Minimally invasive surgery in thoracolumbar fractures: shifting towards targeted, muscle-sparing stabilization
BY DR RATKO YURAC AND DR CHARLOTTE DANDURAND

Minimally invasive spine surgery (MISS) is redefining thoracolumbar fracture management by achieving outcomes comparable to open fusion with reduced morbidity. Surgeons can apply muscle-sparing fixation techniques for faster recovery and better patient value, while research continues into fusion needs, long-term outcomes, and advanced technologies.
Thoracolumbar trauma remains one of the most frequent and challenging entities in spinal surgery. Nearly 90% of high-energy injuries involve the spine, and around one quarter present neurological compromise.
Traditionally, unstable AO Type B and C fractures were managed with open posterior fusion to achieve rigid stabilization and canal decompression. However, the rise of minimally invasive spine surgery (MISS) has transformed this paradigm, offering comparable biomechanical results with substantially reduced morbidity.
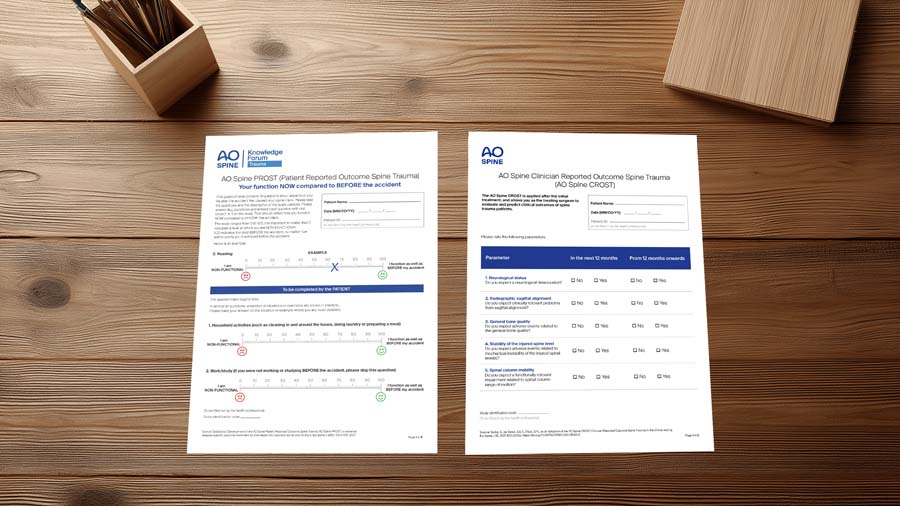
In parallel, the introduction of patient-reported outcome measures (PROMs) and cost-effectiveness analyses has positioned MISS within a broader value-based care framework, highlighting not only clinical equivalence but also potential economic advantages.
-
Read the quick summary:
- Spine experts review how minimally invasive surgery (MIS) is transforming thoracolumbar fracture management toward muscle-sparing stabilization.
- MIS offers outcomes equal to open surgery with less pain, blood loss, and morbidity, supporting value-based, patient-centered care.
- Surgeons can apply MIS for most thoracolumbar fractures, reducing complications and recovery time while maintaining biomechanical stability.
- Future advances include robotics, navigation, and AI to expand MIS indications and clarify long-term results and cost-effectiveness.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Despite these advances, key questions remain, particularly regarding need for fusion versus fixation, implant removal, long-term cost-effectiveness, and the feasibility of MIS for the most complex fracture types, notably with severe deformity.
