Optimizing lower lumbar lordosis and pelvic tilt in high pelvic incidence
BY DR MARKUS LOIBL AND DR PEDRO BERJANO

Degenerative pathology of the lumbar spine remains one of the most frequent problems encountered in daily orthopedic and spine practice. Patients typically present with a combination of mechanical back pain, radicular symptoms, and, in more advanced stages, neurogenic claudication. While decompression and short-segment fusion have been established treatment strategies for decades, clinical experience and growing biomechanical understanding have challenged the idea that treating the “index level” alone is always sufficient.
-
Read the quick summary:
- Markus Loibl And Pedro Berjano discuss treatments for degenerative pathology, and explore the importance of looking beyond standard decompression and short-segment fusion.
- Treating stenosis alone may be insufficient; restoring L5–S1 lordosis and achieving solid fusion improves global alignment and reduces compensation.
- Surgeons can integrate pelvic incidence, pelvic tilt, and compensation patterns into short-segment surgical planning.
- Strong evidence linking alignment correction to long-term outcomes is still limited, and optimal techniques remain under ongoing debate.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Degenerative lumbar disease in the era of sagittal alignment
Over the last two decades, sagittal alignment—and particularly the relationship between the spine and the pelvis—has moved from being an academic concept to a central element of modern surgical planning. Parameters such as pelvic incidence, pelvic tilt, sacral slope, and lumbar lordosis are now routinely discussed not only in long deformity constructs but increasingly also in short-segment degenerative surgery. This has introduced both new opportunities and new challenges. For the practicing clinician, the key question is no longer only whether a segment is stenotic or unstable, but whether the overall biomechanical environment is being addressed adequately to ensure durable outcomes.
Our case discussion at the AO Davos Courses 2025 illustrated many of these challenges. Here we recap the discussion around the case and highlight how high pelvic incidence can fundamentally alter surgical decision-making, how compensation patterns influence segmental degeneration, and why restoration of lower lumbar lordosis may be as important as decompression itself.
Clinical presentation and prior conservative management
The patient in question is a 47-year-old veterinary surgeon working primarily with large animals, a profession associated with high physical loading of the lumbar spine. She had suffered from low-back pain for several years, with substantial worsening over the last four years. During the two years prior to presentation, she developed progressive neurogenic claudication, with a walking distance limited to 50–100 meters before needing to stop.
By the time she reached the tertiary referral center, extensive conservative treatment had already been attempted. This included epidural and radicular injections, long-term drug therapy, and more than one year of active physical therapy. Importantly, the conservative history was not documented superficially. The treating surgeon explored in detail what kind of injections were given, under what technical conditions, which rehabilitation protocols were used, and whether structured trunk stabilization exercises were truly performed and adhered to. This level of detail is essential in contemporary practice, where the indication for surgery increasingly depends on documented failure of adequate nonoperative treatment rather than on imaging alone.
From local pathology to global assessment
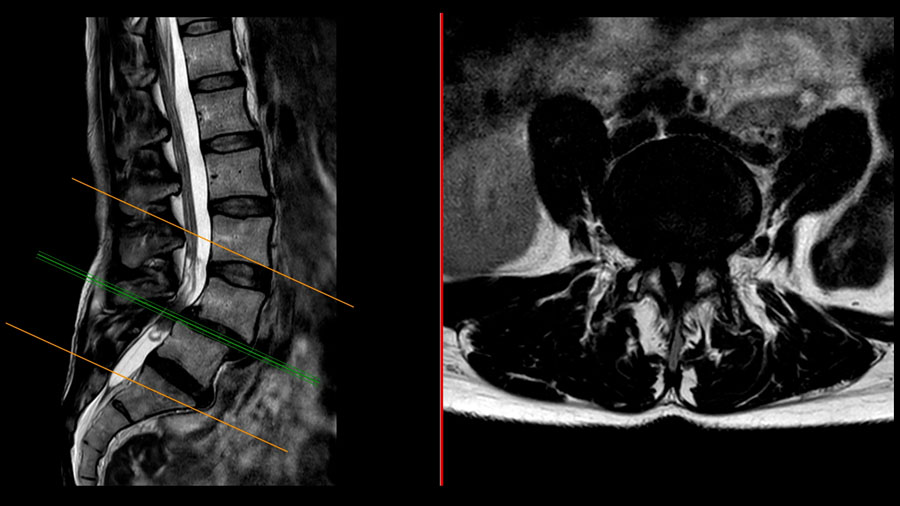
Standard radiographs demonstrated a degenerative spondylolisthesis at L4–5. Two decades ago, such a finding, especially when combined with correlating symptoms, would often have been enough to proceed directly to surgery, typically after confirming stenosis on MRI. Today, that approach is no longer considered sufficient for many patients.
