CT criteria for Posterior Ligamentous Complex (PLC) injuries—insights from a multi-center study
BY DR MOHAMED ALY
CT scans have generally been considered to have limited accuracy and reliability when it comes to assessing PLC integrity, with reports suggesting it can fail to detect up to 17% of PLC injuries. However, recent studies have refined the approach to CT-based PLC assessment with the aim of enhancing diagnostic accuracy and improving clinical decision-making.
Multicenter External Validation of the Accuracy of Computed Tomography Criteria for Detecting Thoracolumbar Posterior Ligamentous Complex Injury. Neurosurgery, December 5, 2024. DOI: 10.1227/neu.0000000000003263
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
The posterior ligamentous complex (PLC) plays a crucial role in spinal stability, as recognized by both the Thoracolumbar Injury Classification and Severity Score (TLICS) and the AO Spine classification.1,2 However, assessing PLC integrity remains a challenge. Magnetic Resonance Imaging (MRI) is considered the gold standard due to its ability to directly visualize ligamentous structures with high sensitivity. Still, it is not always available in trauma settings worldwide, which can delay the timely management of spinal fractures or associated injuries. Furthermore, MRI takes longer scanning times and is more expensive.
Computed Tomography (CT) is more accessible and widely used, but it has its own limitations. Studies indicate that CT alone may overlook up to 17% of PLC injuries, potentially leading to delayed back pain or kyphosis. 3Therefore, enhancing the accuracy of CT-based assessment is essential to minimize reliance on MRI and improve decision-making in urgent trauma care.
Challenges in using CT for PLC injury detection
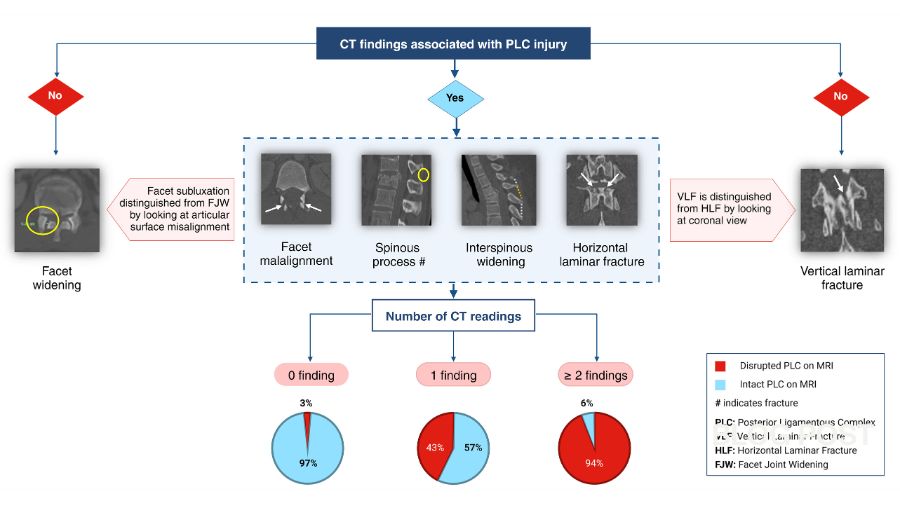
CT indirectly identifies PLC injuries by detecting signs of posterior element injury, including interspinous widening, spinous process fractures, laminar fractures, and facet diastasis. However, these findings are present in various morphological types or combinations that can make interpretation complex. For example, facet diastasis can manifest as dislocation, subluxation, fracture, or simple widening. 4
Traditionally, PLC status on CT has been classified as either intact (when no signs are present) or disrupted (if at least one sign is present). However, this binary approach has demonstrated only 50–70% accuracy since it does not consider the varying diagnostic significance of different findings or indeed a combination of such findings. Additionally, the lack of a standardized interpretation protocol has contributed to inconsistent reliability.
In our early research, we decided to evaluate the diagnostic accuracy of combined CT findings.5 To do this, we compared CT findings on PLC injuries with those of MRI on the same injuries. We discovered that there were several independent predictors of injuries identified by CT. These were:
- Interspinous widening >4 mm
- Spinous process fractures
- Horizontal laminar fractures
- Facet malalignment
Conversely, we found that facet joint widening and vertical laminar fractures were not independent precursors. We then evaluated the diagnostic accuracy of a combination of the four independent predictors outlined above and discovered some interesting conclusions:
- 0 positive findings: This indicated a low probability (9%) of PLC injury, suggesting an intact PLC (A-type injury).
- 1 positive finding: This suggested an intermediate probability (31%), indicating a possible indeterminate PLC injury (M1 modifier).
- 2 or more positive findings: This signaled a high probability of injury, suggesting PLC disruption (B-type injury), where surgical intervention is often warranted.
