Active Apex Correction (APC): innovative non-fusion technique for Early Onset Scoliosis treatment
BY DR ALAAELDIN AHMAD

Early onset scoliosis (EOS) is defined as a deformity in the spine of a growing child which develops before the age of 10 years. (1,2) The spinal deformity, regardless of etiology, produces vertebral rotation that obliterates lung space. The treatment of EOS aims to halt and correct the deformity, while preserving spinal growth and maximizing thoracic volume to allow for cardiopulmonary growth and to avoid respiratory compromise and cardiac diseases. (1-3) Initial treatment consists of non-operative methods (bracing and/or corrective casting), which are used to delay or avoid the need for spinal surgery.
However, treatment is challenging in rapidly progressive curves and hence surgical ‘growth-friendly’ corrective techniques are often necessary. (1,4,5) In this article I explore Active Apex Correction (APC), an innovative and widely accessible solution for treating EOS.
-
Read the quick summary:
- Alaaeldin Ahmad discusses the APC technique for treating early onset scoliosis, highlighting its development and global use.
- APC offers apical control through non-fusion, reducing complications and costs while preserving spinal growth.
- Clinicians can explore APC as a scalable, efficient alternative to traditional methods, especially in resource-limited settings.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
This article refers to the Global Spine Journal Best Paper Award winner: Ahmad M. Hammad, Mohammad Emar, Farah Shahin, et al. A Prospective Multicenter ≥2 Years Clinical Study of the Active Apex Correction (APC) Technique in Early Onset Scoliosis (EOS) Patients, Global Spine J. 2024;15(2):1174-1185. Alaaeldin Ahmad will receive the award at the Global Spine Congress 2025 ceremony in Rio de Janeiro.
Evolution of surgical techniques in EOS management
Multiple surgical techniques have been devised in an aim to maintain a mobile growing spine while preserving lung growth and minimizing the risk of complications. (6) Traditional growing rods (TGR) is the most frequently used technique in EOS management; however, this requires lengthening procedures repeatedly every six months and therefore accompanied by higher complication rates and costs. (3,7)
As a result, several methods have been recently described and introduced to overcome the need of repeated reoperation, including magnetically controlled growing rods (MCGR) and the SHILLA growth guidance system. (3,8)
- MAGEC is similar to TGR but the distractions are done transcutaneously every two months; the main drawbacks are high cost of the implants needed, possible mechanical complications and unplanned surgeries, and metallosis.(9,10)
- SHILLA, on the other hand, was developed by McCarthy as guided growth-based technique to control the apex of the curve, so as to guide spinal growth and to decrease the number of frequent reoperations. It is performed by correction and fusion of 3-4 levels around the apical vertebra with proximal and distal sliding of the rods guiding growth. (6) However, this technique has been found to be accompanied by an increased risk of unplanned surgeries from loss of correction secondary to crank shafting, adding on, screw pull-out and rod breakage, and by complications associated with osteotomies performed on the concave side of the curve. (11,12,13)
The gap in care for low-middle income countries (LMICs)
Further complicating matters, for patients in low-middle income countries (LMICs) surgical choices for early onset scoliosis surgery service have typically been even more limited. The surgeon may be able to perform traditional growing rod but only with years of frequent surgeries and bearing the risk of extensive possible patient complications.
Or, as an even less available option, the surgeon may perform expensive surgeries such as SHILLA or MCGR—which most institutes cannot afford, and which still come with a high rate of complications that are difficult to manage locally.
The shift toward growth-modulating approaches
Fortunately, there has been a transition recently towards techniques which aim to restore a harmonious balanced spine and to preserve growth and mobility of the apex. The goal is to achieve physiological correction of deformity by controlling asymmetric growth with modulation over time at a low complication rate (4).