Flexion–extension radiographs were obtained, not primarily to quantify motion at the index level, but to screen for potential instability at adjacent segments. While their utility remains controversial, they can occasionally reveal translation at levels not otherwise suspected.
More importantly, a full spine standing radiograph from C2 to the proximal femur was obtained in a standardized, relaxed position. This provided the basis for sagittal alignment analysis. Among all measured parameters, two stood out as particularly relevant:
- Pelvic incidence (PI), which reflects the intrinsic morphology of the pelvis and the magnitude of lumbar lordosis required for sagittal balance.
- Pelvic tilt (PT), which reflects the degree of pelvic retroversion and thus the amount of compensatory effort used by the patient to maintain an upright posture.
In this patient, the pelvic incidence measured approximately 75°, placing her at the very high end of the spectrum. High PI fundamentally increases the biomechanical demand on the lumbar spine.
When adequate lordosis is not present—particularly in the distal lumbar segments—multiple compensatory mechanisms are recruited.
Compensation patterns and their clinical meaning
Several compensatory strategies were evident:
- Pelvic retroversion, reflected by an increased pelvic tilt, indicating that the patient was rotating her pelvis posteriorly to compensate for the lack of lumbar lordosis.
- Hyperextension at L3–4, the disc above the spondylolisthesis, suggesting that adjacent segments were being driven into excessive motion to maintain global balance.
- Thoracic straightening and extension, with proximal migration of the kyphosis–lordosis inflection point to around T9–T10.
While these compensations allow the patient to remain upright, they come at a cost. Compensation requires continuous muscular activation. Over time, this contributes to fatigue, pain, and further mechanical overload of adjacent discs and facet joints. Although definitive proof that such compensation directly accelerates adjacent segment degeneration is limited, the clinical association is strong and familiar to most spine surgeons.
Concordance as a prerequisite for targeted treatment
A central concept emphasized in the discussion was concordance, i.e., the alignment between clinical symptoms, imaging findings, and functional impairment. In this case, concordance was clear. The patient’s dominant complaint was progressive neurogenic claudication, and MRI demonstrated central and lateral recess stenosis at L4–5. Supine MRI also showed partial reduction of the spondylolisthesis, highlighting the dynamic nature of the pathology.
Without such concordance, the probability of achieving meaningful symptom relief is reduced. Beyond radiographic correlation, concordance also extends to psychological readiness and the patient’s willingness to actively participate in postoperative recovery.
What exactly should be treated?
Once concordance is established, the next challenge is defining the true objective of surgery. If the goal is only to treat claudication, isolated decompression of the stenotic segment may be sufficient. However, if the goal is to address not only neural compression but also the underlying biomechanical dysfunction, then alignment must be considered.
Here lies one of the most difficult areas in contemporary degenerative spine surgery. While emerging data suggests that restoration of sagittal alignment is associated with improved long-term outcomes, the current evidence base is still incomplete. Surgeons are therefore required to integrate evolving biomechanical concepts without relying on definitive “gold-standard” data. This creates inevitable variability in practice.
In this case, the treating team chose to address not only the stenosis and instability at L4–5 but also the global sagittal imbalance, with particular focus on restoring lower lumbar lordosis.
The dilemma of the L5–S1 segment in high pelvic incidence
Although the primary symptomatic pathology was located at L4–5, the L5–S1 disc showed advanced degeneration with a “black disc” appearance on MRI and a complete loss of segmental lordosis. In a patient with such a high pelvic incidence, this finding became pivotal.
