Orbital Reconstruction: How patient specific technologies helped with desired outcome in Silent Sinus Syndrome
BY DR ALBERTO ROCHA PEREIRA AND DR ADRIÁN CARDÍN PEREDA
Silent Sinus Syndrome (SSS) is a very rare condition, typically consisting of asymptomatic and spontaneous collapse of the maxillary antrum walls and orbital floor. Alberto Rocha Pereira and Adrián Cardín Pereda explore the challenges and controversies in diagnosis and management, and why early diagnosis is vital.
Silent Sinus Syndrome (SSS), also called imploding antrum syndrome or chronic maxillary atelectasis, is a very rare condition, typically consisting of asymptomatic and spontaneous collapse of the maxillary antrum walls and orbital floor. First described by Montgomery in 1964, the term was coined by Soparkar three decades later. Due to its singularity, the literature has often emphasized the confusion around its definition, diagnosis, and optimal management.
The etiology of SSS still elicits controversy. Patients deny previous sinus disease or facial trauma. Currently, it is commonly accepted that collapse of the orbital floor is induced by negative pressure generated by resorption of gas after an ostium occlusion that may happen during the first decades of life. Sometimes, SSS is described as hypoplastic, however this term should be reserved for congenital underdevelopment. In a similar fashion, SSS and chronic maxillary atelectasis are terms which have been used as synonyms with some authors sustaining that the two are different clinical entities, as the fundamental difference between both is the frequent absence of nasosinusal symptoms in SSS.
Thus, for the diagnosis of SSS the following criteria have been proposed: 1-absence of significant sinus complaints, 2-remodeling and inferior bowing of the maxillary roof/ orbital floor as demonstrated on a Computed Tomography (CT) scan, 3-no history of orbital trauma or enophthalmos of a different etiology, and 4-no documented congenital deformity or significant anatomic abnormality of the sinus and/or nasal cavity.
Why it is important to talk about Silent Sinus Syndrome
- The silent sinus syndrome is an acquired uncommon condition in which early diagnosis is vital. Late diagnosis may require correction of secondary orbital deformities. In this scenario, patient-specific implants and intraoperative navigation with CT scan have emerged as safe and effective tools, with current evidence and personal experience supporting its use.
- To diagnose and treat this condition correctly, it is essential to be familiar with it, conduct a correct differential diagnosis, and exclude other causes of orbital alteration as well as sinus pathology.
- Clinical manifestation of silent sinus syndrome typically consists of asymptomatic enophthalmos, hypoglobus, and facial asymmetry. Nonetheless, diplopia, sinusitis, rhinorrhea, postnasal drip, facial pain, or pressure may also be present.
Treatment options for Silent Sinus Syndrome
Historically, surgical treatment consisted in Caldwell-Luc sinus surgery with inferior meatotomy and concurrent repair of the orbital floor. Blackwell and colleagues described in the early nineties treating successfully SSS with endoscopic maxillary antrostomy combined with a transconjunctival orbital floor repair.
Currently, in order to restore the natural ventilation of the maxillary sinus, the SSS treatment of choice appears to be endoscopic maxillary antrostomy, commonly referred as functional endoscopic sinus surgery (FESS). However, the main debate in literature remains the requirement and timing of the orbital floor reconstruction. While some authors would rather perform endoscopic antrostomy and reconstruction of the orbital floor at the same time, others consider that a two-stage approach is more appropriate, with an interval between antrostomy and the orbital floor reconstruction.
The proposed timespan for a potential postponed orbital reconstruction, according to the literature, is six months. On the other hand, orbital volume should accurately be restored to avoid undesirable aesthetical consequences for the patient. In this regard, an assortment of alloplastic and autogenous options is currently available for reconstruction, being titanium plates, nylon sheets, and Medpor implants the most popular.
