Intraoperative neuromonitoring, a careful balance of risk—and what to do when it goes wrong?
BY DR NICOLAS DEA
There's a lot of literature supporting the use of intraoperative monitoring and many authors actually consider neuro monitoring as a standard of care during spinal surgery. But is it really the standard of care? Why has it become so popular? Does it really improve patient outcomes?
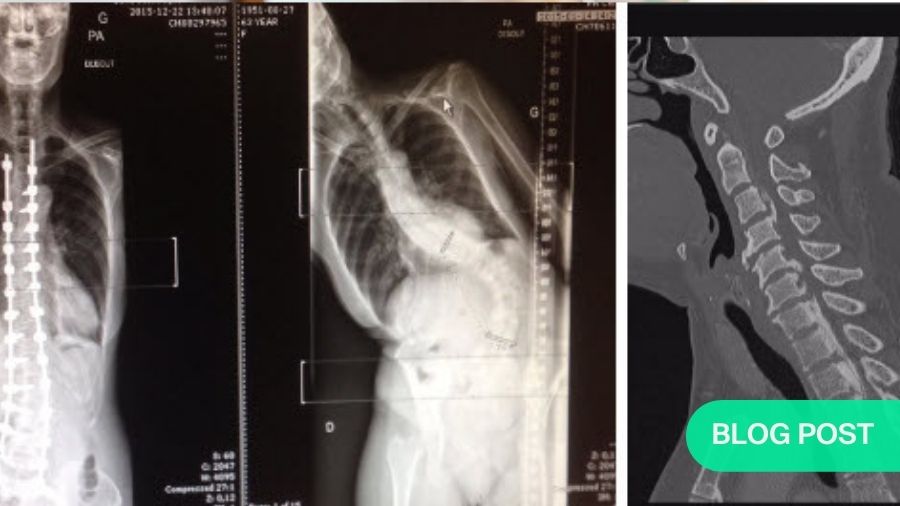
First of all, let’s examine the use of neuro monitoring in deformity surgery, decompression for cervical myelopathy, or surgery for intramedullary tumor. We have many options when we talk about intraoperative neuromonitoring. First and foremost, we have the somatosensory evoked potential, which records the sensory pathway. Second, we have the motor evoked potential, which is direct cortical stimulation and muscle recording in the extremities. We can also do EMGs, either free running or triggered, to monitor the nerve root integrity. Then there’s the D wave option, which is a more refined motor evoked potential recording.
The somatosensory and the motor evoked potential are best suited for intramedullary tumor, extramedullary tumor, intradural tumor, deformity correction, decompression surgery at the cord level. So, anything that is around the spinal cord is good to record the motor evoked in the somatosensory evoked potential.
The free running EMGs are for nerve root integrity. So, for a tumor of the Cauda Equina—any tumor close to nerve roots—we can do triggered EMG when we undertake pedicle screw instrumentation. I personally like using it in degenerative pathology. The D wave is now becoming more and more popular to record the motor evoked potential directly from the spinal cord. So, instead of recording the motor evoked potential from the extremities, we can record them directly from the spinal cord, typically with an individual electrode placed in the epidural space. Even my neurophysiologist likes it when I put it subdurally in the subarachnoid space, directly on the spinal cord. This has been shown to be better for intramedullary tumor specifically, and it's more correlated with postoperative outcome. Even with a complete loss of typical extremity recording MEPs, if the D wave is still preserved, it's usually correlated with deficit on the other side. When there's a complete loss of the D wave, it's unfortunately usually correlated with a permanent neurological deficit.
The problem with false positives
What's the current evidence to use all those modalities? Looking first at its potential to diagnose intraoperative problems, the challenge with the somatosensory and the motor evoked potential is that it is indeed sensible and specific. However, the positive predictive value in most studies is not as great as in the negative predictive value. So, if I'm using the intraoperative neuromonitoring and everything goes well, there's no drop in anything, I'm quite confident that this patient will be fine. However, if there's a significant drop, that doesn’t always correlate to a negative outcome. There's a lot of false positives when we use intraoperative neuromonitoring. The positive predictive value can be as low as 40%.
This raises the definition of how we define ‘meaningful deterioration’. If your neuro physiologist in the room tells you, "Okay, I have a small drop in MEP", what does that mean? There's no strong consensus about what's actually a positive or a significant drop. Most would use an MEP drop of more than 50% or a 10% increase in the latency of the SSPs. Of course, the higher the cutoff, the higher correlation to a real deficit. Because of the high rate of false positive, some would only consider a significant change when there's more than an 80% drop in the MEPs. This is especially the case if we're using a D wave, and we're more confident with that type of recording.
There's a lot of literature summarizing all the published evidence. For example, a 2010 systematic review on the evidence of intraoperative neurophysiology cord monitoring using spine surgery. These papers are not only specific to intradural tumor; they include deformity, decompression surgery, and scoliosis. The sensitivity is quite good at up to 100%, while specificity is a little lower, ranging from 70 to 100. The real problem lies in the positive predictive value. That's what we as surgeons encountered. It can make a surgery even more stressful because the neuro monitoring or the neuro physiologist is telling you, "Doctor we're losing the MEPs." So, it may actually push you towards not achieving your own surgical goal when the change is actually nonsignificant.