High pelvic incidence demands a large amount of lumbar lordosis to achieve sagittal balance. If the distal lumbar segments—especially L5–S1—fail to contribute sufficiently, the entire compensation chain is placed under strain. The decision was therefore made to include L5–S1 in the fusion construct.
This is one of the defining challenges for clinicians treating high PI patients. Limiting surgery to the symptomatic level may appear less invasive, but it risks leaving a mechanically unfavorable environment that could compromise long-term outcomes. On the other hand, extending fusion increases surgical magnitude. Striking the right balance is one of the most difficult judgments in daily practice.
Maximum effective surgery as a guiding principle
Rather than pursuing minimally invasive surgery, the strategy followed the principle of maximum effective surgery, a concept focused on achieving all essential surgical objectives with the least necessary extent. These objectives were clearly defined:
- Adequate neural decompression
- Reduction of spondylolisthesis
- Restoration of sagittal alignment, particularly lower lumbar lordosis
- Achievement of solid fusion
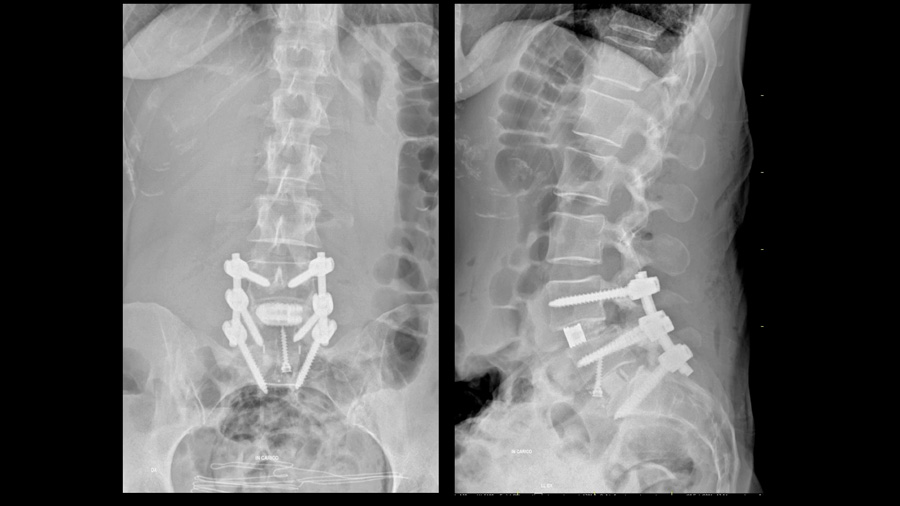
L5–S1 was treated with anterior lumbar interbody fusion (ALIF) to facilitate lordosis restoration. A 12-degree cage was used, with the acknowledgment that greater lordosis might have been achievable with a higher-angle implant. L4–5 was treated with posterior decompression and TLIF. Emphasis was placed on using a large, anteriorly positioned cage, posterior column osteotomy and compressing through the posterior column to maximize segmental lordosis.
A key message from the discussion was that the surgical goal matters more than the technique. Different surgeons may use different approaches—ALIF, TLIF, or other methods—but the biomechanical goal remains the same.
Effects beyond the fused segments
Postoperative imaging demonstrated restoration of alignment and stable fixation from L4 to S1. However, what was particularly striking was the effect on the non-fused segments:
- The compensatory hyperlordosis at L3–4 decreased.
- Thoracic extension was reduced.
- The inflection point between thoracic kyphosis and lumbar lordosis migrated caudally.
These indirect changes illustrate a key concept of modern alignment surgery: successful correction allows the spine to abandon compensation. Compensation, while initially protective, is ultimately exhausting and mechanically costly. Removing the need for compensation may be as important as correcting the index pathology itself.
Fusion challenges in high pelvic incidence
High pelvic incidence is typically associated with a steep sacral slope, which generates significant shear forces at the L5–S1 junction. This mechanical environment increases the risk of loosening and pseudarthrosis. In this patient, strategies to counteract these forces included bicortical S1 screws and a large-footprint interbody implant.