Introducing Active Apex Correction (APC)
In this vein, APC is an innovative technique based on apical tethering through posterior approach proposed to overcome the disadvantages of other procedures. (6)
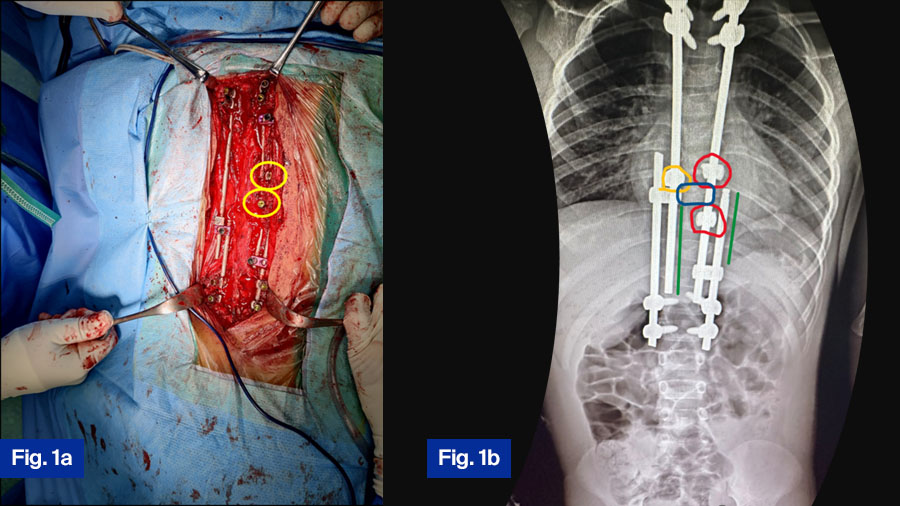
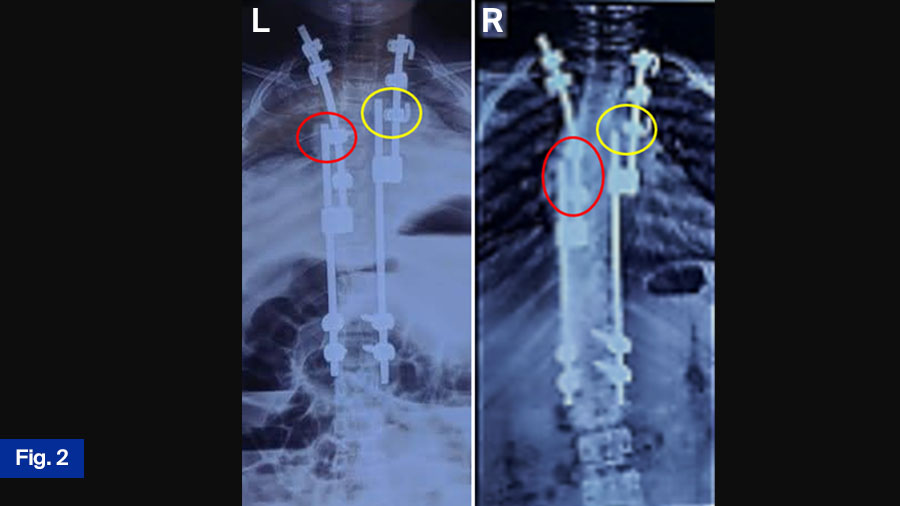
APC is a hybrid of guided growth and apex control through non fusion and reversed modulation-based philosophies for management of growing-spine deformity. It replaces the apical fusion of a traditional SHILLA with procedures (compression/distraction + medial translation + derotation) against primary drivers of curve progression, as shown in Figure 1, Figure 2.
The APC technique was pioneered sixteen years ago in Palestine and has been performed on a regular basis as the main surgical procedure for early onset scoliosis cases in Palestine over the past twelve years.
Research and evidence supporting APC
The reader can refer to the surgical details in the recent multicenter study paper published in GSJ 2024 about APC (14). Another study, a 2019 computational virtual study in the spine lab at the University of Toledo, USA, reveals the apical posterior tethering effect on modulation and spine growth in the finite element study, reinforcing the aforementioned clinical results.
In total, since 2016, eight papers (14,15,16,17,18,19,20,21) have been published in peer reviewed journals about APC technique, propelled in part by international attention to this innovative technique and the multiplicity of centers that have worked with it. The latter cooperation has translated into multicenter studies that demonstrate promising results with short term follow up in comparison to other non-fusion techniques.
One review by Latalski et al. found that the most frequent complications in traditional techniques were implant related and that incidence of complications can be underestimated; they found that 54% of the patients required unplanned surgeries (4) whereas in the APC multicenter study (14) there were only 3 unplanned surgeries i.e., 12.5% of patients.
Recently, we have focused on more detailed studies about the attitude of the apex with this posterior tethering technique, focusing on the non-fusion and vertebral modulation of the apex. One study (17) reveals 84% of non-fusion of the apex in both concave and convex sides. Another research paper, currently in progress, is revealing that there is growth in the convex and concave sides of the apex with clear modulation of the tethered apical vertebrae.
These studies are important in clarifying the difference between the APC and the SHILLA or the CGA (Convex Growth Arrest), proving that APC is mainly apical control with non-fusion and modulation through posterior tethering.