To improve accuracy, we also proposed a structured approach to differentiate PLC-related findings from their mimics, such as distinguishing horizontal versus vertical laminar fractures and facet subluxation versus facet joint widening.4
Multicenter validation of CT criteria
These findings were hugely important, and to validate them further, we recently conducted a multicenter study incorporating 614 patients across three Level 1 trauma centers—two in Saudi Arabia and one in Spain. Patients underwent both CT and MRI within 10 days of injury, and the results were published in Neurosurgery.6 In short, the findings reinforced our previous conclusions:
- The presence of ≥2 positive CT findings reliably indicated PLC injury (B-type injury).
- The absence of positive findings reliably ruled out PLC injury (A-type injury).
- A single CT finding suggested intermediate risk, supporting its use as an M1 modifier to determine the need for further imaging or observation.
This study stands out due to its large sample size and robust methodology, both of which enhance the precision and reliability of its conclusions, and it has important clinical implications for CT-based PLC assessment.
Firstly, it will strongly facilitate decision-making in trauma centers worldwide, particularly in resource-limited settings where MRI is either unavailable, contraindicated (e.g., pacemakers), or can’t be done in a timely fashion due to emergency surgery. These new CT-based criteria provide a reliable alternative for identifying B-type injuries requiring surgery. But even in well-equipped centers, such criteria can reduce unnecessary MRI scans, thereby lowering costs and minimizing delays in treatment.
Previously, the TLICS and AO Spine used the "indeterminate PLC" category, also known as the M1 modifier, to address uncertainty in diagnosing PLC injuries. For patients with neurologically intact burst fractures, the M1 modifier would place treatment recommendations in a so-called “grey zone," making decisions more dependent on a surgeon’s judgment. The M1 modifier is commonly overused as a middle ground option in light of uncertainty about PLC status.
Using a single CT scan finding as a criterion for the M1 modifier offers a more objective approach, reducing bias in treatment decisions. More importantly, the M1 modifier can help determine when further MRI testing is needed. If an MRI is unavailable, alternatives such as standing X-rays or close monitoring for kyphosis in non-surgical cases can be considered.
The cost-effectiveness of this approach is shown by the fact that only 15% of patients had a single CT finding; performing MRI for such a group will avoid 75% of missed PLC injuries on CT.
The usefulness of CT criteria can be further improved by considering their accuracy in different spinal regions, AO fracture classifications, neurological impairments, and unstable burst fractures. A machine learning algorithm is currently being developed to analyze all these factors and improve decision-making.
CT vs. MRI: Complementary tools in PLC evaluation
Rather than debate the merits of CT versus MRI, we believe both imaging methods should complement each other in guiding treatment decisions. Using CT and MRI together can improve the detection of PLC injuries while keeping costs and delays in treatment to a minimum.
Notably, interpreting MRI results for PLC injuries can be more challenging for spine surgeons than for neuroradiologists, but when two or more CT findings strongly suggest PLC injury, a detailed MRI review or a radiologist’s opinion may improve MRI accuracy.
Additionally, the significance of subtle MRI findings, such as an isolated and unclear supraspinous ligament injury, is still uncertain. In such cases, CT findings may help confirm or rule out instability. CT indicators of bone displacement, like interspinous widening, may provide more useful insights into instability than MRI findings alone in such case.
On the treatment side, there are a lot of controversies about when to consider surgery versus conservative management, short- versus long-segment instrumentation, minimally invasive versus open procedures, and posterior versus combined approaches. Most spine surgeons aim to establish clear treatment guidelines for managing burst fractures.
However, the first and most crucial step in addressing this issue is creating a reliable diagnostic process. Our validated CT criteria now provide an objective framework for addressing this diagnostic dilemma and represent the first step toward establishing clearer treatment guidelines.
Understanding PLC injuries
The Posterior Ligamentous Complex (PLC) is a crucial stabilizing structure of the spine. It consists of the supraspinous ligament, interspinous ligament, ligamentum flavum, and facet joint capsules. These structures work together to maintain spinal alignment and prevent excessive motion that could lead to instability or neurological injury. Injuries to the PLC are serious and often indicate significant spinal trauma, requiring careful assessment and management.
PLC injuries are commonly caused by high-energy trauma, such as vehicular accidents, falls from heights, and sports injuries.
Identifying PLC injuries is crucial but proper diagnosis can be challenging. MRI findings are sometimes subtle or open to misinterpretation. CT scans and X- rays may not adequately visualize the true extent of the damage, which can lead to delayed or inappropriate treatment. For example, in stable fractures, conservative management such as bracing may suffice, but with severe ligament disruption, surgical stabilization is usually required.
If PLC injuries are not properly managed, several complications can arise, including chronic pain, progressive spinal deformity. Therefore, PLC injuries are serious and often indicate significant spinal trauma, requiring prompt and accurate diagnosis.