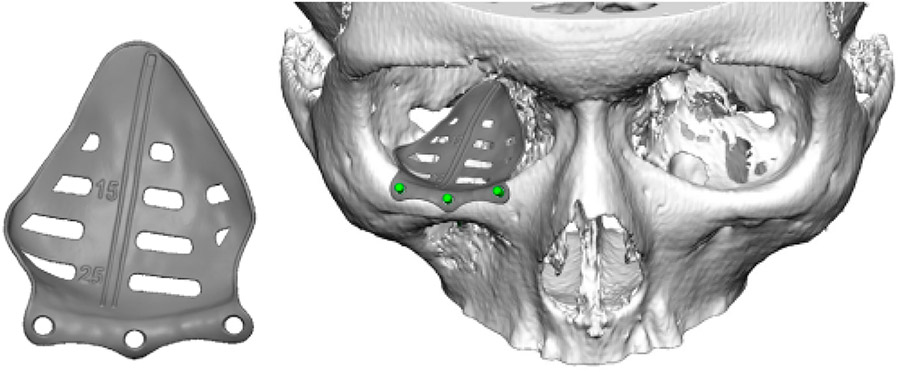
Because of a superior performance over standard implants, patient-specific implants, developed by computer assisted design and computer assisted manufacturing (CAD/CAM) systems, for craniomaxillofacial reconstruction have grown in popularity in the last decade. Customized implants allow a more precise adaptation to the region of implantation, ideal shape and symmetry, with reduced surgical times, and better cosmetic outcomes.
Computer assisted planning and patient-specific implants
We used computer assisted planning and patient-specific implants assisted by intraoperative navigation and CT control in a case with a 33-year-old woman, who was referred to our plastic surgery outpatient department in Hospital da Luz in Lisbon. She reported a sinking right eyeball with no other findings or complaints.
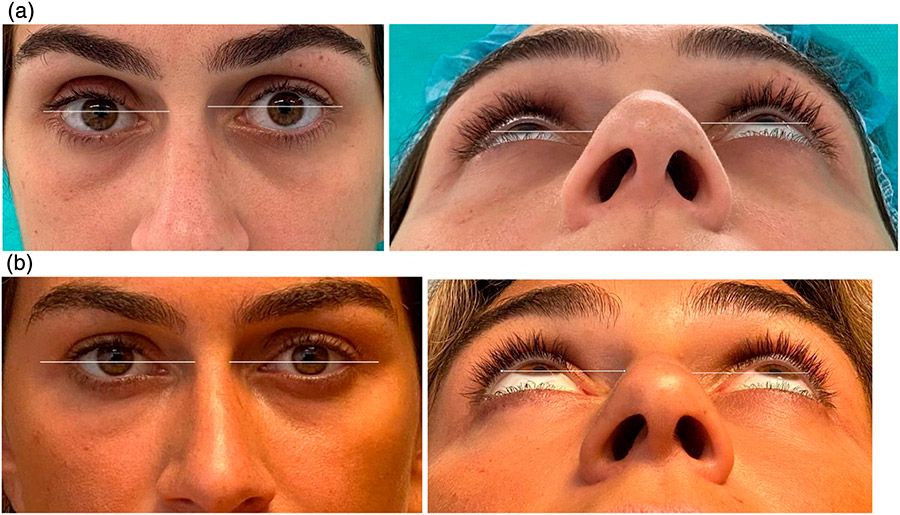
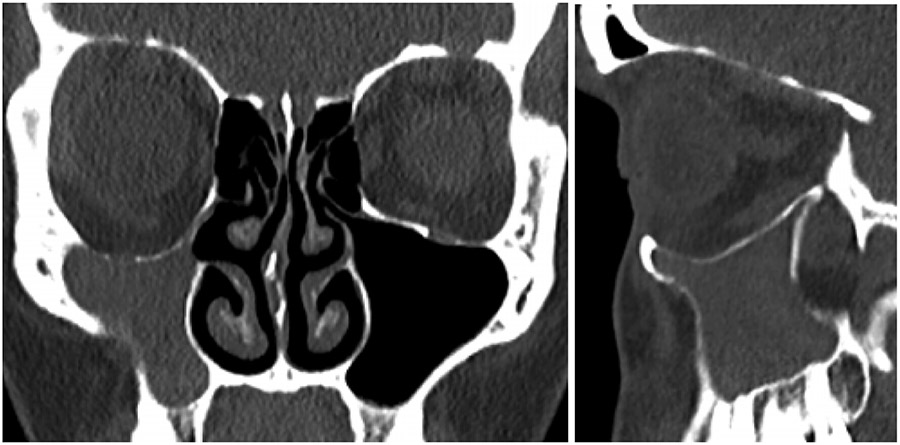
The patient reported a progressive, painless descent in her right eyeball over the last seven months, with no history of facial trauma or nasosinusal disorders. Clinical examination revealed enophthalmos, vertical dystopia and upper eyelid sulcus asymmetry (Fig. 1). Facial CT scan revealed a decreased right maxillary sinus volume with increased right orbital volume, downward displacement of orbital floor and collapse of the maxillary sinus (Fig. 2). Thus, a diagnosis of SSS was made based on the clinical and radiological findings.
