Pediatric TMJ reconstructions—emerging research shows superiority of costochondral graft in autologous experience
BY DR AJOY ROYCHOUDURY

The goals of pediatric Temporomandibular Joint (TMJ) reconstruction are to maintain pain-free mouth opening and prevent re-ankylosis or heterotopic bone formation. We are doing these techniques in small children, but small children will grow. This means adopting a technique that will grow with the children, that would limit asymmetry. There are considerations to differing techniques to TMJ reconstruction in children.
Obviously, children who have undergone TMJ surgery at a very young age will have a small mandible. This decreases the airway space and predisposes these patients to obstructive sleep apnea later on, so we also need to increase the airway space.
This article explores the indications of pediatric TMJ reconstruction using autologous tissues, such as costochondral grafts and transport disc destruction osteogenesis. But what are the strategies to incorporate growth in that, and reduce heterotopic bone at the reconstruction site?
We must also consider TMJ ankylosis, a very challenging area for a TMJ joint reconstruction in children.
The importance of reconstruction
TMJ reconstruction can be alloplastic or autogenous. Alloplastic reconstructions with ramal restorations, with total joint replacements and now Silastic blocks, are again coming into fashion with the two-stage total joint replacements.
Let us first look at what happens when you do no reconstruction in cases where the children are operated on, or diseases of the temporomandibular joint ankylosis, let's say temporomandibular joint. If we consider a case of bilateral ankylosis, one year postoperative, the patient will probably be doing fine, and function is restored. Even three or ten years on, we might say the same.
But what has really happened is that while the mouth opening is adequate, no catch-up growth has happened, even when the functional matrix is restored as per Moss’s theory. Functional treatment has happened, but the growth has not, so aesthetics is compromised.
Another reason why reconstruction should be done is osteoarthrotomy, or a lack of growth in the condyle, if you don’t reconstruct them. We have shown that in two of our publications, where there is a loss of vertical height and the mandible rotated backwards. This pushes the tongue into a more posterior position, causing obstructive sleep apnea. These cases are detailed in the January 2021 and December 2021 Journal of Oral Maxillofacial Surgery.
Therefore, we might ask: do we opt for alloplastic TMJ reconstruction, with or without ramal restoration? I would suggest that without ramal restoration is absolutely nothing in terms of TMJ reconstruction.
However, let’s think about the Silastic blocks. When you restore the ramus, these can act as spacers, and a future joint replacement surgery can be undertaken when the patient grows and matures. There are however some pitfalls to using Silastic spacers. There’s a possibility of displacement, of huge heterotopic bone or foreign body reaction and infection. There’s also a chance of degradation and systemic complications.
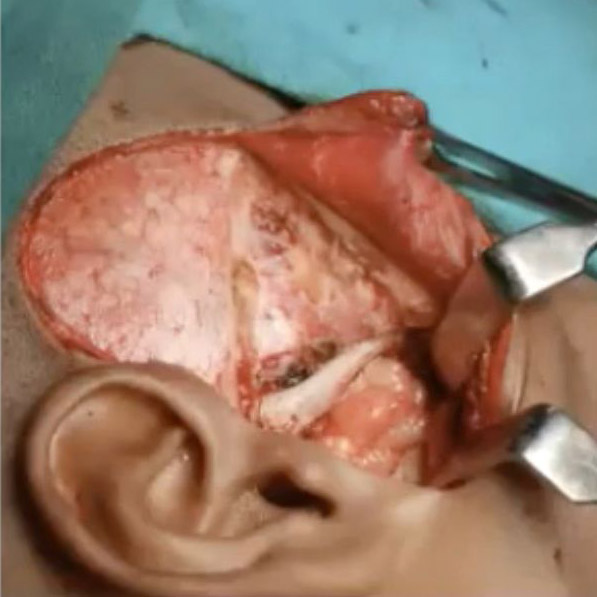
So, what should you do? Let’s consider a case of a chondrectomy in a child of nine years old. In this case, the Silastic block occupied the entire space of the osteoarthrotomy, and it is wired to the zygomatic bone. Once you wire that, there is no chance of this block moving anywhere. When we see her at 15, and at 20, she is fine.
The value of fat in reconstruction
Pediatric reconstructions have traditionally been autogenous, and autogenous with or without growth center transplantation. The cases without growth center transplantation utilize the temporalis, fat, skin, and auricular cartilage. By contrast, growth center transplantation and ramus-condyle unit reconstructions are costochondral graft, sternoclavicular graft and neo condyles.
I feel that the temporalis and fat approaches are just strategies for the reduction of heterotopic bone formation. Whenever we do periodic TMJ reconstruction, we must also think about restoration of the ramus-condyle unit, because it is an area where a lot of bone might fall.
