Pre-psoas approach—a true game changer in Adult Spinal Deformities
BY DR JACOB YOONG LEONG OH AND DR GUNA PRATHEEP KALANCHIAM
The prevalence of Adult Spinal Deformity (ASD) is on the rise, primarily because of the advancements in health care contributing to the increased life expectancy of the aging population. To date, ASD is one of the challenging conditions to treat owing to the varied symptomatology, lack of universally accepted standard guidelines in management, and associated comorbidities in the affected population. Interbody fusion is one of the important workhorses in managing these deformities. And especially, most of the literature on ASD management is based on posterior surgical strategies.
However, the extensive dissection of the erector spinae musculature in this patient subgroup already vulnerable to sarcopenia among others poses concerns in the recovery and associated post-operative rehabilitation. While, several researchers emphasized an alternate lateral approach, the injury to the lumbar plexus is quite a significant complication while performing this trans-psoas approach.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Could ASD correction be less morbid?
The late 90s paved the way for a new oblique corridor when Michael Mayer described the pre-psoas approach. Its ingress to the disc space is what makes this approach quite exciting. It neither strips off the muscular band as in a posterior approach nor encounters the abdominal contents, greater vessels, or nerve plexus as in anterior/ lateral interbody fusion. The pre-psoas approach provides a retroperitoneal minimally invasive access to the lumbar spine, eliminating the possible morbidity of other approaches.
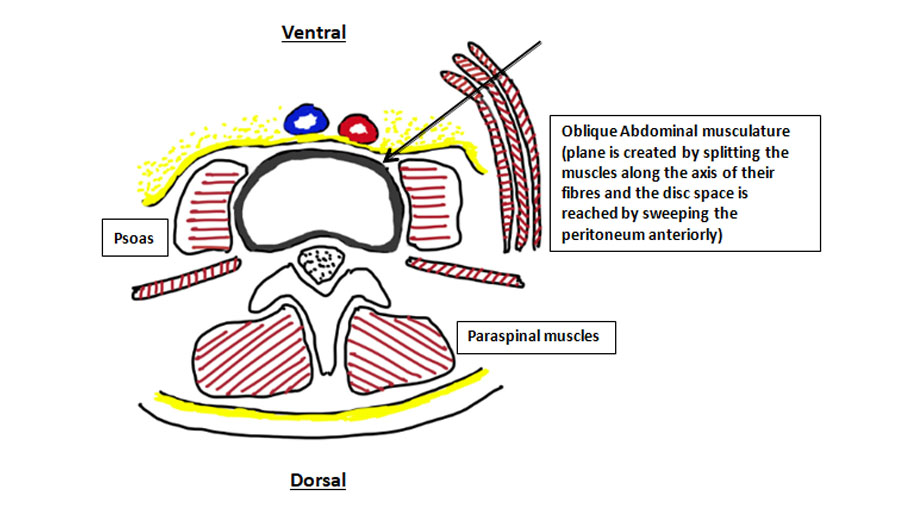
The surgery is performed usually with the patient in the right lateral position, and the approach is from the left side. Skin incision is over the anterolateral aspect of the anterior abdominal wall and the dissection is carried out by splitting the fibers of the oblique (external and internal) and transversus abdominis muscles. Throughout the procedure, muscles are not cut, but only separated along the direction of their muscle fibers. The peritoneum is swept anteriorly by finger dissection and the plane is posterolateral to the great vessels. The Psoas tendon is visualized and retracted posteriorly, thereby reaching the intended disc space.
Using the pre-psoas approach, a larger footprint interbody cage can be placed spanning across the vertebral rim resulting in ‘indirect decompression’ of the neural canal and restoration of foraminal height. Thus, the goals of decompression are achieved without a laminectomy or a foraminoplasty. This helps reduce the risks of dural tear, nerve root injury, and CSF leaks observed with direct decompression.
What are the possible benefits of the pre-psoas approach in ASD?
Minimally invasive surgical corridor
The Pre-psoas approach is truly a minimally invasive (MIS) approach in every sense. Apart from the lesser surgical invasiveness and retroperitoneal approach, there is minimal blood loss even when exposing multiple levels.
Coronal Cobb’s correction
It is well known that, degenerative lumbar deformities are often associated with coronal translation of the vertebral body and asymmetric disc space collapse. This malalignment is better suited for correction on the same plane as the deformity. This is one of the important advantages of the pre-psoas corridor as it helps to effectively correct the asymmetric disc space collapse, coronal obliquity, and lateral vertebral translation and improves the overall C7-CSVL balance.
