Why navigation and robotics are not the standard for all spine surgery—lessons learned
BY DR STEFAN MOTOV AND PROF MARTIN N. STIENEN
The integration of navigation and robotics into spinal surgery represents a significant advancement in medical technology, aiming to enhance surgical precision, reduce complications, and improve patient outcomes. The planning and execution tools of navigation and robotic systems are particularly useful for educational purposes, as demonstrated in the AO spine curriculum and MIS cases (Patel et al., 2023) or cases with challenging anatomy, as in complex deformity and revision cases (Haider et al., 2023). Several additional benefits of both tools have been described by their users. However, the acquisition costs and limited current applications of particularly robotics, mainly restricted to implant insertion and planning, might be a significant hurdle to their implementation.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
We developed a comprehensive AO spine survey (Motov et al., 2025) to provide insights into the current adoption trends, perceived benefits, and barriers associated with spinal navigation and robotics. The questionnaire has been designed with the Survey Monkey platform and distributed from October 25th to November 13th, 2023, to the AO spine members. The survey garnered 424 responses, reflecting the app. 9.9% response rate. Most participants were board-certified orthopedic surgeons (46%) and neurosurgeons (32%), with representation from various continents and primarily affiliated with university hospitals (49.5%) or private hospitals/practices (28.5%).
Where are navigation and robotics used
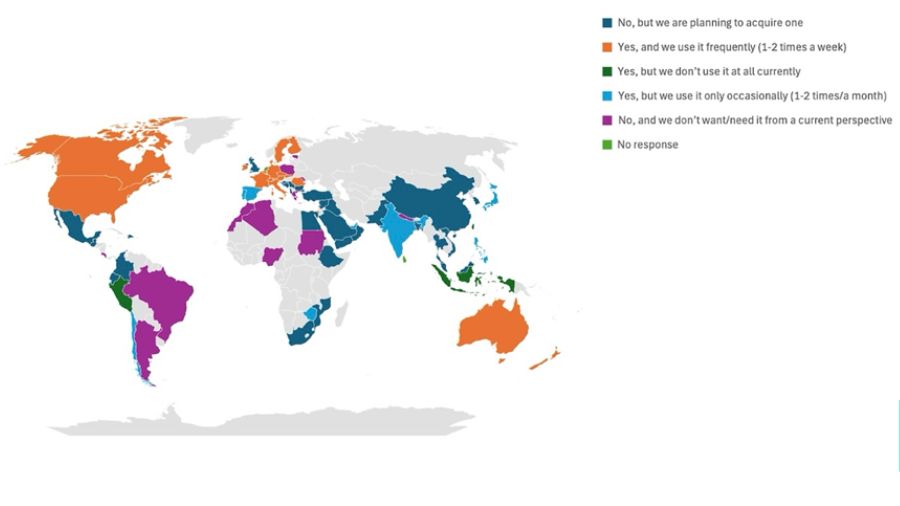
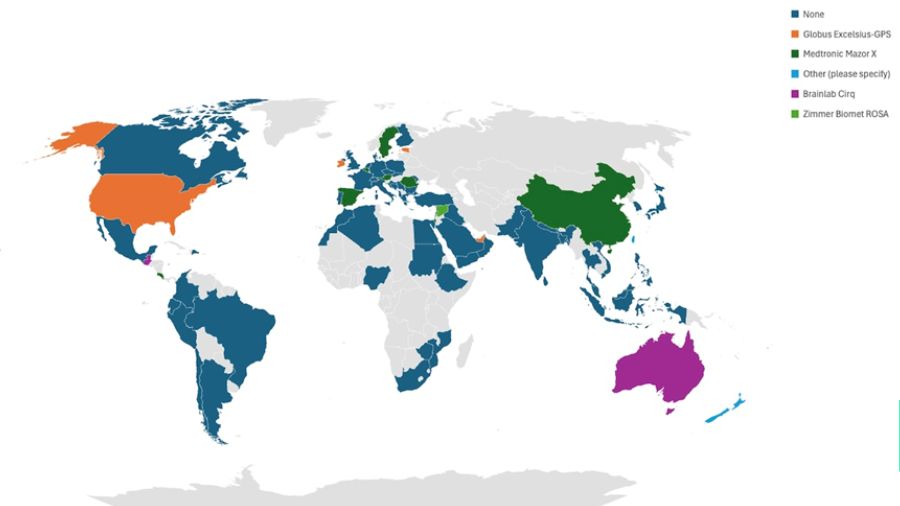
The survey revealed that nearly half (49%) of participants reported occasional or frequent use of navigation assistance during spinal instrumentation procedures (Figure 1). In contrast, only 18% indicated the use of robotic assistance. A significant difference was observed based on the country's median income status and the respondent's number of annual instrumentation procedures. Specifically, surgeons from higher-income countries and those performing a greater number of instrumentation procedures were more likely to utilize robotic assistance (Figure 2).