Technical refinements and surgical modifications in APC
Over the past decade, my global activities and the dissemination of this technique in many centers globally have added to the APC pathway. I have shared experiences in APC surgery and discussed new ideas with fine colleagues, leading to continued refinement in the efficiency of this technique. We have had the opportunity to develop refinements and modifications in accordance with the lab studies and the global experiences we shared with colleagues, such as:
- Stressing on putting the 5.5 rod titanium or 4.75 CC as tethered rod, instead of using the 4.5 rod as the tethering one.
- Using dominos with a hole equal to the rod diameter to overcome soft tissue impinging preventing rod sliding, shown in Figure 2.
- Using screws instead of rib hooks as proximal anchors to increase the medial translation of the apex by connecting the tethered screws with the proximal anchors in case of thoracic apical curve. This goes with the geometry of the corrected spine, reducing stress discontinuity and avoiding a junctional area between the apex and the non-instrumented spine above and below. The latter may be the main reason for the decreased incidence of crankshaft phenomena, rod fracture, besides the good correction post operatively.
- Avoiding using dominos in index surgery of the kyphotic deformity during APC surgery maximizing the effect of Heuter Volkmann’s law on the apical area.
APC as a scalable, affordable solution in global health
I view APC not in the narrow terms of a surgical technique (only), but as part of a vision to democratize medicine by making it affordable and accessible within any healthcare context. I sometimes refer as illustration the example of the car industry, which flourished only after Henry Ford had the idea of a production line that could make cars accessible to the middle class.
With surgery service including early onset scoliosis surgery, spreading it globally entails getting the technique to be simple, affordable, accessible, with short learning curve, and with good results comparable to other techniques. APC provides the chance to translate all these points into action.
Summary of advantages of the APC technique
As a summary, the advantages of APC include the following:
- It is a new idea (controlling the apex through non fusion and modulation) which nonetheless does not need to go first through paperwork and approval from the MOH, since the surgeon does not use any new tool outside what is used traditionally.
- It is a posterior tethering procedure which most spine surgeons are used to, unlike other approaches that need a steeper learning curve.
- The surgeon has no need to go through risky procedures like osteotomies or putting screws on the concave side.
- Using 2 screws to control the apex only on the convex side instead of 6 in SHILLA decreases the cost, in addition to avoiding risks of putting screws on the concave side
- It can be used with cases with 2 structural curves, which can be both controlled with the APC non fusion technique; this is unlike doing fusion for 2 curves which would eliminate any future growth.
- It is an efficient procedure since it goes with the geometry of the spine to better control the apex, especially in non-flexible big curves.
- It is one of the few techniques which can be used efficiently in kyphosis deformity.
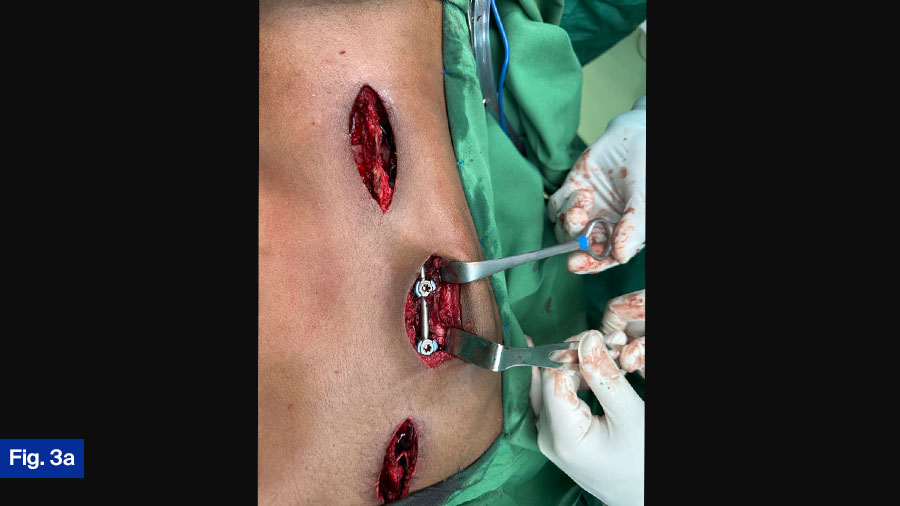
- It can be performed with a less invasive technique by opening limited incisions, proximal anchors one, one on the apex, and one for distal anchors (Figure 3).
- It uses relatively affordable implants, as all the surgeon needs are regular rods, screws, and dominos, therefore allowing surgeons in many LMICs to perform this surgery with good control. In addition, they can avoid the difficulties and costs of going through recurrent distraction surgeries.
- It has a short learning curve as the surgeon who knows how to put screws only needs to learn how to put the apical screws through Wiltse technique and how to do Compression/distraction + medial translation+ derotation. This can be learned after guided performance a few times.
