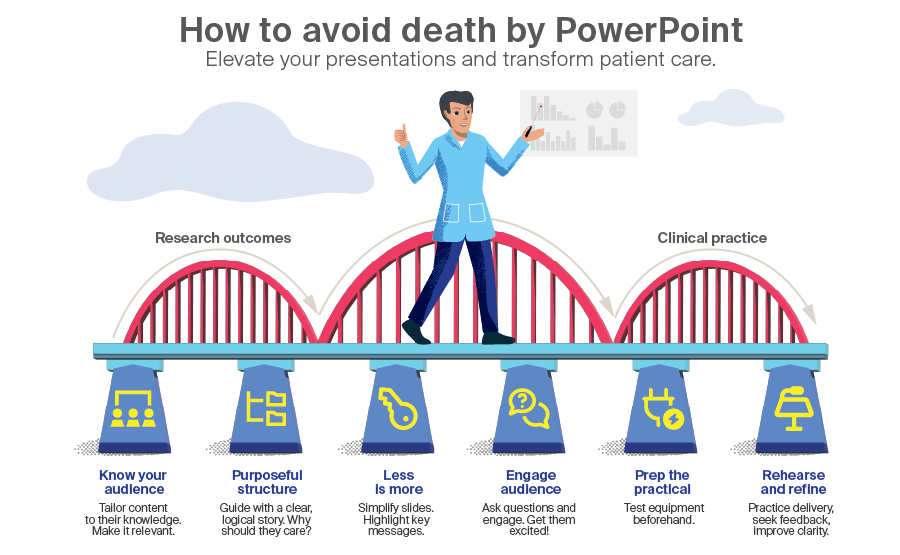
From data to decisions: How to avoid death by PowerPoint and accelerate clinical adoption of your study outcomes.
BY DRS MIKE YY LEUNG AND MOHAMED HAZEM ABDELAZEEM

Whether you’re a veteran academic or a resident eager to make your mark, delivering a strong research presentation is a skill that can elevate both your career and our field. In this blog, we want to offer some practical tips for crafting and delivering presentations that stand out.
As cranio-maxillofacial (CMF) surgeons, we routinely engage in research to advance our field and improve patient outcomes. Sharing these findings with peers, whether at conferences, departmental meetings, or in academic forums, is a key part of our role as clinician-scientists. Yet, the ability to present research clearly and effectively is sometimes undervalued in surgical training. This skill is not just a matter of personal development—it can help contribute to the progress of CMF surgery as a discipline.
-
Read the quick summary:
- Drs Mike Leung and Mohamed AbdelAzeem explain how surgeons can make research presentations clear, structured, and engaging for any audience.
- Effective presentations increase understanding, boost professional reputation, and help new techniques and findings get adopted in clinical practice.
- Surgeons should tailor content to their audience, use simple visuals, practice delivery, and prepare for technical issues to maximize impact.
- Mastering these skills accelerates translation of research into patient care, with ongoing opportunities to refine communication and share best practices.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Why do presentation skills matter for CMF research?
Presenting your research at congresses and events is an important practical tool for knowledge translation—to speed up the adoption of your findings in clinical practice and to boost your citations. It is a practical tool for disseminating new knowledge, fostering collaboration, and encouraging critical discussion. Well-structured presentations help ensure that our work is understood, evaluated, and, where appropriate, implemented by colleagues. They also play a role in building professional reputation and facilitating academic advancement.
In our field, where complex surgical techniques and nuanced clinical outcomes are common, clear communication is essential. An effective presentation can clarify methodology, highlight the significance of findings, and make technical details accessible to a wider audience. Conversely, poorly presented research may lead to misinterpretation, missed opportunities for feedback, or limited uptake of new ideas.
You’re not alone—common presentation challenges
Many surgeons, including ourselves, encounter similar obstacles when presenting research. Presentations are often overloaded with information, making slides difficult to follow and diluting the impact of key findings. Some lack a clear narrative, focusing solely on data without sufficient context or explanation, which can be hard for the audience to engage with. There is also the risk of using language or technical detail that does not match the audience’s background, limiting understanding and discussion.
Speaking confidently and engaging with the audience are skills that require practice, and managing time effectively during a presentation is a common concern. The list goes on – but how can we be proactive and better prepared?
