How good is trans-Kambin TLIF with a large-footprint interbody compared to ALIF?
BY DR CHRISTIAN MORGENSTERN
At the beginning and during its initial stages of development in the 1980s, 1990s and 2000s, the adoption of endoscopic spine surgery was slow and limited to a few early-adopters and pioneers. Yet, in the last decade, endoscopic spine surgery has experienced an exponential rise in popularity and adoption all over the world by both orthopedic and neurologic surgeons. This is mostly due to improving instrumentation and increased availability of educational opportunities, as well as an ever-broadening scope of indications. Furthermore, an increasing number of high-quality randomized control trials [1] have finally provided solid evidence for the long-anticipated superior cost-effectiveness and non-inferior clinical outcome of spinal endoscopic procedures.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Endoscopic trans-Kambin TLIF and current limitations
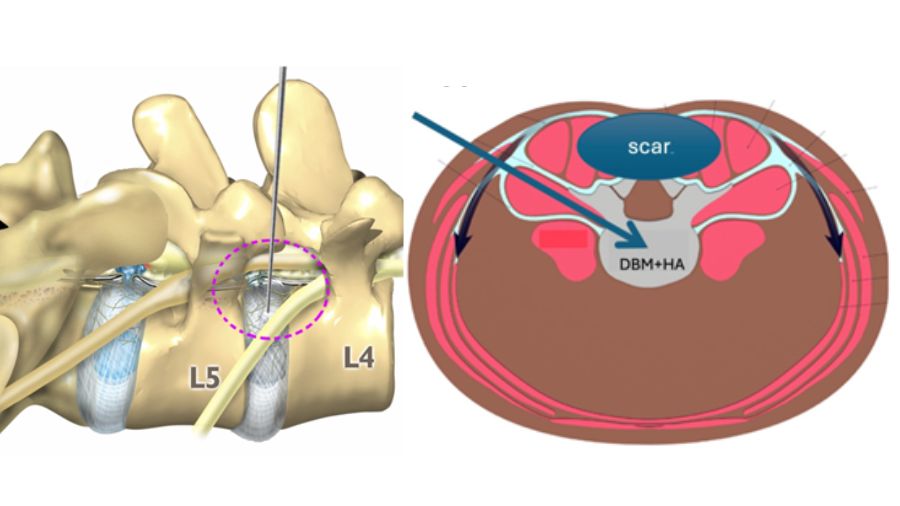
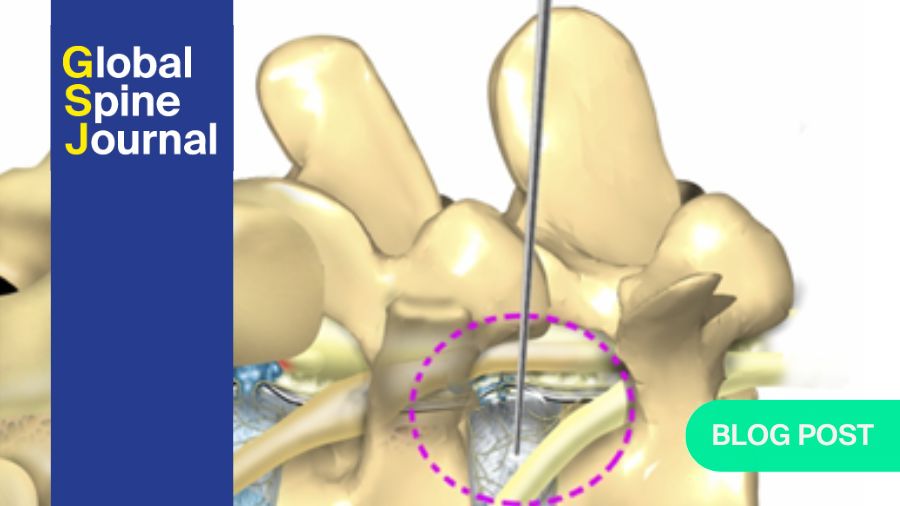
Full-endoscopic/percutaneous transforaminal lumbar interbody fusion (TLIF) surgery has been one of the latest indications to be added to the endoscopic spine surgery portfolio. In this technique, a uniportal, extra-foraminal approach using Kambin’s triangle allows safely bypassing the exiting nerve root and inserting an interbody cage into the lumbar disk (trans-Kambin approach) [2–4], see figure 1.
Advantages of trans-Kambin TLIF comprise minimal soft tissue disruption using sequential dilators (no dissection necessary), a facet-sparing approach with limited bone resection, minimal intra- and post-operative bleeding, minimal risk of infection, early and opioid-free post-operative ambulation and hospital discharge, as well as direct decompression of the neuroforamen with foraminoplasty and a postero-lateral approach that allows bypassing posterior scar tissue in revision surgeries.