Despite this low positive predictive value, a lot of societies have endorsed the use of neuro monitoring during spinal surgery. For instance, the American Academy of Neurology says that the IOM is established as effective and predicts the increased rate of adverse outcome of neurological deficit in spinal surgery as a whole. In 2018, the Congress of Neurological Surgeons acknowledged the high rate of false positives, yet still concluded that the multimodal MEP and SSP is a reliable and valid diagnostic adjunct to assert the integrity of the motor and sensory pathway. By far, we need to include the MEP and also have a combinal multi-modal monitoring, not using only the SSP. From a diagnostic perspective, there's definitely evidence to support that. It’s good to add this as a diagnostic measure, but what really matters is whether it makes our surgery safer.
Let’s look at the evidence that it decreases neurological injury or helps surgeons towards a better tumor resection. This is where it gets less clear. Once again, a lot of literature shows that even when we have multimodal sensory and motor recording with the D wave, it does not result in significant improvement in the rate of a tumor resection. I sometimes ask myself, will it actually make me back off a little bit sooner than I would have done without the neuro monitoring? For these cases, if you have a nice plane of dissection, especially for let's say cervical ependymoma, it's really hard to stop the resection when we feel like everything is going well. I see this as a very useful adjunct when I'm doing some retraction or to give the spinal cord a little bit of a break from manipulation. However, for tumor resection, if I have a nice plane of dissection, I will usually proceed.
What about the extramedullary tumor? Again, while it's a good diagnostic tool and it can predict neurological deficit, there's no global benefit from a neurological perspective or a tumor section perspective. It's a topic that is definitely hot. A lot of people are publishing on this. In the last decade, there's been three systematic reviews of the literature on this topic. The conclusion of all those systematic reviews is that the use of intraoperative neuro monitoring does not result in fewer neurological events and does not result in improved tumor resection. Returning to those guidelines by the Congress of Neurological Surgeons, it shows that while it's a good diagnostic tool, it is not a good therapeutic tool. It does not improve tumor resection or neurological outcome.
Intraoperative decision making
Despite all of this, many surgeons use this modality very frequently. Even if it's not evidence based to show improved neurological outcome, I personally use it very routinely for intradural tumor, intramedullary tumor and certain cases of deformity correction, extradural resection (when I anticipate some cord manipulation) or when I close an osteotomy. So, we need to know what happens if it goes wrong. What if your neuro physiologist comes to you and says, "Doctor, I'm losing MEPs, I'm losing SSPs”?
Is there any algorithm we can use to decrease the risk of neurological injury? There are some surgical reactions to consider here. Am I retracting too much? I will tell my assistant, relax the cord, relax the retraction. Did I just close the osteotomy? Did I just over distract the spinal cord to deliver a tumor on a lab liposuction? Sometimes, even just the position of the patient can deliver a false positive, and simply raising the position of the patient can cause a peripheral nerve compression or an unstable spine. The neurophysiology team will usually do baseline assessment prior to surgery, and then another set when the patient is under GE, and we can use those baselines to see if there's any deterioration. If I'm putting screws and I lose some motors, is that related to my screw placement? You need to consider whether to use triggered EMG, intraoperative CT scan to confirm the misplacement, or whether to just go ahead with the decompression and move on with your case.
What can be done from a physiological perspective? Often, the first thing I will do when I have a drop in the neuro monitoring, is to pause and talk with my anesthetist. We will make sure that the patient is warm and that the perfusion pressure is good, especially if I'm in at cord level. I'm quite picky with this. For an MEP above 80 to 85, I will irrigate, see what's happening, make sure that it's not technical. If I'm doing a thoracic tumor, I will check for a global drop in the upper and lower extremities. If it's real, and despite all of these checks, I still have a drop in my MEPs, this is where the intraoperative judgment is very important. Do I actually think that I've done something wrong? Do I believe that there's anything to be done to decrease the risk of neurological injury to that patient?
The toughest decision is when I have a significant drop in the MEPs, let's say 60–70%, when there's a nice plane with the tumor and everything seems to be going well. I often have that discussion with the patient ahead of time. We discuss whether in these circumstances I should stop the resection to decrease the neurological risk. Those are all very tough intraoperative decisions to make, depending on the scenario. There's no evidence as to what the best remedial measure is—it's a complex process.
***
The title of intraoperative neuromonitoring is also covered in a lecture series by the AO Spine Knowledge Forum Tumor. A selection of the lectures is published open access in the AO Spine Clinical Library. More recorded lectures and videos available in the AO Video Hub.
About the author
Dr Nicolas Dea is a Clinical Associate Professor of Neurosurgery at the University of British Columbia. He completed his MD program and his neurosurgical training in Sherbrooke, Quebec, and his spine surgery fellowship in Vancouver, BC. Dr. Dea completed his Masters in Health Economics, Policy and Management at the London School of Economics & Political Sciences in London, UK. He is the Vice-Chair of the Neurosurgery Examination Committee at the Royal College of Physicians & Surgeons of Canada, playing an active role in the examination of neurosurgical candidates. He is an associate member of the AO Spine Knowledge Forum Tumor, an international multi-disciplinary panel of experts pursuing innovative research into spine oncology and is the co-PI of an international study dedicated to the primary tumors of the spine. He also sits on the executive board of the Canadian Spine Society, is a Steering Committee member of the Canadian Spine Outcomes and Research Network and is the Principle investigator of the Canadian Prospective Cervical Spondylotic Myelopathy study.
Disclaimer
The articles included in the AO Spine Blog represent the opinion of individual authors exclusively and not necessarily the opinion of AO Spine or AO Foundation.


