Precision surgery—balancing risk and impact in maxillofacial surgery
BY DR ARIEL HIRSCHHORN
At 40 years old, Jessie, a mother of three, sat in our clinic, facing a complex decision. Diagnosed with an ameloblastoma, she was presented with a conventional approach: radical resection, free flap reconstruction, which would mean a significant change to her appearance and a long recovery. The implications extended beyond surgical risks—they affected her identity, function, and quality of life. I want to share her story to highlight the considerations, how to balance the risks and impact in maxillofacial surgery, and future direction of precision surgery.
-
Read the quick summary:
- A patient presented with an ameloblastoma; conventional treatment would have involved radical resection and free flap reconstruction, with consequences for her appearance and function, plus a long recovery time.
- The surgical team took a different approach, beginning with shrinking the tumor before minimally invasive surgery that maintained her facial contours and reduced functional and aesthetic disruption.
- The team has adopted this approach for all benign craniofacial tumors.
- The article discusses risk and sequela, and the importance of each member's role in a multidisciplinary team. It outlines the step-by-step processes that were involved in this case, and discusses the ways that risk-adapted, precision-driven strategies can improve patient outcomes.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
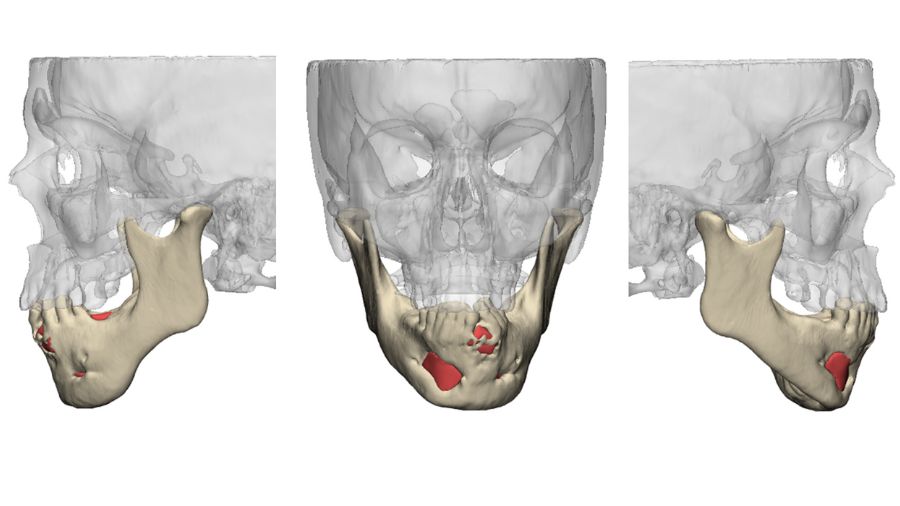
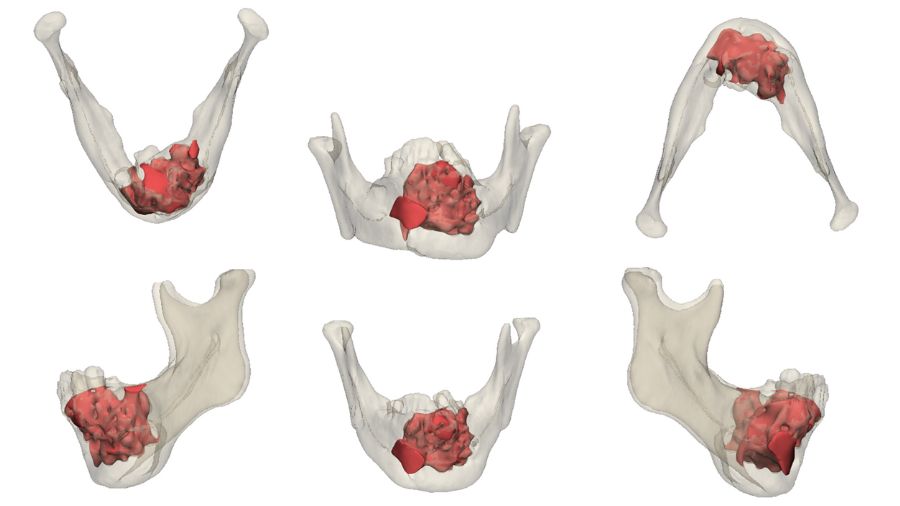
Patient-centered innovation is a guiding principle at our practice in Sheba and we decided to pursue an alternative. By leveraging molecular profiling and targeted therapy, we were able to shrink the tumor before surgery, preserving her natural appearance. Instead of radical resection and a free flap reconstruction, she underwent a minimally invasive surgery that maintained her facial contours, reducing functional and aesthetic disruption. This approach not only preserved her ability to eat and speak but allowed her to return to her family with confidence and continuity in her appearance.