6 principles for effective research presentations
To enhance the impact of your presentations, several strategies are worth considering. These are some tips and tricks that we have learned along the way.
1. Know your audience
Knowing your audience is fundamental to effective research presentation. Whether speaking to CMF specialists, general surgeons, or a broader medical audience, adjusting the level of detail and terminology accordingly helps ensure your message is received as intended. Providing necessary background and avoiding assumptions about prior knowledge can make your research more accessible and relevant.
For example, when presenting to a multidisciplinary team, briefly outline the clinical relevance before delving into technical details. We find that engaging listeners directly, for example by asking questions or inviting them to interpret a clinical image, creates a more interactive and attentive atmosphere.
2. Structure can make it or break it
A logical structure guides the audience through your research. There are many ways to go about this. We recommend starting with a strong opening that captures attention, such as sharing a rare case or posing a clinical question for the audience to consider. Present the case, follow with relevant imaging, discuss assessment and treatment, and then reveal the outcome. This flow helps maintain interest and provides a clear narrative.
Summarizing at the end reinforces the main points and ensures the audience leaves with a clear take-home message. Consider starting with a clinical question or problem statement, as this sets the context and relevance for the audience right away.
For example, at a prior FACE AHEAD, many presenters began by highlighting a challenging or unusual patient case that immediately resonated with the audience. One memorable session opened with the story of a complex condylar fracture, inviting attendees to consider possible approaches before revealing imaging and treatment details. This strategy not only engaged the audience but also set the stage for an interactive discussion about best practices and new techniques. By structuring the presentation around a real-world scenario, the speaker was able to make the research findings more relatable and applicable to everyday clinical practice.
3. Clarity is key
Clarity should be prioritized throughout. Focus on the most important findings and minimize extraneous information. Slides should be simple—less is more. Avoid clutter, stick to one main idea per slide, and use concise text rather than lengthy paragraphs.
Well-designed visuals, such as diagrams, tables, and clinical images, can be powerful tools for supporting your message. However, these images, icons, and charts should be relevant and help convey your point, not just fill space. For example, when illustrating the classification of condylar fractures, clear figures can demonstrate anatomical and clinical details in a memorable way. Similarly, a visual explanation of the mechanism of secondary enophthalmos can immediately communicate the concept without excessive explanation.
Slides should be easy to read, with clear labels and concise text. The “assertion-evidence” slide design is particularly effective: start each slide with a clear statement and support it with data or relevant visuals. Limiting slides to one main idea for each, using short direct sentences rather than dense bullet points, and highlighting key rows or columns in tables with color or bolding can all help emphasize your most important results. For data, simple graphs, such as bar, line, or pie charts, are often most effective, especially when annotated directly with key findings.
4. Get the audience excited and engaged
Encourage questions and discussion when possible. Making eye contact, using body language and gestures, and varying your tone and pace all help maintain interest. Interact with your audience by asking questions, involving listeners, and responding to feedback. Introducing rhetorical questions and allowing brief pauses after key points gives the audience time to absorb information and reflect on its relevance. Sharing brief, anonymized case examples or clinical anecdotes can make your findings more relatable.
5. Practice makes perfect
Rehearse your presentation to ensure smooth delivery and adherence to time limits. Practicing with colleagues can help identify areas for clarification and improve overall confidence. Recording practice sessions and reviewing them for pacing, clarity, and volume is a useful technique. Timing each section of your talk ensures you stay within allotted limits, and preparing concise answers for anticipated questions allows for effective engagement during Q&A. Practicing transitions between slides, particularly when moving from background to results or discussion, helps maintain flow and coherence.
Train yourself to avoid reading directly from your slides and instead use them as prompts for deeper explanation tends to make the presentation more enjoyable for those in the audience.
6. Avoid awkward technical mishaps
Managing technical aspects is another important consideration. Test slides and equipment in advance to prevent disruptions. Familiarize yourself with the AV setup at the venue, including clickers, microphones, and screen resolution, if possible, to avoid last-minute issues.
Use high-contrast colors and readable fonts for accessibility, and limit animations and transitions to those that genuinely aid understanding. Bring your presentation in multiple formats—such as USB, email, or cloud storage—to provide a safety net. Embed videos or images directly in slides, rather than relying on external links, for reliability. This will allow you to stay focused on the important things you have to say and not be distracted by foreseeable technical issues.