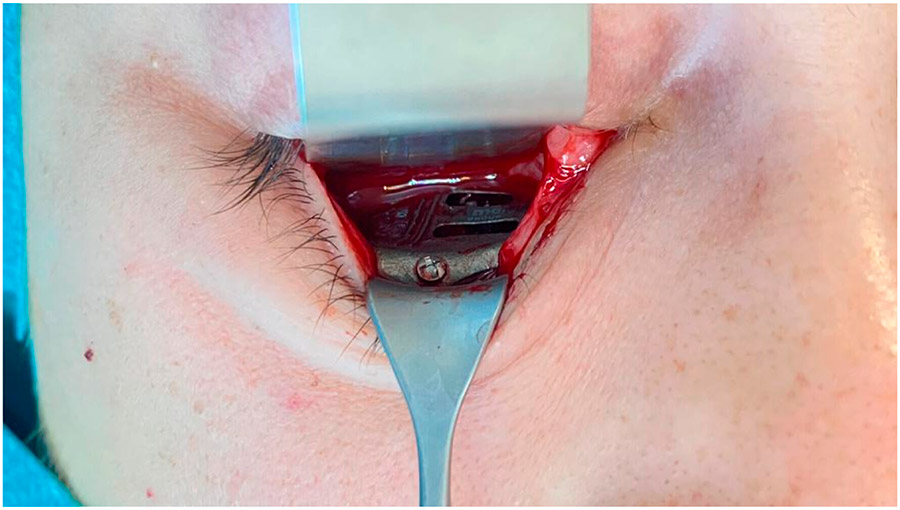
The patient underwent a Caldwell-Luc approach and concurrent orbital floor reconstruction. A one-stage approach was chosen for a faster recovery and single surgery. Correction of enophthalmos and dystopia was performed using a patient-specific CAD/CAM implant (Fig. 3) assisted by intraoperative navigation and CT scan (Fig 4.). The 0.3mm orbital floor titanium plate was placed through a transconjunctival approach (Fig. 5). The patient was found to be complaint free and full recovered at 6th-month follow-up (Fig 1.).
Aim is to normalize sinus aeration and restore orbital anatomy
Initial management of SSS could be conservative according to the severity and patient complains. If the condition is progressive, then proper sinus drainage must be restored by enlargement of the maxillary ostium. Currently, the procedure of choice to restore aeration of the maxillary sinus is FESS. In our case, since we did not have an endoscope available in our department, sinus repermeabilization was performed using the Caldwell-Luc technique, a procedure traditionally performed in literature and which we have experience with. Sinus drainage and aeration was successfully achieved.
Interventions improving antrum aeration usually stop the progress of maxillary sinus reduction, but no significant restoration of orbital volume is achieved.
Consequently, the treatment of SSS has two specific objectives: to normalize maxillary antrum aeration and to restore orbital anatomy. In cases where enophthalmos, diplopia or cosmetic deformity are significant, the tendency in the literature is to perform surgical treatment in a single procedure. Enophthalmos is considered objectively significant from 2mm onwards. In our case, the patient did not present vision alterations, but she did show significant enophthalmos and dystopia.