Ameloblastoma was the first tumor where we applied this risk-adapted approach. Today, we have extended this methodology to all benign craniofacial tumors, ensuring that each patient receives treatment tailored to oncologic safety and long-term quality of life.
Differentiating risk and sequela in a changing surgical landscape
Risk, in the context of maxillofacial surgery, is the probability that a certain intervention will lead to a suboptimal or unintended outcome. It encompasses both oncologic risk (such as recurrence) and functional risk (such as impaired speech, mastication, or facial aesthetics). Proper risk assessment involves weighing these factors systematically to optimize outcomes while maintaining patient safety.
It is important to differentiate between risk and sequela. Risk refers to the potential for an adverse outcome, such as recurrence or complications, whereas sequela refers to the inevitable consequences of a specific intervention. For example, an aggressive surgical approach may reduce recurrence risk, but it comes with a certainty of functional and aesthetic impairment.
In contrast, a risk-adapted approach that balances oncologic control with tissue preservation might carry a slightly higher potential for recurrence but avoids the guaranteed morbidity associated with overly aggressive treatment.
The role of a multidisciplinary team in maxillofacial surgery
Managing complex craniofacial tumors requires collaboration across multiple disciplines ensuring that each patient benefits from a level of coordinated expertise that defines advanced healthcare systems. A multidisciplinary team approach allows for more comprehensive risk assessment, adaptive treatment strategies, and improved patient-centered care.
Key members of the team include:
Maxillofacial surgeons—responsible for risk-adapted surgical planning and reconstructive techniques
Medical oncologists—guide the use of targeted therapies and systemic treatments pre- and post-operatively
Radiologists—monitor tumor progression and treatment response through advanced imaging, pinpointing the optimal timing of surgical intervention
Pathologists—conduct molecular profiling and histopathologic analysis to refine diagnoses and treatment planning
Effective teamwork is crucial in dynamically adapting treatment protocols to each patient’s unique needs. By integrating expertise across fields, we can make informed, calculated decisions that balance oncologic control with the highest possible functional and aesthetic outcomes.
A stepwise approach to precision surgery
The implementation of precision surgery begins with a structured, data-driven approach to evaluating and treating craniofacial tumors. The key steps in this methodology include:
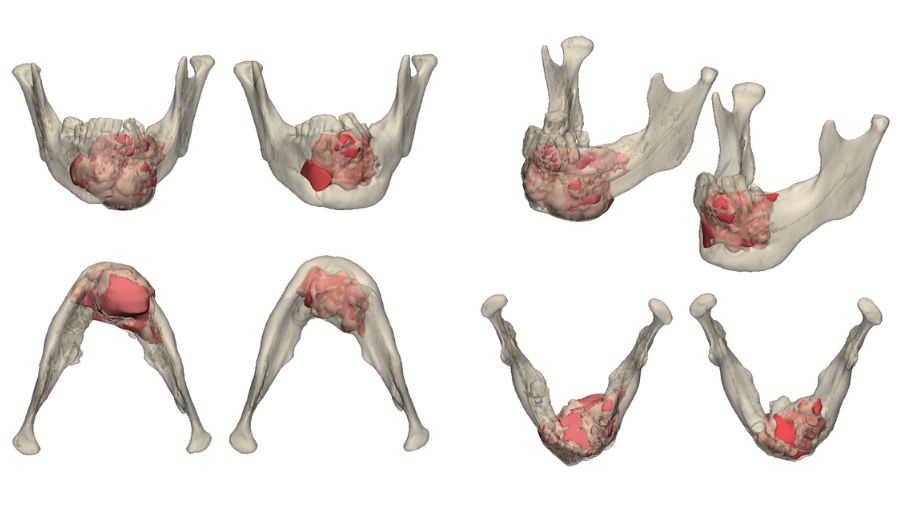
- Molecular Profiling—understanding tumor biology: Before any surgical intervention, we perform molecular profiling to identify key mutations that drive tumor behavior. For example, BRAF V600E mutations in ameloblastomas have been linked to responsiveness to targeted inhibitors. Similarly, SMO and PTCH1 mutations in odontogenic tumors provide valuable insights into potential therapeutic pathways. Understanding the genetic makeup of the tumor allows us to tailor treatment strategies accordingly.