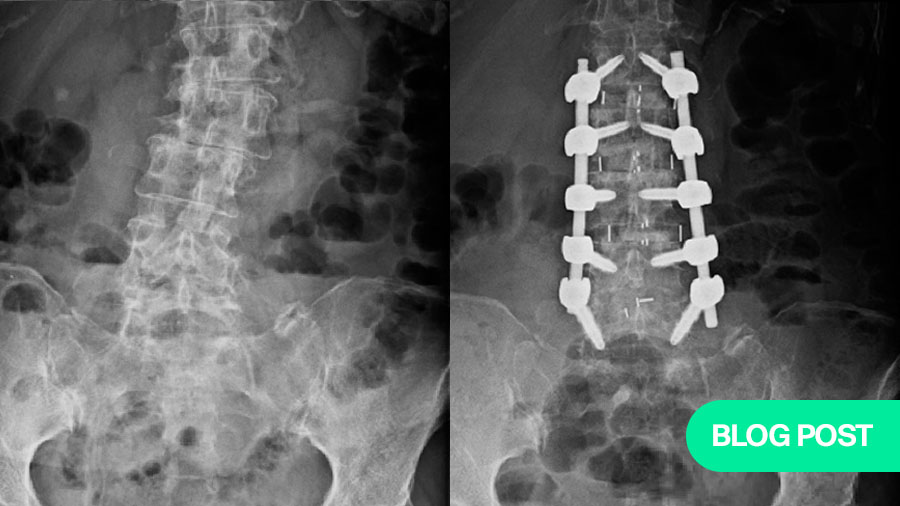
Note the coronal imbalance in the patient. Fusion performed using the pre-psoas approach, showing the vertebral bodies almost horizontal with a good correction of the coronal Cobb’s angle.
Sagittal plane correction
Most often, ASD patients have a reduced lumbar lordosis and flat back. Restoration of lordosis and optimizing the pelvic parameters are among the primary aspects of managing patients with ASD. Compared to other approaches, Using the pre-psoas approach large interbody implants could be placed anteriorly in the disc space, thereby jacking up the collapsed and kyphotic disc spaces to improve the segmental lumbar lordosis and the overall sagittal vertical axis.
Better chances of fusion
A biomechanically better anterior column support is provided using the pre-psoas approach, as they allow for the insertion of a larger foot print cage. These cages span along the long axis of the vertebral body along the peripheral annular epiphysis of the vertebral body. This provides a suitable environment for fusion reducing the chances of cage subsidence.
Reducing the length of fusion constructs
In ASD, there is always a possibility of longer fusion constructs, especially in patients with significant deformities. As the interbody cages are inserted after releasing the annulus and removing the lateral osteophytes, the flexibility of the coronal curve is increased and the correction achieved would be better thereby reducing the need for extensive osteotomies and the length of posterior pedicle screw instrumentation.
Staging of the procedure
Following a multi-level fusion through the pre-psoas approach, patients can be staged for the percutaneous pedicle screw fixation. This reduces the prolonged anesthetic complications, especially in patients with profound cardiac risks, and a higher American Society of Anesthesiologists (ASA) grading. Nowadays, with the use of robotics and navigation, simultaneous pedicle screw fixation can be performed by two surgeons, in a single stage.
Lesser surgical morbidity
The surgical morbidity of this approach is comparably less than other approaches for deformity correction surgeries. This is owing to the reduced concomitant muscle damage and minimal blood loss. This enhances early post-operative recovery and improves overall surgical outcomes.
What cases to choose first—and is there a learning curve?
Most orthopedic and neuro spine surgeons are usually quite familiar with the posterior approach to the lumbar spine during their training phase. However, the pre-psoas approach utilizes the oblique corridor and hence, there is a learning curve to adapt this technique in day-to-day practice. For early adopters, it is safer to start your pre-psoas journey using single or two-level lumbar instability (listhesis) cases.
Patients with abnormal vascular anatomy, large bulky psoas, high iliac crest, and approaching a large deformity through the concavity of the curve are cases not suited for beginners using this approach. After gaining surgical confidence and familiarity with the retro-peritoneal anatomy, surgeons can expand their indications to lumbar deformities.
Also, during the procedure, attention has to be given to the preparation of the disc space, avoiding violation of the bony end plates and optimal position of the cage under fluoroscopy guidance. Injuries to the ureter, lumbar plexus, segmental vessel, and iliolumbar vein have been reported in literature and hence, a thorough knowledge of the anatomy is of paramount importance to master this minimally invasive technique.
About the authors:
References and further reading:
- Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, Liu J, Acosta F, Drochner TE. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine. 2014 Nov;21(5):785-93. Doi: 10.3171/2014.7.SPINE13564. Epub 2014 Sep 12. PMID: 25216400.
- Neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2015;40(3):E175–182.
- Park SW, Ko MJ, Kim YB, Le Huec JC. Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity. J Orthop Surg Res. 2020;15(1):13.
- Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37(12):1077–1082
- Zeng ZY, Xu ZW, He DW, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. 2018;10(2):98–106.
You might also be interested in:
Minimally Invasive Spine Surgery (MISS)
AO Spine MISS educational material and courses cover all types of MISS, through tubular/microscopic, endoscopic, and instrumented procedures, and pathologies that you deal with in your busy practice.
AO Surgery Reference
AO Surgery Reference degenerative spine disease modules developed by the AO Spine MISS Taskforce cover treatments for disc herniation, stenosis, and spondylolisthesis.
AO Spine courses and events
Explore the upcoming courses, webinars or online events in your region or worldwide. You can download a list of all upcoming events in your region in PDF format
AO Spine Guest Blog
Discover diverse views and perspectives on hot topics from the spine community around the world, learn how to promote your work effectively, or submit your proposal for a guest post.