Global highlights in MISS for thoracolumbar fractures
- Equivalent outcomes, less morbidity with MISS: Minimally invasive fixation achieves radiographic, functional, and neurological outcomes comparable to open surgery with significantly reduced blood loss, pain, and hospitalization with markedly reduced perioperative morbidity
- Percutaneous fixation without the use of arthrodesis does not influence clinical and radiographic outcomes in thoracolumbar burst fractures compared to the posterior open approach and fusion
- Expanded indications: MISS is increasingly validated for AO type A, as well as type B1 and B2 fractures. Ankylosed (B3) patterns are increasingly treated via MIS
- Hardware removal may be beneficial in a selected group of patients. The decision should be individualized based on fracture type, symptoms, function, and imaging evidence of fusion. In thoracolumbar burst fractures (A3/A4), there is evidence that hardware removal is beneficial and should be strongly considered
- Patient-centered value: Early PROMs and limited cost analyses at 1–2 years favor MIS in selected cases. Economic analyses favor MIS as a cost-effective alternative
- Emerging technologies—robotics, navigation, and augmented reality—will further expand MIS applications in complex thoracolumbar trauma
However, limitations still remain. Severe Type C injuries or high canal compromise may still require hybrid or open strategies despite advancing MIS tools. Future direction with integration of navigation, robotics, and AI-driven models promises further refinement and individualized spine-trauma management.
Where we currently stand with evidence, PROMs, and costs
Over the last decade, comparative studies and meta-analyses have consistently shown that MISS—particularly percutaneous pedicle screw fixation—provides radiological and functional outcomes comparable to those of open surgery, while significantly reducing operative time, blood loss, postoperative pain, and hospital stay (Afolabi 20191; Carazzo 20212).
In the 2024 meta-analysis by Esposito et al.3, the average Oswestry Disability Index and pain scores for the MIS group were numerically better, although the differences were not statistically significant, reinforcing the safety and and non-inferiority of MIS approaches in thoracolumbar trauma.
A recent retrospective series applying MIS techniques even to high-grade thoracolumbar injuries (average TLICS ≈7.5) documented PROMs (ODI, SF-12) at around 600 days of follow-up with acceptable functional results and minimal blood loss (~119 mL) in experienced hands.
From a cost perspective, a comparative Spanish study of MIS versus open surgery in thoracolumbar fractures found that, although MIS reduced hospital stays and blood bank resource use, total direct hospital costs were not significantly different.
However, the pattern of resource savings in perioperative care indicates that MIS has potential for value-based application, especially when considering PROM improvements, faster recovery, and lower complication rates. Hardware removal has been shown to be cost-effective in thoracolumbar burst fractures through postoperative year 2.
Advances in MISS for PLC-injured fractures (B2/B3)
Historically, surgeons favored open fusion for AO Type B2 fractures with posterior ligamentous complex (PLC) disruption. However, emerging data suggest that, when reduction and fixation are adequate, percutaneous instrumentation without fusion can achieve similar alignment and complication rates. Short-segment constructs enhanced with an intermediate screw at the fractured vertebra (SSPF + IS) improve stiffness and radiographic correction without compromising mobility.
Hybrid strategies that combine percutaneous fixation with limited fusion can be considered in certain situations, notably when traumatic disk injury, severe deformity or anterior column compromise are present. In cases with neurological compression, minimally invasive decompression techniques—using tubular or lateral corridors—can be safely added in selected cases, maintaining much of the minimally invasive (MIS) approach.