Whether to perform the treatment in one or two stages continues to be a matter of controversy, with opinions for and against. Advocates of a two-stage treatment argue the possibility of avoiding orbital reconstruction surgery once sinus aeration is restored, by slowing the progression of orbital collapse and even achieving minor sinus re-expansions. Accordingly, some of the cases reported in the literature waited between two and six months after sinus repermeabilization for orbital reconstruction. This argument is especially relevant in children. Moreover, the avoidance of orbital infections associated with the one-stage procedure has also been argued. In the other hand, proponents of one-stage repair procedure claim a lower anesthetic risk associated with a single surgery, shorter hospitalization time and costs, and a faster rehabilitation of the patient.
In our case, the patient preferred to be treated in a single procedure, because of the above reasons. In addition, the chances of recovering proper orbital volume with the mere repermeabilization of the sinus in an adult were considered to be low.
What to watch out for with orbital floor implants and complications
In order to return a normal facial appearance, three deformities must be addressed: the hypoglobus, the enophthalmos, and the upper lid sulcus deformity. Although orbital floor implants often improve the anterior projection of the eye and improve hypoglobus, they can hardly by themselves correct the deformity of the upper eyelid sulcus.
When significant upper lid sulcus depression is present, a pre-aponeurotic dermis fat graft and/or alloplastic materials may improve aesthetic outcome. In our case, proper repositioning of the eyeball, with PSI implant just at the orbital floor, completely corrected the upper lid sulcus deformity (fig 1).
In traumatic orbital reconstruction, factors determining the vertical position of the globe should be carefully evaluated while pre-surgical planning is performed. These determinants include integrity of the suspensory ligaments of Lockwood, intact orbital walls, periorbital fat volume, and extraocular muscles layout.
In this particular pathology, however, just one of these factors is involved in asymmetry: the orbital floor deformity or resorption. To achieve repositioning of the globe, subperiosteal grafts or implants, are commonly used. Reasons advocating the use of bone grafts include the biocompatibility and a lower risk of extrusion, foreign body reaction, or infection. On the other hand, resorption of the bone, the need of two surgical fields and potential complications at donor sites are the main disadvantages with this technique.
Furthermore, the osseous remodeling and anatomic landmarks loss present in this syndrome imply a huge challenge when trying to reconstruct the orbit with stock implants. In addition, preformed titanium meshes may facilitate the bending process, but it is often difficult to predict the exact positioning of the mesh, lengthens the operative time and does not produce as satisfactory aesthetic and functional results when compared to a specific implant. On the other hand, the use of a customized virtual planned implant, as in our case, enables a precise orbital reconstruction restoring shape and volume accurately with symmetric replacement of the eyeball. Since these implants are specifically designed to fit in a stable and precise position, the risk of damaging the optic nerve and other important structures minimizes.
Moreover, virtual surgical planning can offer the surgeon a better understanding of the anatomy. Intraoperative navigation and CT intraoperative control, add extra safety and greater accuracy to the procedure, controlling ideal positioning of the implant and avoiding complications regarding optic nerve damage. The use of intraoperative navigation has been shown to offer a significantly better orbital volume and eyeball projection, without increasing surgery duration. Customized titanium implants accurately reproduce orbital contours thus restoring orbital volume. This reduces operative time and improves the functional and aesthetic outcomes of post-traumatic orbital reconstruction.
About the authors:
Dr. Alberto Rocha Pereira is head of the Plastic, Aesthetic and Reconstructive Surgery Department at the Hospital da Luz in Lisbon, and consultant physician at the Plastic, Aesthetic and Reconstructive Surgery Department of the Instituto Português de Oncologia in Lisbon. He has been head of the Plastic and Maxillofacial Surgery Department at the Hospital das Forças Armadas in Lisbon, as well as member of Craniofacial Expert Group of AO Foundation and president of the AO Foundation Distraction Task Force. His main area of expertise is facial reconstructive surgery, being a renowned expert in distraction osteogenesis.
You might also be interested in:
Open a world of opportunities with AO CMF membership
AO CMF member plus privileges include free article submission to Craniomaxillofacial Research & Innovation.
Abstract submission for FACE AHEAD is open!
Present your research at FACE AHEAD 2024. Submission Deadline: September 18, 2023.
AO CMF Course finder
Find your next educational event on orthognathic surgery in our course finder.