Now, we all know that the temporal is a bipennate muscle occupying the area of the temporal fossa. But a lovely paper from Lin Cheung highlights that there’s a lot of vascular there, and because of this, you can split these muscles and the muscle will survive. However, the temporalis muscle will have to be rotated.
The next strategy to reduce the heterotopic bone formation in the reconstructed area is the fat, which can be taken from the buccal pad or the abdomen. We have a new method, which can be found in the 2015 British Journal of Oral and Maxillofacial Surgery, where the fat lying anterior to the coronoid process, with the five extensions, can be easily transposed into the gap where you have operated under the condyle. Otherwise, you can use abdominal fat, which our research shows is much better than the buccal pad.
The question arises: how does fat prevent heterotopic bone formation in TMJ reconstruction? Wolford and his group have published largely in this area and say that number one, it prevents dead space, acting as a barrier between the temporal bone and the ramal stump. It has stem cells, and potential for lipogenesis, adipogenesis, and angiogenesis of the adjacent lipocytes. So, it induces the adjacent lipocytes to form more fat there, and the pluripotent cells prevent the heterotopic bone formation, preventing fibrosis and calcification. Above all, fat acts as a lubricant and improves the range of motion.
Shorter cartilage grafts reduce the risk of overgrowth
Next, let’s consider the classic method of the costochondral graft in TMJ reconstruction. The rationale for this approach is its physiological compatibility to the temporomandibular joint. It maintains ramus height, has growth potential, and acts as an interpositional barrier for the reduction of re-ankylosis and/or heterotopic bone formation.
We have achieved many good results and growth with this method, but a lot of controversies herald the CCG. The growth pattern of the graft is extremely unpredictable, because ankylosis is a common problem.
What are the potential reasons for overgrowth? Kagan says it is the wrong technique when people use rib for the costochondral graft. We also believe that may be true, but our own results suggest something else.
We have found that the length of the cartilage is directly responsible for the growth capacity of the CCG. If you keep it more than four millimeters long, you will find there is more overgrowth and a lot of movement. This causes ankylosis. Kaban advocated using one or two millimeters of cartilage cap. However, we use about two to four millimeters and have seen adequate results with that, and no or very few cases of overgrowth.
Reitzik suggests in his paper, that cortex to cortex healing after mandibular osteotomy takes 25 weeks in a man for the graft to totally integrate to the host point. So why do fixation seven days postoperatively? What does it really help?
Our strategy has changed now. We use a washer and the screw, and we don't really do the intermaxillary fixation for seven to 10 days. It suggests that if you keep doing physiotherapy immediately postoperatively, that will cause some kind of micro-motion that could cause the graft to break or fail. That is the reason for shorter cartilage grafts.
Costochondral grafts deliver better growth outcomes
Another controversy is whether the costochondral graft can be used in a case which has been previously operated. In our experience integration does not happen in those cases, so CCG in recurrent cases is a pitfall, because it contains more of cortical and less of cancellous bone, and the graft relies on local soft tissues for incorporation at the donor site.
It becomes evident that restoration of function will not cause growth, as told by Moss in his functional matrix theory. So. there is more than enough reason for us to believe that the functional matrix and growth center transplantation are required to work in tandem. Growth is one of the major goals of reconstruction.
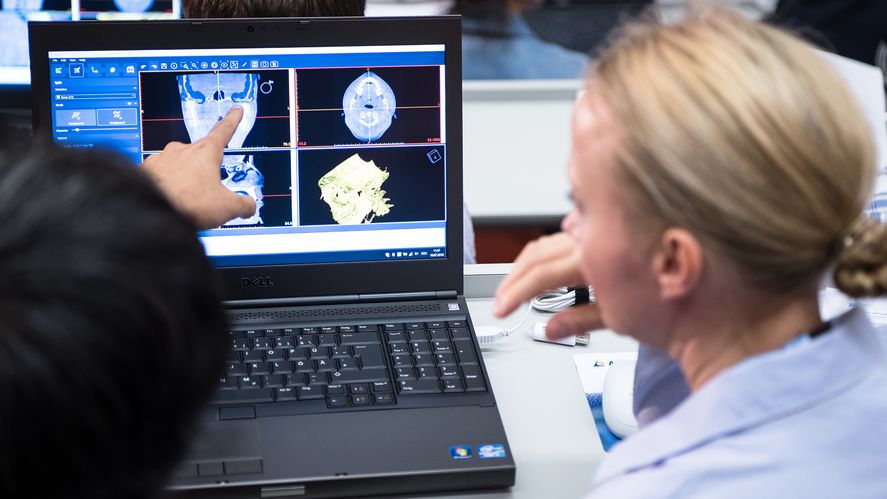
If we look at the literature we find a systematic review, and it suggests there are no randomized control trials on the growth potential of costochondral grafts in temporomandibular joint surgery. The only evidence is from case studies, so it was concluded that the use of CCG lacks scientific evidence.