- The surgeon has a plan B with this technique: if there is crankshafting with less control on the apex, they can go back and try more translation and compression distraction without the need to replace any of the implants.
- The control of the apex through non fusion and modulation preserves growth posteriorly, decreasing the incidence of crank shaft in comparison with the SHILLA (62% in comparison to 20%).
- Using the non-fusion modulation apex control in adjunction with growth guidance with rod gliding will overcome the problem of recurrent distraction surgeries. This relieves a large logistical and financial burden on the child and the family, in addition to decreasing the incidence of complications.
- Although in the beginning of dissemination we focused on APC as an excellent choice for surgeons in LMICs, we have since realized and reaffirmed that it is an effective and beneficial technique to perform more generally across the world.
The APC technique is now popular in relatively developed countries (Italy, USA, Saudi Arabia, UAE, Oman, England, Nederland, and South Africa) in addition to countries with more limited resources (Palestine, Jordan, Egypt, India, Pakistan, Vietnam, Nigeria, Tanzania, and Mozambique).
Recognition and future outlook
Reaffirming these benefits, I continue to receive highly encouraging comments from the surgeons who have adopted this technique, and to my knowledge none of them stopped using it. I was also fortunate that the technique was recognized locally in Palestine by winning the best innovation in health in 2023 from the domestic Higher Council for Innovation and Excellence and proud that the APC was innovated in Palestine and developed through servicing the needs of Palestinian children.
I am also fortunate and humbled to receive the global recognition of the APC innovative technique by winning the best paper published in Global Spine Journal 2024 which was about the APC. (14)
Moving forward with data and multicenter studies
On a concluding note, we are fortunate to have the data of more than 100 patients who were treated with this technique by excellent surgeons in developed and developing countries, giving us the chance to do more multicenter studies related to the efficiency of this technique. However, as the APC technique has been recently described, there is no long term follow up data yet. I hope that these studies will be a step on the way not only to evaluate the technique and its potential benefits, but also to add to the knowledge related to modulation in growing spine.
For more information, please contact the author Dr Alaaeldin (Alaa) Ahmad by email.
About the author
Dr Alaaeldin (Alaa) Ahmad is an experienced pediatric orthopedic surgeon from Palestine and Professor in the Palestine Polytechnic University. He has published more than 40 papers and chapters in international peer-reviewed journals and books. His interest areas include pediatric spinal surgery and club foot management, with special focus on early-onset scoliosis, minimally invasive techniques in pediatric spine deformity, and accelerated Ponseti technique.
Ahmad is internationally active, running and participating in several clinical programs with an educational focus in Asia, Africa, and Latin America. He co-authored the book Early-Onset Scoliosis—Guidelines for Management in Resource-Limited Settings (Taylor and Francis). He also participates in the governance and programs of several international spine organizations, the SRS, SICOT, AO Spine, NASS, Eurospine, and the PanArab Spine society.
Over the last 15 years Ahmad has developed a novel technique, Active Apex Correction (APC), for surgical management of EOS. This technique has proved to be reliable, accessible, and affordable in developed and developing countries with results published in several peer reviewed global journals and continued plans for multicenter studies.
References and further reading:
-
Schlösser T, Kruyt M, Tsirikos A, Surgical management of early-onset scoliosis: indications and currently available techniques, Orthopaedics and Trauma 2021; 35 (6): 336-346.
-
Williams BA, Matsumoto H, McCalla DJ, et al. Development and initial validation of the classification of early-onset scoliosis (C-EOS). J Bone Joint Surg Am 2014; 96: 1359e67.
-
Kim G, Sammak SE, Michalopoulos GD, et al. Comparison of surgical interventions for the treatment of early-onset scoliosis: a systematic review and meta-analysis [published correction appears in J Neurosurg Pediatr. 2023 Jan 13;31(4):388]. J Neurosurg Pediatr. 2022;31(4):342-357.
-
Latalski M, Fatyga M, Sowa I, Wojciak M, Starobrat G, Danielewicz A. Complications in growth-friendly spinal surgeries for early-onset scoliosis: Literature review. World J Orthop. 2021;12(8):584-603.
-
Skaggs DL, Guillaume T, El-Hawary R, Emans J, Mendelow M, Smith J. Early onset scoliosis Consensus Statement, SRS growing spine committee, 2015. Spine Deformity 2015; 3: 107.
-
Ahmad AA. Early onset scoliosis and current treatment methods. J Clin Orthop Trauma. 2020;11(2):184-190.