Good research presentations matter more than you think
Effective presentation skills benefit not only individual surgeons but the CMF field as a whole. They facilitate the exchange of ideas, support the adoption of new techniques, and contribute to ongoing professional development.
As our field continues to evolve, the ability to communicate research findings clearly will remain a core academic competency. Sharing experiences and research through presentations not only educates others, but also builds professional networks, fosters international collaboration, and strengthens the academic community. Opportunities to present at forums like FACE AHEAD or publish in journals such as CMTR allow us to showcase our work and connect with colleagues worldwide. These activities are crucial for effective knowledge translation, ensuring that research is not just shared but also understood, adopted, and applied in clinical settings across the globe.
For CMF surgeons, presenting research is an integral part of academic practice. By focusing on clarity, structure, and audience engagement, we can ensure that our work contributes meaningfully to the advancement of CMF surgery. Investing time in developing these skills is a practical step toward enhancing both individual and collective progress within our specialty. To accelerate the translation of our research from publication to clinical practice, we must take proactive steps to educate, inform, and engage others in meaningful discussions about the value our findings bring to patient care. Take advantage of opportunities to present at academic meetings and publish in open access journals. Together, we can advance the quality and impact of CMF research communication.
Did you know?
FACE AHEAD provides a unique stage for CMF surgeons to showcase their innovative research, breakthrough techniques, and clinical insights to an international community of leading craniomaxillofacial experts. Held every two years, the summit highlights cutting-edge work from around the world. Plus, all accepted abstracts and e-posters are published free of charge and open access in AO CMF’s journal CMTR, giving your work global visibility.
About the authors:
Prof. Mike Y.Y. Leung, BDS (HK), MDS (HK), MOSRCS (Edin), FHKAM (DS), FCDSHK (OMS), PhD (HK), serves as a Clinical Professor and Postgraduate Programme Director in Oral and Maxillofacial Surgery at the Faculty of Dentistry, The University of Hong Kong. Additionally, he holds the position of Associate Dean (Global Engagement and Development) of the Faculty. Prof. Leung is also the President of the Hong Kong Association of Oral and Maxillofacial Surgeons. On an international level, he represents the Asia Pacific region in the AOCMF Education Commission and is the President of the Asian Association of Oral and Maxillofacial Surgeons.
After graduating with a BDS, MDS (OMFS), and PhD from the University of Hong Kong, Prof. Leung began his career in oral and maxillofacial surgery in Hong Kong. With over 140 publications in peer-reviewed international journals, he ranks among the Top 2% of the World's Most Cited Scientists by Stanford University for 2021-2024. Prof. Leung's clinical and research interests encompass orthognathic surgery, management of obstructive sleep apnea, temporomandibular disorder, trigeminal nerve repair, and management of complications after dentoalveolar surgery. As a renowned expert in his field, he frequently delivers lectures both regionally in the Asia Pacific and internationally.
Prof. Dr. Mohamed Hazem AbdelAzeem is a Consultant in Plastic and Cranio-maxillofacial Surgery, currently serving as a Professor at Cairo University’s Faculty of Medicine. He holds an MB BCH, MSc, MD, MRCS(Eng), and FRCS(Glasg), demonstrating his extensive training and expertise in the field.
A fellow of Freiburg University in Germany and AO CMF in Switzerland, Professor Abdelazeem is actively involved in the AO CMF community as both a Faculty member and a Board Member for the MENA region. He chairs the AOCMF Community Development Commission for MENA and is a founding Board Member of the Egyptian Society of Craniomaxillofacial Surgery (EG-CMF).
In addition to his academic roles, he practices in private clinics located in central Cairo and the New Giza area, specializing in a range of plastic surgery procedures with a focus on minimally invasive and endoscopy-assisted surgeries within cranio-maxillofacial surgery. His commitment to advancing surgical techniques and community development underscores his significance in the field.
You might also be interested in...
Craniomaxillofacial Trauma & Reconstruction
AO CMF's official peer-reviewed journal, CMTR is devoted to the study and treatment of craniomaxillofacial conditions.
Elevate your career at FACE AHEAD 2026
Abstract submission is now open for FACE AHEAD 2026, the CMF summit, in Bangkok, Thailand, October 1–3.
AO Knowledge Translation
AO’s Knowledge Translation (KT) initiative accelerates the integration of new research into clinical practice.