However, personal experience in ankylosis or TMJ reconstruction suggests they have growth potential but can be unpredictable. We are continuing our randomized control trial, which was supported by the Indian Council of Medical Research, and we published in the Journal of Oral Maxillofacial Surgery in December 2021.
We saw that the growth outcomes and jaw functions were better in patients who have undergone a costochondral graft than the patients who have not undergone a costochondral graft. We found that the costochondral reconstructive osteoplasty in pediatric patients has a better outcome, in terms of growth of the mandible, improvement of the lower facial height, chin deviation, and facial asymmetry and occlusal tilt. The finding supports our hypothesis that the superiority of costochondral graft in pediatric TMJ reconstructions.
Furthermore, we examined whether costochondral grafts fulfill the ramus-condyle unit reconstruction goals in children with temporomandibular joint ankylosis, and we found that yes, it plays a significant role in the treatment of TMJ ankylosis in children, or TMJ reconstructions in children.
We found that 55% of our patients had optimal growth, 41% had suboptimal growth and 4% had overgrowth. The important fact is that 96% were showing some kind of growth. That is good enough for me because these patients, once they are mature, can be managed through other maxillary surgery.
Translating adult treatments to pediatric reconstructions
The pearls we might take from these cases is that you need fat grafting to reduce the extra heterotopic bone formation. The cartilage graft should be one to four millimeters, and then you do a decortication, and you do postoperative physiotherapy. And follow up is very important, because immediate intervention can be undertaken in the case of heterotopic bone formation or overgrowth.
The other factor is the transport disc distraction osteogenesis. That is, you use the distraction osteogenesis to make a neocondyle. One millimeter a day, the transport disc gets covered with fibrocartilage. In our cases we have seen a decreased overbite, showing that the mandible is growing because the cartilage of the neocondyle is helping it. However, one disadvantage is that you need to go in again and explant the distractor which you have placed. We tried using external distractors, and that also gave us good results.
Next, we looked into how the transport distraction osteogenesis compares with the costochondral graft in terms of ramus-condyle unit reconstruction. The answer, is that it really does. We found equal success in both ramus-condyle unit reconstruction with costochondral graft, and the transport distraction osteogenesis. However, these are very, very preliminary results, and future research is needed in these patients.
One big advantage is that this can be used in children and adults too. It allows for restoration of the ramal height, there is no donor site morbidity, fibrocartilage covering simulates the natural condyle. There are also minimal long-term changes in the height.
The disadvantage is that it requires two incisions and repeat surgeries for device removal. It also requires patient cooperation for daily activation, and the consolidation period can range up to 12 weeks.
Of course, adult ankylosis or adult TMJ ankylosis requires a total joint replacement for its treatment. Can this treatment be translated into pediatric reconstructions? We don’t know that yet. Orthopedic literature shows some excellent long-term results. Wroblewski in his Charnkey’s low friction hip replacements in teenage boys produced a wonderful long-term result. SK Velde also found that a total hip replacement in patients under 16 had excellent results, but he has expressed that a longer follow up is needed to measure longevity.
Looking at whether orthopedic experience be translated into TMJ surgery, the problems are graft failure, unpredictable growth, ankylosis and potential donor site morbidity. We can think about using the alloplastic TMJ in these growing children. However, the rationale is to continue to re-operate with the failed or overgrown or ankylosed costochondral graft, with either bony or soft tissue replacements, or both. Using the same modality again and again and thinking that you will get different kinds of results, seems very myopic.
Emerging research shows potential of costochondral grafts for children
However, on the other hand, orthopedic experience has shown that there are good results when alloplastic replacements are used in children or growing patients. So why not use it in total joint replacements in the growing children in the TMJ area as well?
In terms of feasibility, this technique can be used in high inflammatory TMJ disease, recurrent fibrosis or bony ankylosis, failed tissue grafts, loss of vertical mandibular height, or occlusion relationship.
However, there are a great many concerns. What is the effect on the growth? Would it require additional surgery? What is the potential lifespan of these devices? I feel that these patients are better off undergoing alloplastic TMJ/TGR, knowing that depending on the growth, revision of the replacement surgery would be required in future. And if we continue to operate them with the failures of costochondral graft or the soft tissue grafts, then they would as such undergo many surgeries till the time they mature.
So, we investigate the literature and find a pilot survey of surgeons by Keyser, Banda, Mercuri, Warburton, and Sullivan. Looking at a study of 14 patients aged seven to 17, they found encouraging results suggesting that total joint replacement surgery may be a viable option.