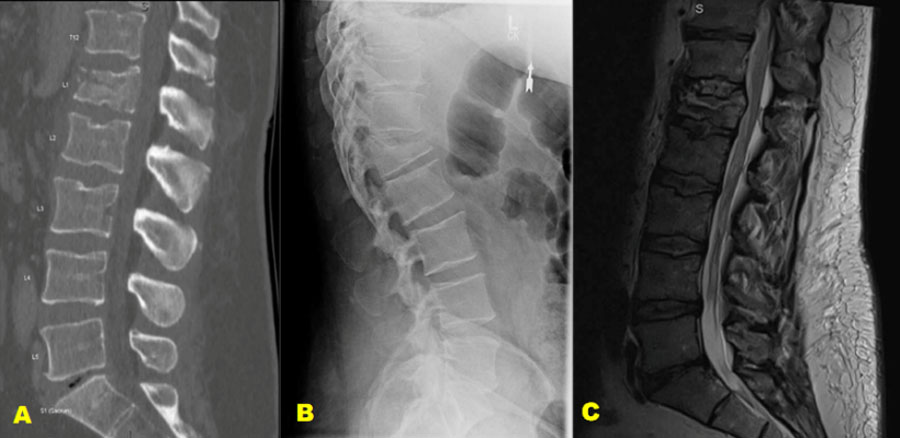
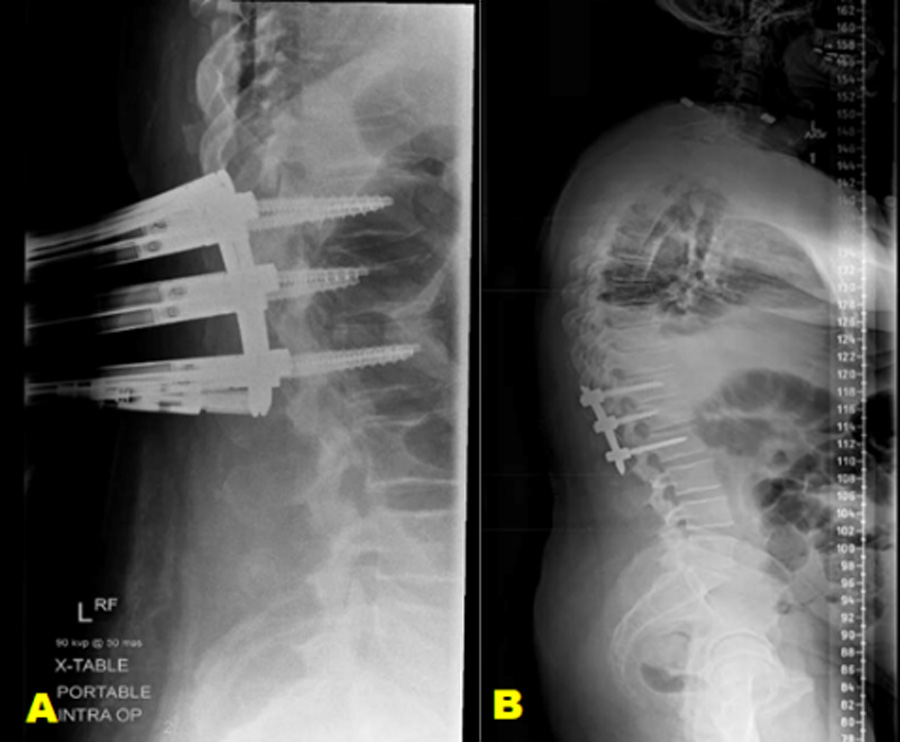
Example case 1: neurologically intact patient
A 45-year-old male who was involved in a motor accident and was ejected from the vehicle. The patient was neurologically intact.
MIS in ankylosed spines (B3)
Fractures in ankylosed spines (e.g., DISH, ankylosing spondylitis) act as long lever arms and are prone to hyperextension or distraction injury. Open surgery in this group carries high perioperative risks, including bleeding, pulmonary complications, and longer recovery times.
Several comparative studies now show that minimally invasive spine surgery (MISS) significantly reduces operative time, blood loss, and hospital stay, while providing comparable alignment and neurological outcomes.
Long percutaneous constructs—spanning three levels above and below the fracture—are recommended; in some cases, iliac fixation may be necessary at the lumbosacral junction.
Damage-Control Spine Surgery and MIS
In polytrauma or physiologically unstable patients, Damage-Control Spine Surgery focuses on rapid, low-impact stabilization to allow systemic recovery before definitive fusion. In this context, MISS is ideal: percutaneous fixation offers immediate mechanical stability with minimal physiological stress, enabling early mobilization and better lung function. Once the patient stabilizes, staged extension or fusion can be performed if necessary.
The emerging AO consensus (AO Damage Control 2.0) aims to establish thresholds—both physiologic and biomechanical—where MISS may serve as both a temporary and permanent stabilization option in thoracolumbar trauma.