-
Helenius IJ, Oksanen HM, McClung A, Pawelek JB, Yazici M, Sponseller PD, Emans JB, Sánchez Pérez-Grueso FJ, Thompson GH, Johnston C, Shah SA, Akbarnia BA. Outcomes of growing rod surgery for severe compared with moderate early-onset scoliosis: a matched comparative study. Bone Joint J. 2018;100-B:772–779.
-
Andras LM, Joiner ER, McCarthy RE, McCullough L, Luhmann SJ, Sponseller PD, Emans JB, Barrett KK, Skaggs DL Growing Spine Study Group. Growing Rods Versus Shilla Growth Guidance: Better Cobb Angle Correction and T1-S1 Length Increase But More Surgeries. Spine Deform. 2015;3:246–252.
-
Kwan KYH, Alanay A, Yazici M, et al. Unplanned Reoperations in Magnetically Controlled Growing Rod Surgery for Early Onset Scoliosis With a Minimum of Two-Year Follow-Up. Spine (Phila Pa 1976). 2017;42(24):E1410-E1414.
-
Odent T, Ilharrebordeb B, Miladi L. Fusionless surgery in early-onset scoliosis. Orthopaedics & Traumatology: Surgery & Research 101 S281eS288. 2015
-
Wilkinson JT, Songy CE, Bumpass DB, McCullough FL, McCarthy RE. Curve Modulation and Apex Migration Using Shilla Growth Guidance Rods for Early-onset Scoliosis at 5-Year Follow-up. J Pediatr Orthop. 2019;39(8):400-405.
-
Balioğlu MB, Abul K, Akpolat AO, et al. Implant-Related Complications Do Not Interfere with Corrections with the Shilla Technique in Early Onset Scoliosis: Preliminary Results. Children (Basel). 2023;10(6):947.
-
Murphy RF, Mooney III JF. The Crankshaft Phenomenon. JAAOS. 2017;25(9):e185-93.
-
Hammad AM, Emar M, Shahin F, et al. A Prospective Multicenter ≥2 Years Clinical Study of the Active Apex Correction (APC) Technique in Early Onset Scoliosis (EOS) Patients. Global Spine J. Published online January 24, 2024. doi:10.1177/21925682241229677
-
Agarwal A, Aker L, Ahmad AA. Active Apex Correction (Modified SHILLA Technique) Versus Distraction-Based Growth Rod Fixation: What Do the Correction Parameters Say? Spine Surg Relat Res. 2019;4(1):31-36.
-
Ahmad AA. Early onset scoliosis and current treatment methods. J Clin Orthop Trauma. 2020;11(2):184-190.
-
Ahmad A, Dwaik M, Vo N, et al. Controlling the Apex in Early Onset Scoliosis Through Active Apex Correction (APC) Non Fusion Growth Modulating Technique, Is It a Myth?. Global Spine J. Published online September 29, 2024. doi:10.1177/21925682241289902
-
Alaaeldin Azmi Ahmad, Aakash Agarwal. Active Apex Correction: An overview of the modified SHILLA technique and its clinical efficacy. Journal of Clinical Orthopaedics and Trauma Volume 11, Issue 5, September–October 2020, Pages 848-852
-
Aakash Agarwal, Loai Aker,and Alaaeldin Azmi Ahmad. Active Apex Correction With Guided Growth Technique for Controlling Spinal Deformity in Growing Children: A Modified SHILLA Technique, Global Spine J 2020 Jun;10(4):438-442.
-
Alaaeldin Azmi Ahmad, Minimal invasive surgery techniques for patients with adolescent idiopathic and early onset scoliosis, Journal Of Clinical Orthopaedics and Trauma 2020 Jul 22;11(5):830–838
-
Alaaeldin A. Ahmad, Loai Aker, Yahia Hanbali, et al. Growth modulation and remodeling by means of posterior tethering technique for correction of early-onset scoliosis with thoracolumbar kyphosis. Eur Spine J (2017) 26:1748–1755
You might also be interested in:
Global Spine Journal
AO Spine’s official scientific journal is the first fully open access journal in the field of spine surgery with an impact factor. Read, submit, or apply to become a reviewer.
AO Spine curriculum courses
AO Spine deformity curriculum courses are developed and taught by world-leading experts, based on latest evidence, and provide skills that spine surgeons need for the future.
Global Spine Diploma Program
The first globally developed, ultimate, systematic spine surgery training pathway for recently graduated orthopedic surgeons and neurosurgeons. Stand-alone enrolment offered in deformity.
AO Spine Guest Blog
Highlighting diverse perspectives from the global spine community, sharing knowledge and learnings. Filter by topic to find the most relevant posts for you.