The ECO Health Project: towards personalized and precision spine care
BY DR ASDRUBAL FALAVIGNA

Health science is moving from generalization to personalization of information. Precision and accuracy are the words that will change the future of spine care. Transformation is something expected and necessary for survival.
Mobile technology is transforming healthcare, allowing the rise of telemedicine and its incorporation into day-to-day medical practice as well as into research scenarios. One promising field of telemedicine is remote patient monitoring, which has been studied in recent years across a multitude of medical specialties, with positive results.
Health technology assessment collects data focusing on the medical, economic, social, and ethical implications to inform real-world decisions about the value of new technologies, interventions, and practices.
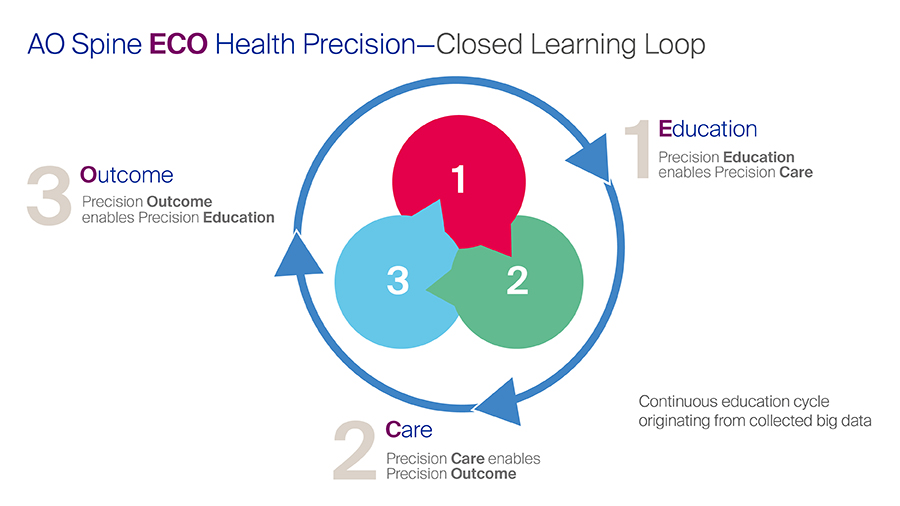
My strategy in life is grounded in performing a personalization of needs and implementing innovation in education, research, and delivery of care. Therefore, it is essential to discuss the importance of Health Precision in Education, Care, and Outcome (ECO Health Precision). The learning loop for surgeons starts with Education that influences care, promotes a change in the outcome, and ultimately endorses new education or consolidates the previous information. Thus, it is a continuous education cycle that uses the big data collected for learning.
Besides the fundamental importance for learning, ECO Health Precision is a strategic value proposition for a patient and surgeon centered organization.
In the next paragraphs I will explain each of the three pillars of ECO Health Precision.
- Precision Education: Precision education is where the spine surgeon gets the knowledge and skills that fill his or her training gap. The goal is to provide the personalization of the surgeons' needs, such as learning and training activities at fingertip. The products that AO Spine must enable this are myAO and the mentoring program. For precision education, it is necessary to create an integrated library that provides smart search and smart recommendations of the following courses according to the surgeon's profile and needs. This can become even better with a chance of greater integration and to enhance the network between the regions and the AO community.
- Precision Care: Strengthening the network between patients and doctors enables us to apply preventive strategies for specific spine pathologies and complications. Numerous trials have demonstrated the effectiveness of telemonitoring for habit changing as in weight loss, adoption of healthy dietary habits and smoke cessation, as well as adherence to treatment and positive cost-benefit outcome 1-11. In this sense, it is reasonable to add remote monitoring in our practice to track the patient's clinical situation live, during the perioperative period. The most important aspect is the patient's multidisciplinary tele-education and telemonitoring care that has opened a communication portal with the patient because many of the most troublesome problems in health care come down to lack of communication. It empowers patients by supplying them with multi-professional information, enabling them to better understand their condition or treatment, and to engage more fully with their care. The purpose is to share point-of-care medical data and information captured in patient portals to the remote platform, while adhering to strict security standards for health information. Besides that, it proved to be an extremely valuable research tool. It is my goal to make available a worldwide platform to remotely deliver care and obtain metrics from the patient about the effectiveness of the treatments.
