, including Dr. Jorge Cabrera Escamilla, Dr. Victor Davila, Dr. Sebastian de la Torre, Dr. Omar Hernandez, Dr. Cristobal Herrera Palacios, Dr. Jose Marıa Jimenez Avila, Dr. Arturo Rodriguez Montalvo, Dr. Janicke Rodriguez, Dr. Alvaro Rocchietti, Dr. Luis Saavedra, Dr. David Servin, and Dr. Hugo Tejerina.
References and further reading:
- Ricciardi GA, Cirillo I, Cabrera JP, et al. Mechanical Instability After Civilian Thoracolumbar Gunshot Injuries: A Systematic Review to Support Classification Development. Global Spine Journal. 2025;0(0). doi: 10.1177/21925682251379371
- Steverlynck A, Castelli R, Astiasaran J, Rullan Corna A, Ricciardi D, Vadra G. Heridas por proyectiles de arma de fuego en la columna vertebral. Rev. Asoc. Argent. Ortop. Traumatol. 2001;66(4):261-267.
- Barros TE, Zigler J, Aito S, Di Lorenzo N, Wing P. Gunshot wound to the spine. Spinal Cord. 2001;39(10):541-544. doi: 10.1038/sj.sc.3101186
You might also be interested in...
AO Spine Classification Systems
The AO Spine Classification Group, International Board, and Knowledge Forum Trauma collaborated on a classification that incorporates both fracture morphology and clinical factors relevant for clinical decision making.
Latin America research study groups
As part of AO Spine’s mission to promote excellence in the treatment of spinal pathologies, AO Spine Latin America launched regional Study Groups and a range of research support opportunities, including technical assistance and funding.
Global Spine Journal
AO Spine’s official scientific journal is an open access, peer-reviewed journal focusing on the study and treatment of spinal disorders.