Barriers to implementation of robotics
High acquisition costs were identified as the primary barrier to the implementation of robotics, cited by 77% of participants. Other notable barriers included the perceived insufficient benefit of spinal robots (28%) and the belief that existing spinal navigation systems already provide adequate precision (20%).
Perceived benefits and limitations of robotic assisted systems
Among spine surgeons who have adopted robotic assistance, 69% believe that robots increase precision during instrumentation procedures, and 72% consider them useful tools. However, there was no clear consensus regarding the reduction of intraoperative complications (54%) or an increase in surgical efficiency (43%).
Future perspectives for innovations and investments
Looking ahead, 35% of participants plan to acquire a robotic system in the future, while 36% stated they do not currently see the need for one. The survey also highlighted a desire for future innovations, with 70% of respondents expressing interest in more integrated surgical options and 55% in the integration of artificial intelligence. Additionally, 43% of surgeons indicated they would consider a shared company investment with guaranteed use of implants or other products by the hospital as a viable option to acquire a robotic system.
Despite the growing interest in robotics within spine surgery, these systems are not yet standard equipment for many surgeons, primarily due to high acquisition costs and limited perceived usability. Further developments and innovations are necessary to justify broader utilization and to overcome existing barriers. This survey provides a comprehensive overview of the current state and future perspectives of spinal navigation and robotics, offering valuable insights for surgeons, healthcare institutions, and policymakers aiming to navigate the evolving landscape of spine surgery.
Navigation and robotics offer advantages in limited scenarios
Our study (Motov et al., 2025) reflects very much the differences in standard equipment in spine surgery among the different AO regions and presents a review of the current state of adoption of spinal navigation and robotics. Continuous innovation and synergy of robotics with e.g. augmented or mixed reality and artificial intelligence, might provide a more cutting-edge technology demanded for a higher adoption rate. It appears for now that robotics are not providing a significant benefit over spinal navigation for many spine surgeons, and therefore, they are less willing to utilize them. Specifically, in lower and middle-income countries, it matters most what kind of innovation devices are acquired, and the financial turnover is paramount for their implementation.
Despite the growing popularity of spinal robotic systems, real-world data demonstrated similar radiation exposure and complication rates compared to navigated and freehand techniques (Tarawneh et al., 2021), (Keric et al., 2017), (Huang et al., 2020), (Staartjes et al., 2018). Unless robotics might enable higher efficiency with lower complication rates and reduce expenditure for care providers, they appear to be very expensive gadgets from the current perspective, especially in these geographical areas. Interestingly, a significant number of participants in the survey who stated their department already possesses a robot indicated they use it only occasionally (1-2 times a month) or don’t use it at all, which further emphasizes the limited benefits robotic systems provide at the current stage.
Spinal navigation, on the other hand, seems to have been broadly adapted and utilized by all specialties. Naturally, more surgeons from high-income countries with higher numbers of annual instrumentation procedures are more prone to use navigation as they are presumably able to afford the acquisition costs and are eager to avoid medicolegal issues with suboptimal placement of implants. Financial plans with the possibility of multiple shareholders or funding through implant usage for both tools are of high importance to enable a higher distribution around the globe.
In our practice, we experienced several advantages of both spinal navigation and spinal robotics during fellowships and residency. However, we see the advantages of both tools in limited scenarios, e.g., cervical pedicle screws, deformity and revision cases with distorted anatomy, percutaneous screw insertion, and prone or lateral one-stop shop procedures. In standard degenerative, tumor, or infection cases with open approaches, the need for navigation or robotic use might be debatable. With a reliable OR workflow in open procedures, one might be even quicker with freehand techniques and achieve similar results. Safety, screw placement accuracy, and reduction of X-ray exposure to the OR-Team appear to be strong arguments for navigation and robotics.
Nevertheless, both devices require funding, designated educational courses for the OR personnel, constant workflow, and disposals, which are associated with a negative ecological footprint. Even though the trend in spine surgery is clearly toward the implementation of these tools and it is a matter of time until legal issues become omnipresent for everybody not using this type of technology as intraoperative errors such as malpositioned implants are one of the most common alleged malpractice in the US courts (Sankey et al., 2020; Zhang et al., 2022). For us, it is still smarter to use it regularly but not to rely entirely on it, as in straightforward cases, the benefits are not pronounced, and one should always be prepared for the times when technology fails or misguides us.
About the authors:
Dr Stefan Motov is a neurosurgeon specialized in spine surgery. He completed his neurosurgical residency at the Technical University Munich in 2020 and is currently working in the joint neurosurgery/orthopedics center in Kantonsspital St Gallen, Switzerland, focusing on endoscopic, oncological, MIS spine surgery, and interventional pain medicine. Motov is part of the EANS Young Neurosurgeons Committee and the DWG Junges Forum, where he is involved in educational activities for neurosurgery and spine surgery residents in Europe and Germany. He also recently launched a German podcast with his colleague Dr Sami Ridwan on controversies in spine surgery (SpineDocs).