Another big study recently came from Douglas Sinn and Paul Tiwana’s group, looking at alloplastic TMJ reconstruction in five patients with severe ankylosis aged under 16. The follow-up range was huge, up to 221 months. In one case they operated on a seven-year-old and followed up seven years later, and subjectively recorded that some kind of growth was happening. In both this case and Dr Sinn’s, the overjet was increasing.
But compared to the costochondral graft, which we published in 2021, the overjet is actually decreasing. The mandible is definitely growing. What will happen when these children mature? I speculate that either I will have to replace or do a revision surgery for the ramus component, or I have to do a revision surgery for fossa and ramus component both, or I may have to do a conventional orthognathic surgery for the asymmetry and maxillary cant, which may not get corrected in these patients.
My take home message is that growth considerations make costochondral graft the logical choice for reconstruction of TMJ in children.
About the author:
Ajoy Roychoudhury, MDS, FDSRCPS, specializes in oral and maxillofacial surgery, and he is currently the head and associate professor at the Department of Oral and Maxillofacial Surgery at the All India Institutes of Medical Sciences, a leading unit in India to perform total TMJ replacements. Roychoudhury deals with the entire spectrum of oral and Maxillofacial surgery from exidingia to cranial base surgery including trauma orthognathic TMJ and mandibular reconstruction post pathology. His research interests include Temporomandibular Joint Ankylosis, Maxillofacial Trauma, Distraction Osteogenesis, Maxillofacial Tumors, and Trigeminal Neuralgia.
References and further reading:
- Agarwal B, Yadav P, Roychoudhury A, Bhutia O, Goswami D, Shukla G. Does Bilateral Gap Arthroplasty Increase the Severity of Obstructive Sleep Apnea in Patients With Temporomandibular Joint Ankylosis? J Oral Maxillofac Surg. 2021 Jun;79(6):1344.e1-1344.e11. doi: 10.1016/j.joms.2021.01.015. Epub 2021 Jan 22. PMID: 33609445.
- Gagnani SP, Agarwal B, Bhutia O, Roychoudhury A. New method of harvesting a buccal fat pad for interposition after gap arthroplasty of the temporomandibular joint. Br J Oral Maxillofac Surg. 2016 May;54(4):469-70. doi: 10.1016/j.bjoms.2015.09.004. Epub 2015 Sep 26. PMID: 26395214.
- Keyser BR, Banda AK, Mercuri LG, Warburton G, Sullivan SM. Alloplastic total temporomandibular joint replacement in skeletally immature patients: a pilot survey. Int J Oral Maxillofac Surg. 2020 Sep;49(9):1202-1209. doi: 10.1016/j.ijom.2020.02.001. Epub 2020 Feb 26. PMID: 32113746.
- Reitzik M. Cortex-to-cortex healing after mandibular osteotomy. J Oral Maxillofac Surg. 1983 Oct;41(10):658-63. doi: 10.1016/0278-2391(83)90020-4. PMID: 6578308.
- Roychoudhury A, Yadav P, Bhutia O, Kaur K, Dekyi T, Pandey RM. Growth Outcome and Jaw Functions Are Better After Gap Arthroplasty Plus Costochondral Graft Reconstruction Than Gap Arthroplasty Alone in Pediatric Temporomandibular Joint Ankylosis Patients: A Cluster Randomized Controlled Trial. J Oral Maxillofac Surg. 2021 Dec;79(12):2548-2561. doi: 10.1016/j.joms.2021.08.164. Epub 2021 Aug 30. PMID: 34592135.
- Sinn DP, Tandon R, Tiwana PS. Can Alloplastic Total Temporomandibular Joint Reconstruction be Used in the Growing Patient? A Preliminary Report. J Oral Maxillofac Surg. 2021 Nov;79(11):2267.e1-2267.e16. doi: 10.1016/j.joms.2021.06.022. Epub 2021 Jun 23. PMID: 34339614.
- Van de Velde SK, Loh B, Donnan L. Total hip arthroplasty in patients 16 years of age or younger. J Child Orthop. 2017 Dec 1;11(6):428-433. doi: 10.1302/1863-2548.11.170085. PMID: 29263754; PMCID: PMC5725768.
- Wroblewski BM, Purbach B, Siney PD, Fleming PA. Charnley low-friction arthroplasty in teenage patients: the ultimate challenge. J Bone Joint Surg Br. 2010 Apr;92(4):486-8. doi: 10.1302/0301-620X.92B4.23477. PMID: 20357322.
You may alsobe interested in:
AO CMF Study Clubs
AO CMF Study Clubs is where you connect with like-minded peers in your region.
AO Videos
Discover the full collection of expert presentations and other educational videos by AO CMF's world-renowned faculty.
From the AO CMF Blog
How a simple drug transformed the future of three young ameloblastoma patients.