However, we identified three important limitations of present trans-Kambin TLIF techniques that are currently hindering a wide-spread acceptance:
- First, endoscopic visualization is mandatory for most trans-Kambin fusion systems, which implies investment in expensive endoscopic equipment and instrumentation, as well as overcoming the steep learning curve of endoscopic spine surgery [4].
- Second, most full-endoscopic trans-Kambin systems use a tubular sleeve for endoscopic disk access and endplate preparation. The tubular sleeve’s and/or the endoscope’s working channel diameter is usually small (less than 12mm), representing a main constraint to the size of an interbody cage that can be placed through that tube. Therefore, expensive, small-footprint interbody cages with an intricate expansion mechanism for interbody fusion are employed in most full-endoscopic fusion systems.
- Third, also the size of the disk preparation instruments is usually small as they must fit through a small endoscopic working channel. Small disk preparation instruments are expensive and frail, and it takes more surgical time with small instruments to complete a disk preparation at costs of surgical efficiency.
Moreover, even though an increasing number of studies are being published on trans-Kambin TLIF, questions remain about its capability to restore lumbar lordosis, perform a good disk preparation, transitory post-operative radiculitis and placing large-footprint interbody cages, in comparison to other established lumbar fusion techniques.
Figure 1.
a) anatomic schematics of Kambin’s triangle that allows an extra-foraminal approach to the disk and canal bypassing the exiting nerve root.
b) anatomic axial view of the lumbar spine showing the usual postero-lateral trajectory of a trans-Kambin approach that would allow bypassing the posterior scar tissue in a revision surgery.
Novel technical developments to overcome limitations of trans-Kambin TLIF
We aimed to address the mentioned limitations of trans-Kambin TLIF by developing a completely new and specialized percutaneous trans-Kambin TLIF system with a novel dilator [2, 3], that incorporates a universal delivery sheath (see figure 3 in the GSJ article) This delivery sheath allows protecting the exiting nerve root in Kambin’s triangle during foraminoplasty, disk preparation and cage insertion, while its non-tubular shape allows a diameter-independent insertion of instruments and a large-footprint lumbar interbody cage. [3] With this new system, endoscopic visualization is not required anymore to perform a full-percutaneous TLIF, which should make this technique accessible to surgeons without previous endoscopic experience. The surgical steps of this procedure are reproducible, while the handling of the fluoroscope feels familiar to percutaneous transpedicular screw insertion [3]. Hence, the learning curve for this full-percutaneous TLIF should be shorter than for a standard endoscopic TLIF.
Furthermore, this full-percutaneous TLIF surgery allows a time-efficient interbody cage placement in less than 30 minutes per level [2, 3] and should be more cost-efficient, as standard interbody cages and regular instruments for disk and endplate preparation can be used (no need for expensive specialized interbody cages and endoscopic instruments).
Furthermore, we developed these instruments to facilitate placing a large-footprint interbody cage using the trans-Kambin approach [2, 3].
This was challenging, given the anatomic constraints of Kambin’s triangle, which have led current endoscopic TLIF systems to use small, expandable interbody cages specially designed to fit through an endoscopic tube and/or working channel. These specialized cages usually have a complex, centrally placed expansion mechanism that is expensive and impedes bone growth through the cage, while they usually do not provide a great range of lordosis.
In contrast, large-footprint interbody cages usually have a big window for bone graft and a high bone/cage surface contact area, hence decreasing the risk for subsidence and increasing the rate of intervertebral bone fusion (see figure 1 in GSJ). Therefore, it was our aim to translate the advantages of a large-footprint interbody cage to trans-Kambin fusion. In fact, the TLIF cage we ended up choosing to test the capabilities of our trans-Kambin TLIF system, has a footprint of 39x12mm (surface 468mm2), which represents a 1.5 to two-fold increase in surface compared to most regular-sized MIS TLIF and endoscopic TLIF cages [2, 3], and probably has one of the largest graft windows currently available for a TLIF cage.
How do ALIF and endoscopic/percutaneous TLIF compare
We all know how good Anterior Lumbar Interbody Fusion (ALIF) surgery is for lumbar interbody fusion. Why ALIF? ALIF is probably the most powerful technique for lumbar spine fusion, especially for L5/S1, as it allows placing a very large, hyperlordotic interbody cage and considerably restoring segmental lumbar lordosis.
But can endoscopic/percutaneous TLIF keep up with it? How good is our novel percutaneous TLIF (pTLIF) system really? This is a question I asked myself and many colleagues have been critically asking me. In order to be able to answer that, I reckoned that the only way to find out was to design a study directly comparing endoscopic/percutaneous TLIF (pTLIF) against ALIF.