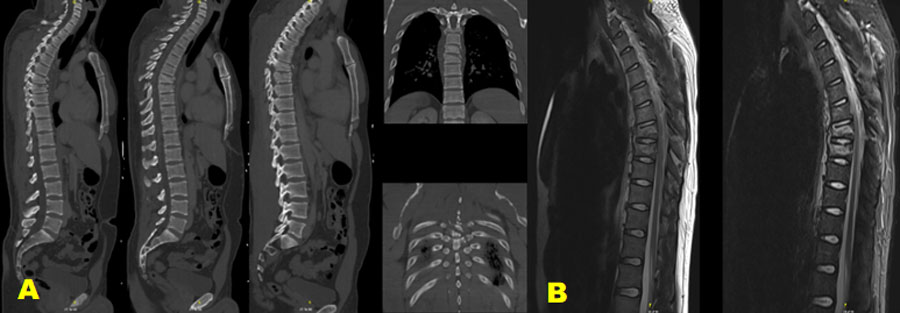
Example case 2: neurologically intact patient
A 28-year-old male patient has a history of recurrent dislocation of the right shoulder, for which he underwent surgery three years ago. He was involved in a traffic accident, colliding with a car while riding his motorcycle and being thrown from it.
Severe pain in his back and left forefoot, as well as deformity and functional weakness in his right shoulder. The patient was neurologically intact and experienced temporary loss of consciousness.
Adjunct techniques, implant removal, and long-term considerations
Modern MIS algorithms also incorporate cement augmentation and expandable implants in selected traumatic compression fractures with anterior column compromise. Kyphoplasty and intravertebral devices can provide quick pain relief and restore vertebral height, although their use is selective in trauma cases.
Routine hardware removal after MIS stabilization may be beneficial in selected groups of patients. A 2024 meta-analysis of implant removal versus retention in thoracolumbar burst fractures concluded that planned removal in younger patients may enhance functional scores but carries risks of deformity recurrence and reoperation complications; removal should be tailored to each case.
In symptomatic patients, early (<12 months) removal often relates to better recovery of the segmental range of motion, though the evidence is inconsistent. Percutaneous removal has proven to be a safe, minimally invasive option in certain series. Long-term data confirm the durability of posterior constructs in open surgery; by extension, the durability of MIS is promising but lacks extensive follow-up over a decade or more. Cost-effectiveness over time remains plausible, considering lower costs associated with infection, reoperation, and recovery.
Limits, challenges, and future directions
The scope of MIS is expanding: Endoscopic or tubular decompression combined with percutaneous fixation has been effectively used in selected cases of neurological injury (burst/compression) with outcomes similar to open surgery in specialized centers (Camacho 2019).
However, for high-grade translational (Type C) injuries, severe disc or ligament disruption, or cases with canal compromise that require extensive decompression or vertebrectomy, there is limited evidence. Many of these still require hybrid or open surgical approaches, tailored to the patient's anatomy, the surgeon's expertise, and neural element preservation.
AO Guidelines for Acute Spinal Cord Injury highlight the importance of individualized planning rather than applying MIS universally. In the future, the incorporation of 3D navigation, robot-assisted instrumentation, AI-driven planning, and real-time biomechanical feedback could further advance MIS, even in complex trauma cases.
Growing evidence supports MIS in most cases
The evolution of minimally invasive techniques in thoracolumbar trauma represents a shift from extensive exposures to targeted, muscle-sparing stabilization. Growing evidence now supports MIS as the standard for fractures with healing potential and as a feasible option for more complex instability patterns. Implant removal may be beneficial in appropriately selected cases.
Early PROMs and limited cost data at 1–2 years show promising indicators for MIS value.
However, not every case—especially severe translational or neurologically complex fractures—can be managed solely with MIS at this time. As navigation, robotics, and predictive modeling advance, the scope of MIS in spinal trauma will continue to grow, striving for wider use without sacrificing safety or outcomes.