About the author:
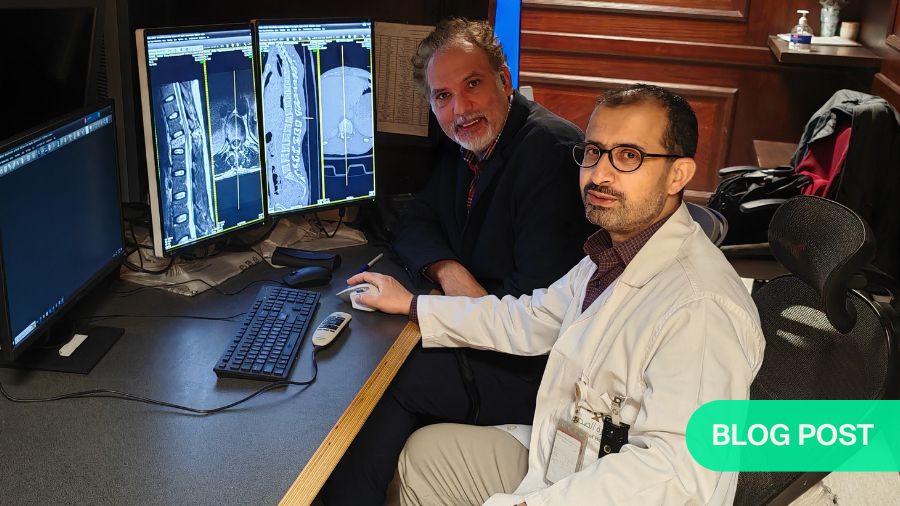
Dr Mohamed Aly is a fellowship-trained neurosurgeon and an associate professor at Mansoura University, Egypt. He serves as a neurosurgery consultant at Prince Mohamed Ben Abdelaziz Hospital, a Level 1 trauma center in Riyadh, Saudi Arabia. Aly holds a PhD in Neuroscience from Osaka University, Japan, and completed his residency at Mansoura University. He pursued further neurosurgical training through fellowships at the University of Calgary and the University of Colorado.
He is an associate member of the AO Spine Knowledge Forum Trauma and Infection and was recently elected as the Research Officer for the AO Spine Saudi Arabia Council. Additionally, he serves as Deputy Editor for the Advanced Spine Journal. Aly has authored around 50 peer-reviewed publications and several textbook chapters, presenting his research at national and international conferences. He has secured multiple research grants from AO Spine and other institutions, including funding for the study discussed in this article.
Acknowledgment
The author wishes to thank AO Spine for supporting the study. Interacting with AO Spine Knowledge Forum Trauma & Infection members during the last three years has added important insights to this work.
He also wishes to thank all co-authors contributing to this study from Prince Mohamed Ben AbdelAziz Hospital in Riyadh, King Saud Medical City, Riyadh, and Department of Neurosurgery, University Hospital Puerta de Hierro Majadahonda, Madrid, Spain for their invaluable contribution to the study. A full list of co-authors can be found in the paper published in Neurosurgery. Dr AbdulBaset Alshoaibi, a neuroradiologist from Prince Mohamed Bin Abdelaziz Hospital, is featured in the first picture and has a big contribution to the initial work as well as validation, especially for MRI analysis.
References and further reading:
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38(23):2028-2037. doi:10.1097/BRS.0b013e3182a8a381
- Vaccaro AR, Lehman RA, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: The importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30(20):2325-2333. doi:10.1097/01.brs.0000182986.43345.cb
- Aly MM, Soliman Y, Elemam RA, Pizones J, Alzahrani A, Elwatidy S. How frequently MRI modifies thoracolumbar fractures’ classification or decision-making? A systematic review and meta-analysis. European Spine Journal. 2024;33(4):1540-1549. doi:10.1007/s00586-023-08087-4
- Aly MM, Al-Shoaibi AM, Aljuzair AH, Issa TZ, Vaccaro AR. A Proposal for a Standardized Imaging Algorithm to Improve the Accuracy and Reliability for the Diagnosis of Thoracolumbar Posterior Ligamentous Complex Injury in Computed Tomography and Magnetic Resonance Imaging. Global Spine J. 2023;13(3):873-896. doi:10.1177/21925682221129220
- Aly MM, Al-Shoaibi AM, Alzahrani AJ, Al Fattani A. Analysis of the Combined Computed Tomography Findings Improves the Accuracy of Computed Tomography for Detecting Posterior Ligamentous Complex Injury of the Thoracolumbar Spine as Defined by Magnetic Resonance Imaging. World Neurosurg. 2021;151:e760-e770. doi:10.1016/j.wneu.2021.04.106
- Aly MM, Abdelaziz M, Alfaisal FA, et al. Multicenter External Validation of the Accuracy of Computed Tomography Criteria for Detecting Thoracolumbar Posterior Ligamentous Complex Injury. Neurosurgery. Published online December 5, 2024. doi:10.1227/neu.0000000000003263
You might also be interested in:
Global Spine Journal
Access the latest spine research evidence, submit your manuscripts, or become a reviewer for the GSJ.
Global Spine Congress
One of the largest spine meetings, bringing together thousands of spine surgeons from around the world.
AO Spine Knowledge Forums
Generating knowledge that matters to our members and to our patients.
AO Spine Guest Blog
Read about exciting developments and experiences from our global network.