Dr Motov is a member of multiple societies, including the German (DWG) & Swiss Society of Spinal Surgery (SGS), EANS, and AO Spine, where he is involved in educational programs and multiple research collaboration projects.
Prof Dr Martin N. Stienen trained in St.Gallen, Geneva, and Zurich to obtain his board-certification in neurosurgery, followed by fellowship trainings in the US (Stanford University) and Korea (Gangnam Severance University Hospital). He is co-chair of the interdisciplinary spine center at Health Ostschweiz (H-OCH), formerly Kantonsspital St.Gallen, where he supervises a team of 20 physicians and treats a broad variety of spinal pathologies ranging from minimally invasive/endoscopic procedures for degenerative to adult spinal deformity and vertebral column/spinal cord tumors.
Prof Stienen is active in several professional societies, including the AO Spine (past Neuro-Officer Switzerland), EANS Spine Section, German (DWG) & Swiss Society of Spinal Surgery and runs the spinal research lab in St.Gallen, frequently collaborating on multi-center studies with other globally leading institutions.
References and further reading:
- Haider, G., Shah, V., Johnstone, T., Maldaner, N., Stienen, M., & Veeravagu, A. (2023). Accuracy of predicted postoperative segmental lumbar lordosis in spinal fusion using an intraoperative robotic planning and guidance system. J Neurosurg Sci. https://doi.org/10.23736/S0390-5616.23.06142-8
- Huang, J., Li, Y., & Huang, L. (2020). Spine surgical robotics: review of the current application and disadvantages for future perspectives. J Robot Surg, 14(1), 11-16. https://doi.org/10.1007/s11701-019-00983-6
- Keric, N., Doenitz, C., Haj, A., Rachwal-Czyzewicz, I., Renovanz, M., Wesp, D. M. A., Boor, S., Conrad, J., Brawanski, A., Giese, A., & Kantelhardt, S. R. (2017). Evaluation of robot-guided minimally invasive implantation of 2067 pedicle screws. Neurosurg Focus, 42(5), E11. https://doi.org/10.3171/2017.2.FOCUS16552
- Motov, S., Butenschoen, V. M., Krauss, P. E., Veeravagu, A., Yoo, K. H., Stengel, F. C., Hejrati, N., & Stienen, M. N. (2025). Current state and future perspectives of spinal navigation and robotics-an AO spine survey. Brain Spine, 5, 104165. https://doi.org/10.1016/j.bas.2024.104165
- Patel, N. A., Kuo, C. C., Pennington, Z., Brown, N. J., Gendreau, J., Singh, R., Shahrestani, S., Boyett, C., Diaz-Aguilar, L. D., & Pham, M. H. (2023). Robot-assisted percutaneous pedicle screw placement accuracy compared with alternative guidance in lateral single-position surgery: a systematic review and meta-analysis. J Neurosurg Spine, 39(4), 443-451. https://doi.org/10.3171/2023.3.SPINE2329
- Sankey, E. W., Mehta, V. A., Wang, T. Y., Than, T. T., Goodwin, C. R., Karikari, I. O., Shaffrey, C. I., Abd-El-Barr, M. M., & Than, K. D. (2020). The medicolegal impact of misplaced pedicle and lateral mass screws on spine surgery in the United States. Neurosurg Focus, 49(5), E20. https://doi.org/10.3171/2020.8.FOCUS20600
- Staartjes, V. E., Klukowska, A. M., & Schroder, M. L. (2018). Pedicle Screw Revision in Robot-Guided, Navigated, and Freehand Thoracolumbar Instrumentation: A Systematic Review and Meta-Analysis. World Neurosurg, 116, 433-443 e438. https://doi.org/10.1016/j.wneu.2018.05.159
- Tarawneh, A. M., Haleem, S., D'Aquino, D., & Quraishi, N. (2021). The comparative accuracy and safety of fluoroscopic and navigation-based techniques in cervical pedicle screw fixation: systematic review and meta-analysis. J Neurosurg Spine, 1-8. https://doi.org/10.3171/2020.11.SPINE201877
- Zhang, J. K., Del Valle, A. J., Alexopoulos, G., Patel, N., Van Nispen, J., Patel, M., Xu, E., Mercier, P., Kohn, N. A., & Mattei, T. A. (2022). Malpractice litigation in elective lumbar spinal fusion: a comprehensive review of reported legal claims in the U.S. in the past 50 years. Spine J, 22(8), 1254-1264. https://doi.org/10.1016/j.spinee.2022.03.015
You might also be interested in:
Global Spine Journal
Read open access, submit your research, or become a reviewer for AO Spine’s official scientific journal.
AO Spine fellowships
Providing additional experience in surgical techniques for fully trained orthopedic and neurosurgeons interested in spine surgery.
AO Spine courses
Where will you go next? Explore all upcoming courses and event in your region and worldwide.
AO Spine newsletters
Never miss a beat! Sign up for the AO Spine newsletter to see the latest news, open calls, guest articles, and more.