We are delighted that our results have recently been published in AO Spine‘s Global Spine Journal [2, 3]. Summarizing the outcome of our comparative study [2]:
- Study design: exploratory prospective observational case-control study. 87 patients in total with 44 patients in the ALIF group and 43 with pTLIF.
- Clinical outcome was comparable for both techniques after 2.5 years post-operative follow-up.
- Bone fusion rate (assessed by CT scan and standing X-ray films at 1 year F/U) showed no significant differences between ALIF (97%) and pTLIF (91%)
- Radiologically, ALIF excelled with a post-operative increase in segmental lordosis of 7.8 degrees, doubling the 3.7 degrees we were able to achieve with pTLIF.
- We were significantly faster placing a cage with pTLIF (< 30 minutes), that's half the time that we needed for ALIF (approx. 1 hour surgery time).
- ALIF presented more intra-operative complications, while pTLIF presented more complications in the post-operative follow-up (cage subsidence and revision surgery).
Lessons taken for my clinical practice
So, how does all of this translate into my clinical practice? ALIF is a very powerful technique, but not every case is suited for an ALIF: i.e. patients with a (very) high BMI and/or a history of previous abdominal surgery/-ies and/or abdominal vascular pathologies, etc. should probably not opt for an elective ALIF procedure, unless you have an access surgeon with a lot of experience (I do all anterior approaches myself) and warn the patient of potentially severe approach-related complications. Probably, I would still choose ALIF over (percutaneous) TLIF for cases for which I need to maximize post-operative segmental lordosis, like in deformity cases.
In my opinion, pTLIF has proven itself in our studies [2, 3] with excellent results, especially considering that it is now possible to place a large-footprint interbody cage in less than 30 minutes surgery time using the trans-Kambin approach. pTLIF can be an excellent choice for patients that are not eligible for ALIF and i.e. have a high BMI and/or a history of previous lumbar surgeries, etc.
In conclusion, I will keep using both techniques selectively in my practice after carefully assessing each case's specificities.
About the author:
Dr Dr med. Dipl-Ing. Christian Morgenstern is an Orthopedic surgeon from Barcelona and currently serves as head of the Morgenstern Institute of Spine at the Centro Médico Teknon in Barcelona, Spain. He obtained his board certification in orthopedic surgery form the German Board in Berlin after completing his residency at the Charité University hospital in Berlin and fellowships in minimally invasive and endoscopic spine surgery in Barcelona and Korea. Between 2020 and 2024 he was the head of the spine department of the public health system (SAAS) in Andorra.
Morgenstern possesses a sound technical background with a Ph.D. in biomedical engineering from UPC-BarcelonaTECH (Spain), a Dipl.-Ing. in Electrical Engineering by the Karlsruhe Institute of Technology (Germany) and wrote his graduation thesis as a visiting student at the Massachusetts Institute of Technology (MIT) in Cambridge, MA, USA. His interests lie in minimally invasive and endoscopic spine surgery and identifying and finding technical and surgical solutions to current challenges in spine surgery in cooperation with the medical industry.
Morgenstern has presented and published more than 100 abstracts and papers in international peer-reviewed journals and conferences, holds several international patents, has been an international faculty for endoscopic spine surgery at the AO Davos Courses (Switzerland), has been appointed a honorary vanguard member of the international Spinal Endoscopy Research Foundation (iSERF), USA, has been appointed the ISMISS national representative for Spain, and is a member of several international societies (AO Spine, NASS, ISMISS, ISASS, Eurospine and IEEE).
References and further reading:
- Gadjradj PS, Rubinstein SM, Peul WC, et al. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. BMJ. 2022; 21;376:e065846.
- Morgenstern C, Nogueras F, Delbos G, Morgenstern R, Anterior Lumbar Interbody Fusion (ALIF) versus Full-Endoscopic/Percutaneous TLIF with a Large-Footprint Interbody Cage: A Comparative Observational Study, Global Spine J 2025; OnlineFirst, DOI: 10.1177/21925682251316280
- Morgenstern C, Morgenstern R, Full-Percutaneous trans-Kambin Lumbar Interbody Fusion with a Large-Footprint Interbody Cage, Global Spine J 2025; OnlineFirst
- Morgenstern R, Morgenstern C, Yeung AT, The learning curve in foraminal endoscopic discectomy: experience needed to achieve a 90% success rate. SAS J 2007;1:100-107.
You might also be interested in:
Global Spine Journal
AO Spine’s official scientific journal. Read open access, submit your manuscript, become a reviewer.
AO Surgery Reference
A powerful online resource for the management of a vast variety of fractures.
AO Spine Knowledge Forum Degenerative
Helping surgeons to make the best choice—increasing awareness of evidence.
AO Spine Guest Blog
Insights form the AO Spine community, current hot topics, and controversies in spine care.