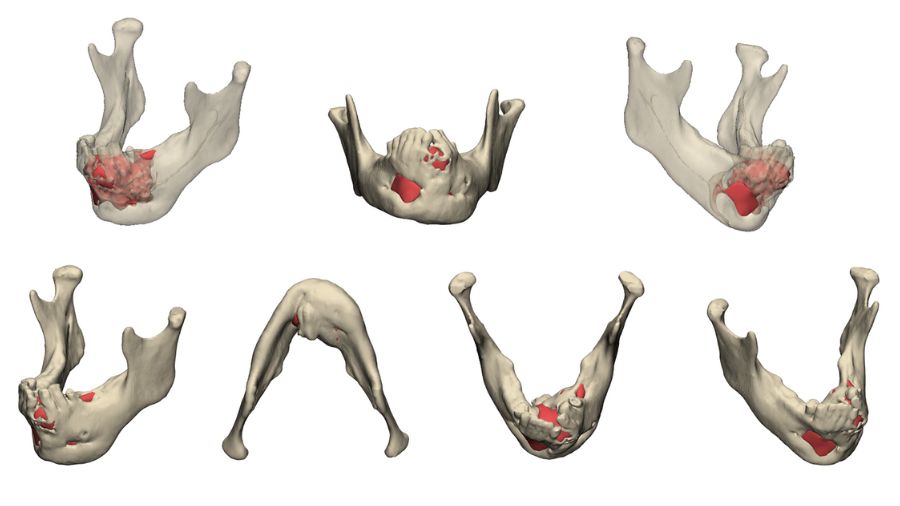
- Targeted Therapy—shrinking the tumor before surgery When an actionable mutation is identified, systemic therapy can be initiated preoperatively to reduce tumor burden. Targeted therapies, such as BRAF inhibitors for ameloblastoma or Hedgehog pathway inhibitors for odontogenic tumors, can significantly shrink tumors, thereby preserving healthy tissue and reducing the extent of resection required.
- Bone Regeneration and Reconstruction Optimization: One of the unexpected benefits of targeted therapy is that, in some cases, bone regeneration is observed when the tumor shrinks. Instead of relying solely on grafting and reconstruction, we can leverage the body's natural regenerative capacity, reducing morbidity and improving patient outcomes.
Risk-Adapted Surgical Planning: Using risk matrices and functional outcome analysis, we determine the optimal balance between oncologic control and tissue preservation. This ensures that each case is managed based on individual risk factors rather than standardized protocols, allowing for a more personalized approach to surgery. - Real-Time Decision-Making During Surgery: Rather than committing to a single plan preoperatively, we integrate intraoperative findings and imaging to guide the extent of resection. reflecting a dynamic, patient-adaptive approach that prioritizes both medical precision and ethical responsibility. This flexibility allows us to adapt the surgery dynamically based on real-time tissue response.
- Postoperative Surveillance and Functional Outcome Measurement: Beyond recurrence monitoring, we incorporate Patient-Reported Outcome Measures (PROMs) to evaluate speech, mastication, and aesthetics, ensuring that surgical success is defined not only by oncologic control but also by patient quality of life.
A structured approach to risk allows us to individualize treatment rather than apply a rigid, one-size-fits-all protocol. Patients should be active participants in risk assessment, understanding that taking a calculated risk—such as opting for neoadjuvant therapy to shrink a tumor before resection—can significantly improve their quality of life. Shared decision-making ensures that surgeons and patients align on priorities, balancing the need for oncologic control with the benefits of functional preservation.
The future of maxillofacial surgery: a shift in risk assessment
For years, maxillofacial surgery has been guided by a principle of maximal resection for minimal recurrence. However, as our understanding of tumor behavior and functional rehabilitation deepens, this model is evolving.
We can redefine risk, ensuring oncologic control while prioritizing patient functionality. We can move beyond recurrence as the sole metric, integrating patient-reported outcomes and functional restoration into success criteria.
We will develop risk-adapted, precision-driven strategies, leveraging real-time data and molecular profiling to personalize treatment. In a field that balances oncologic necessity with reconstructive precision, the ability to manage risk dynamically is key—an approach that ensures patients are treated with both technical excellence and an unwavering commitment to their long-term well-being. As surgeons, our responsibility is to continuously evaluate and refine our approach to maximize both oncologic safety and functional outcomes.
Established surgical protocols continue to serve as the foundation of care; however, incorporating molecular profiling and patient-specific risk factors allows for a more refined and individualized therapeutic approach—broadening treatment possibilities and enhancing clinical outcomes. This ensures that treatment strategies remain evidence-based while allowing for individualized decision-making that prioritizes both oncologic safety and functional outcomes. The challenge ahead is not whether we can adopt these strategies, but how effectively we implement them to benefit every patient who entrusts us with their care.