At 15-month follow-up, CT imaging confirmed a solid fusion. For the treating surgeon, this confirmation provided confidence in the durability of the result. In high PI patients, achieving reliable fusion is not an accessory goal; it is fundamental to the overall success of the operation.
Postoperative activity and counseling
After confirmation of solid fusion, the patient was allowed to return to unrestricted activities. Rather than imposing rigid limitations, the focus was placed on ergonomics and sensible load management. Deep squatting with heavy weights and improper lifting techniques were discouraged, but otherwise the patient was encouraged to live without major restrictions.
This reflects a pragmatic philosophy: modern constructs should allow patients to return to active lives, provided they understand how to protect their spine in daily activities.
Broader challenges for practicing clinicians
This case highlights several broader challenges that are increasingly relevant in daily clinical practice:
- High-demand, younger patients with degenerative disease
Expectations for long-term durability are rising, making biomechanical optimization more important than ever. - Integration of global alignment into short-segment surgery
Even “simple” cases may require complex alignment considerations. - Evidence gaps
While alignment is clearly important, definitive prospective data remain limited, forcing surgeons to rely on evolving clinical experience. - Variability in surgical strategies
Multiple techniques can achieve similar goals, but variability remains high. Reducing unwarranted variation without enforcing dogma is an ongoing challenge.
Take-home messages
Degenerative lumbar spine surgery is increasingly about understanding and correcting the mechanical environment in which those segments function, not only about decompressing nerves and stabilizing unstable segments. High pelvic incidence represents one of the clearest examples of how pelvic morphology can dictate spinal behavior, compensation patterns, and long-term surgical success.
We distilled several practical lessons from our discussion:
- Degenerative lumbar pathology should be evaluated in its global mechanical context.
- High pelvic incidence fundamentally changes surgical planning and risk assessment.
- Concordance between symptoms, imaging, and function is essential for predictable outcomes.
- Restoring lower lumbar lordosis—especially at L5–S1—may be critical in high PI patients.
- Solid fusion is non-negotiable in high-shear environments.
- Surgical success depends more on achieving the right biomechanical goals than on the specific technique chosen.
As this case illustrated, modern spine surgery requires technical execution and thoughtful biomechanical strategy. While much remains to be learned, the direction is clear: durable outcomes depend on addressing both the pain generator and the global alignment that shapes it.
About the authors:
Prof. Dr. med. Markus Loibl is Head of Spine Surgery at the Schulthess Klinik in Zürich, Switzerland.
Dr Loibl's surgical focus is primary and revision surgery of degenerative pathologies of the spine, from disc herniation and degeneration to adult spinal deformities and scoliosis. He has a clear focus on outcome research and adapting surgical strategies. Dr Loibl is the current AO Spine Europe and South Africa Education Officer.
Dr Pedro Berjano is an Orthopedic Spine Surgeon and Director of the GSpine4 Spine Surgery Division at the IRCCS Ospedale Galeazzi Sant'Ambrogio in Milan, Italy.
Dr Berjano's areas of expertise are minimally invasive spinal surgery and its application to scoliosis, adult deformity surgery, and anterior spinal surgery. He is considered by his colleagues to be one of the leading experts in minimally invasive lateral approach surgery, revision surgery and spinal deformity in adults. Dr Berjano is the current Past-Chairperson of AO Spine Europe and Southern Africa.
You might also be interested in...
Window on the AO Davos Courses
AO's video platform with exclusive interviews, live-streamed surgical simulations, case discussions, and insights from diverse surgeons from around the world.
AO Spine Courses and Events
Explore the upcoming courses, webinars or online events in your region and worldwide, or download a list of all upcoming events in your region in PDF format.
AO Spine Classification Systems
Download and start using the AO Spine Injury Classification System toolkits, including posters, handy pocket cards, and and short videos with experts explaining details.
AO videos and webinars
Explore AO's digital teaching and learning material, webinars, and event coverage for educational purposes.