- Precision Outcome: We need to measure the influence of the educational activities in AO Spine on the wellbeing of the patients. The changes necessary to improve our effectiveness come from surgeon and patient data. The use of clinical registries based on PROMs adds strategic value to medical care by narrowing the gap between the clinician’s and patient’s view of the clinical reality, and also helps tailor the treatment plans for specific needs. The integration among PROMs systems and Electronic Health Records is a relevant topic because it facilitates communication, improves care delivery, and leverages the use of artificial intelligence algorithms. Electronic databases need to be easier and user friendly to both physicians and patients, and actively deliver PROM questionnaires to the patients and engage by themselves according to a pre-established timeline.
Digital transformation bridges the gaps in education, research and health care and keeps them open to the future. The world is changing so fast that it is essential to plan and immediately reframe our actions for the next five, ten, and twenty years with confidence and clarity of our goals.
We need to be inclusive by involving present, past, and future generations by providing them with a platform for growth and development in spine surgery, having synergy by being creative and having cooperation in the global spine community. We have the opportunity to roll out this innovative project, making doctor-patient communication easier and improving the effectiveness of health care.
About the author
References and further reading:
- Haas K, Hayoz S, Maurer-Wiesner S. Effectiveness and Feasibility of a Remote Lifestyle Intervention by Dietitians for Overweight and Obese Adults: Pilot Study. JMIR mHealth and uHealth. 2019;7(4):e12289.
- Hansel B, Giral P, Gambotti L, et al. A Fully Automated Web-Based Program Improves Lifestyle Habits and HbA1c in Patients With Type 2 Diabetes and Abdominal Obesity: Randomized Trial of Patient E-Coaching Nutritional Support (The ANODE Study). Journal of medical Internet research. 2017;19(11):e360.
- Dunn C, Olabode-Dada O, Whetstone L, et al. Using synchronous distance education to deliver a weight loss intervention: A randomized trial. Obesity. 2016;24(1):44-50.
- Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity. 2013;21(9):1789-1797.
- Abroms LC, Boal AL, Simmens SJ, Mendel JA, Windsor RA. A randomized trial of Text2Quit: a text messaging program for smoking cessation. American journal of preventive medicine. 2014;47(3):242-250.
- Nomura A, Tanigawa T, Muto T, et al. Clinical Efficacy of Telemedicine Compared to Face-to-Face Clinic Visits for Smoking Cessation: Multicenter Open-Label Randomized Controlled Noninferiority Trial. Journal of medical Internet research. 2019;21(4):e13520.
- Gandhi S, Chen S, Hong L, et al. Effect of Mobile Health Interventions on the Secondary Prevention of Cardiovascular Disease: Systematic Review and Meta-analysis. The Canadian journal of cardiology. 2017;33(2):219-231.
- Kim JY, Wineinger NE, Steinhubl SR. The Influence of Wireless Self-Monitoring Program on the Relationship Between Patient Activation and Health Behaviors, Medication Adherence, and Blood Pressure Levels in Hypertensive Patients: A Substudy of a Randomized Controlled Trial. Journal of medical Internet research. 2016;18(6):e116.
- Bobrow K, Farmer AJ, Springer D, et al. Mobile Phone Text Messages to Support Treatment Adherence in Adults With High Blood Pressure (SMS-Text Adherence Support [StAR]): A Single-Blind, Randomized Trial. Circulation. 2016;133(6):592-600.
- Lu K, Marino NE, Russell D, et al. Use of Short Message Service and Smartphone Applications in the Management of Surgical Patients: A Systematic Review. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2018;24(6):406-414.
- Farias FAC, Dagostini CM, Bicca YA, Falavigna VF, Falavigna A. Remote Patient Monitoring: A Systematic Review. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2019.
Disclaimer
The articles included in the AO Spine Blog represent the opinion of individual authors exclusively and not necessarily the opinion of AO Spine or AO Foundation.