About the author:
Dr Ariel Hirschhorn is an attending surgeon in the Department of Oral and Maxillofacial Surgery at Sheba Medical Center, Tel Hashomer, Israel — ranked #8 on Newsweek’s list of the World’s Best Hospitals. At Sheba, genomic insights are integrated with advanced digital surgical planning tools to deliver highly individualized, patient-specific treatment strategies. These include molecularly guided therapies, 3D-printed anatomical models, and virtual simulations — enabling organ-preserving approaches in complex cranio-maxillofacial surgical challenges. As part of a multidisciplinary team, Dr Hirschhorn is involved in driving clinical innovation in this evolving field.
He earned his DMD from the Hebrew University of Jerusalem and completed his residency in oral and maxillofacial surgery at Sheba, followed by an AO CMF fellowship at the University Hospital Basel, Switzerland. Dr Hirschhorn is an AO CMF faculty member and has previously served as an adjunct representative on the AO CMF Community Development Commission for the European and Southern African region. He is currently the AO CMF Fellowship Program coordinator at Sheba.
Dr Hirschhorn's clinical and translational research focuses on immunomodulatory strategies to enhance bone regeneration in craniofacial reconstruction.
References and further reading:
- Hirschhorn A, Grynberg S, Campino GA, Dobriyan A, Patel V, Greenberg G, Yacobi R, Barshack I, Yahalom R, Toren A, Vered M. Histopathologic and Molecular Insights Following the Management of Ameloblastomas via Targeted Therapies - Pathological and Clinical Perspectives. Head Neck Pathol. 2024 Dec 2;18(1):129. doi: 10.1007/s12105-024-01734-2. PMID: 39621130; PMCID: PMC11612134.
- Grynberg S, Vered M, Shapira-Frommer R, Asher N, Ben-Betzalel G, Stoff R, Steinberg Y, Amariglio N, Greenberg G, Barshack I, Toren A, Yahalom R, Schachter J, Rechavi G, Hirschhorn A, Abebe Campino G. Neoadjuvant BRAF-targeted therapy for ameloblastoma of the mandible: an organ preservation approach. J Natl Cancer Inst. 2024 Apr 5;116(4):539-546. doi: 10.1093/jnci/djad232. Erratum in: J Natl Cancer Inst. 2024 Apr 5;116(4):631. doi: 10.1093/jnci/djad264. PMID: 37966914.
- Hirschhorn A, Campino GA, Vered M, Greenberg G, Yacobi R, Yahalom R, Barshack I, Toren A, Amariglio N, Rechavi G. Upfront rational therapy in BRAF V600E mutated pediatric ameloblastoma promotes ad integrum mandibular regeneration. J Tissue Eng Regen Med. 2021 Dec;15(12):1155-1161. doi: 10.1002/term.3254. Epub 2021 Oct 9. PMID: 34599642.
You might also be interested in:
Global Oral Cancer Diploma
Join the next global cohort in 2025! Register your interest now! 10 online modules over 10 months.
AO Surgery Reference, your vital guide
The all-in-one online reference supporting you from patient assessment to aftercare.
CMTR—official scientific publication
Craniomaxillofacial Trauma & Reconstruction (CMTR) is now open access.
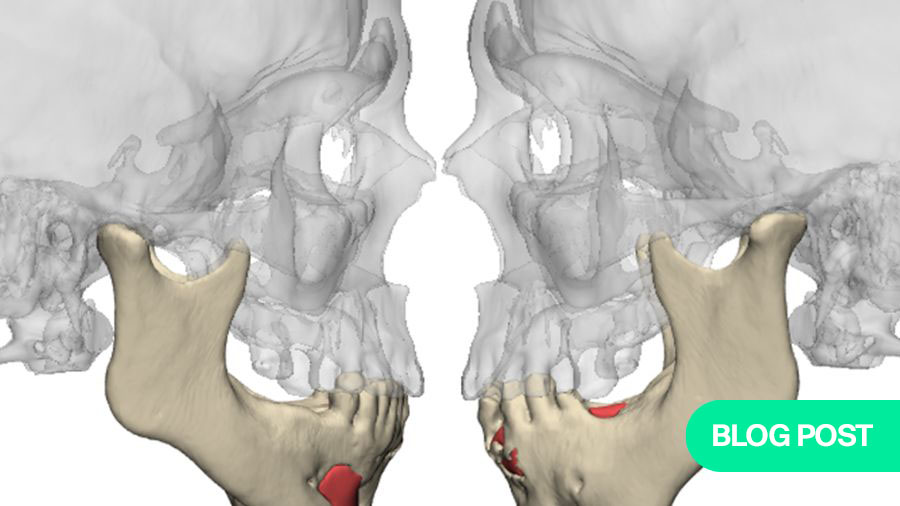
Blog: ameloblastoma and a simple drug
Read another article from Ariel Hirschhorn's practice on treating young ameloblastoma patients.