About the authors:
Dr Dandurand’s research interests concentrate on spinal trauma research and clinical outcomes of spine surgery. She is an associate member of AO Spine Knowledge Forum Trauma, an international multi-disciplinary panel of experts pursuing innovative research into spinal trauma. She is also an active member of the Canadian Spine Society and North American Spine Society.
References and further reading:
- Afolabi A et al. Comparison of percutaneous minimally invasive versus open posterior spine surgery for fixation of thoracolumbar fractures. J Orthop. 2019;18:185–190.
- Carazzo M et al. Minimally invasive versus open posterior stabilization for thoracolumbar fractures: a systematic review and meta-analysis. Int J Spine Surg. 2021;15(5):973–985.
- Esposito M et al. Minimally invasive stabilization of thoracolumbar trauma: evidence update and cost analysis. Global Spine J. 2024;14(2):240–251.
- Saravi B et al. One-Year Clinical Outcomes of Minimally Invasive Dorsal Percutaneous Fixation. Medicina. 2022;58(5):606.
- Panero E et al. Cost Difference Between Open Surgery and Minimally Invasive Surgery for Thoracolumbar Fractures (Spain cohort). Spine. 2024.
- Diniz JM, Botelho RV. Is fusion necessary for thoracolumbar burst fracture treated with spinal fixation? A systematic review and meta-analysis. J Neurosurg Spine. 2017;27(5):584-592. doi:10.3171/2017.1.SPINE161014
- Chou PH, Ma HL, Wang ST, Liu CL, Chang MC, Yu WK. Fusion may not be a necessary procedure for surgically treated burst fractures of the thoracolumbar and lumbar spines: a follow-up of at least ten years. J Bone Joint Surg Am. 2014;96(20):1724-1731. doi:10.2106/JBJS.M.01486
- Wang Y et al. Is It Necessary to Remove Implants After Fixation of Thoracolumbar Trauma? J Clin Med. 2023;12(6):2213.
- Han-Dong Lee 1, Chang-Hoon Jeon, Nam-Su Chung, Young-Wook Seo. Cost-Utility Analysis of Pedicle Screw Removal After Successful Posterior Instrumented Fusion in Thoracolumbar Burst Fractures. Spine (Phila Pa 1976). 2017 Aug 1;42(15):E926-E932.
- Camacho JE et al. The use of minimally invasive surgery in spine trauma: concepts, limitations, applications. J Spine Surg. 2019;5(4):4556.
- Yang H et al. Endoscopic decompression and fixation for thoracolumbar burst fractures: outcomes in 62 patients. Eur Spine J. 2023;32(8):1641–1655.
- Deng J et al. Percutaneous reduction systems for multi-planar thoracolumbar fractures. Global Spine J. 2024;14(3):411–422.
- Li X et al. MIS fixation for incomplete spinal cord injury: comparative results. Neurosurg Rev. 2021;44(6):3327–3338.
- AO Spine Knowledge Forum Trauma. AO Damage Control Spine Surgery 2.0 – Consensus Initiative. AO Spine Reports. 2024.
Thanks to AO Spine KF Trauma and Infection Group for their support and ongoing efforts to bridge knowledge gaps in the management of patients with trauma and spinal infections worldwide!
You might also be interested in...
AO Spine Classification Systems
The AO Spine Thoracolumbar and Subaxial Injury Classification systems are the result of a systematic assessment and revision of the Magerl classification.
Knowledge Forum Trauma and Infection
Leading the globe in generating the knowledge that improves patient care after suffering from spine trauma and infection.
AO Surgery Reference
AO Surgery Reference is a resource for the management of fractures, based on current clinical principles, practices and available evidence.
Minimally Invasive Spine Surgery (MISS)
Educational material and courses covering all types of minimally invasive spine operations through tubular/microscopic, endoscopic, and instrumented procedures.