Mastering full endoscopic spine surgery—an essay on the steep learning curve and adoption
BY DR WONGTHAWAT LIAWRUNGRUEANG

Full endoscopic spine surgery (FESS) is a minimally invasive technique used to treat various spinal disorders, such as herniated discs, spinal stenosis, and other degenerative spine conditions. This advanced surgical approach utilizes an endoscope—a small, flexible tube with a camera and light at its tip—to visualize and access the spine through small incisions. This essay delves into the surgeons' learning curve associated with mastering the technique, the motivations for driving its adoption, and the barriers to overcome its implementation.1
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
From a surgeon's viewpoint, FESS represents a paradigm shift in spinal surgery. Traditional open spine surgeries, while effective, often involve significant tissue disruption, leading to prolonged recovery times and higher complication rates. In contrast, FESS offers a minimally invasive alternative, promising reduced trauma, faster recovery, and lower postoperative pain.
Overcoming the steep learning curve2
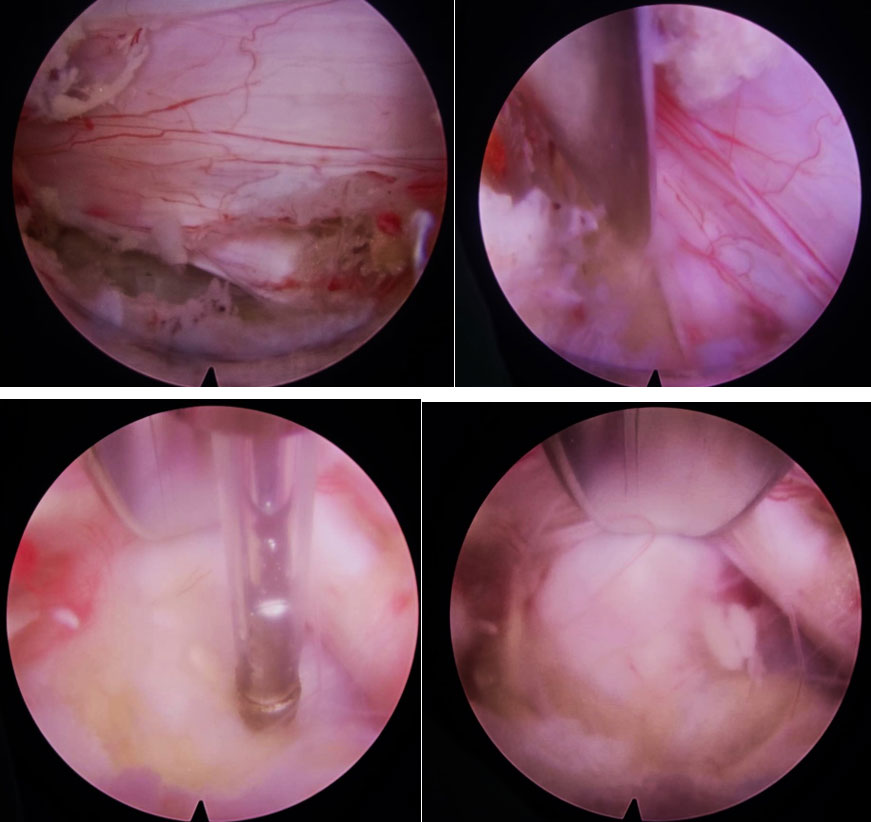
These benefits align with the overarching goal of enhancing patient outcomes while minimizing the risks associated with surgery. However, the transition to FESS requires a fundamental change in surgical approach and technique. Surgeons accustomed to open procedures must adapt to the use of an endoscope, which provides a different visual and tactile experience. The reliance on indirect visualization through a monitor, as opposed to direct sight of the surgical field, demands a high level of hand-eye coordination and spatial awareness.
The learning curve for FESS is steep and multifaceted, encompassing both technical skills and cognitive adaptation. Surgeons must acquire proficiency in handling endoscopic instruments, navigating the confined spaces of the spine, and interpreting endoscopic images. This technical mastery often requires extensive training, including cadaveric practice, simulation, and mentorship under experienced endoscopic spine surgeons.
The cognitive aspect of the learning curve involves a shift in surgical mindset. Surgeons must become comfortable with a less invasive approach, which may initially seem counterintuitive, especially for those with years of experience in open surgeries. Overcoming this cognitive barrier is essential for successful adoption and integration of FESS into clinical practice.
Motivation and barriers2
Several factors motivate surgeons to embrace FESS despite the challenges it presents. Firstly, the potential for improved patient outcomes is a powerful incentive. The prospect of offering a minimally invasive option with reduced recovery times and enhanced postoperative comfort aligns with the ethical commitment to patient welfare.
Secondly, professional development and staying at the forefront of surgical advancements drive surgeons to adopt new techniques. Mastery of FESS not only broadens a surgeon's skill set but also enhances their reputation and competitiveness in the field of spinal surgery.
Thirdly, the growing body of evidence supporting the efficacy and safety of FESS serves as a compelling motivator. Studies demonstrating comparable or superior outcomes to traditional open surgeries provide confidence in the technique's validity and encourage its adoption.
Despite these motivations, several obstacles impede the widespread adoption of FESS. The most significant barrier is the steep learning curve itself. Surgeons must invest considerable time and effort in training, often balancing this with their existing clinical responsibilities. Access to comprehensive training programs and mentorship opportunities is crucial but can be limited, especially in regions with fewer experienced endoscopic spine surgeons.
Another obstacle is the cost associated with acquiring and maintaining the specialized equipment required for FESS. Endoscopic instruments, imaging systems, and associated technologies represent a substantial financial investment, which may be prohibitive for some institutions and practitioners. Institutional resistance and inertia also pose challenges. Hospitals and surgical centers may be slow to adopt new techniques due to concerns about costs, training requirements, and potential disruptions to established protocols. Convincing administrative bodies and colleagues of the long-term benefits of FESS requires robust evidence and advocacy.
Key advantages of full endoscopic spine surgery3
- Minimally invasive: FESS requires only small incisions, typically less than 1 cm, compared to the larger incisions needed for traditional open surgery. This minimally invasive approach results in significantly less damage to muscles and surrounding soft tissues, leading to a faster and less painful recovery.
- Reduced recovery time: Due to the less invasive nature of FESS, patients can often return to their normal activities much sooner than after traditional open surgery. Hospital stays are typically shorter, and in many cases, the procedure can be performed on an outpatient basis.
- Less postoperative pain: The smaller incisions and reduced tissue disruption associated with FESS lead to less postoperative pain. This often translates to a decreased need for pain medications, which can have their own side effects and complications.
- Lower infection risk: Smaller incisions mean less exposure of internal tissues to potential contaminants, thereby reducing the risk of infections. Additionally, the decreased need for extended hospital stays further minimizes the risk of hospital-acquired infections.
- Preservation of spinal anatomy: FESS techniques allow for the precise removal of pathological tissue, such as herniated disc material or bone spurs, while preserving the normal anatomy of the spine. This approach helps maintain the structural integrity and function of the spine, which can contribute to better long-term outcomes.
Innovations and future directions
- Robotics and navigation: The integration of robotic systems and advanced navigation technologies is enhancing the precision and safety of FESS. Robotic assistance can help surgeons perform highly accurate and consistent movements, improving the overall success rate of the procedures. Navigation systems, such as intraoperative imaging and computer-assisted navigation, provide real-time feedback and detailed anatomical information, aiding in the precise placement of instruments and implants.4
- Improved endoscopic instruments: The development of more advanced and specialized endoscopic tools is facilitating the performance of increasingly complex procedures. Innovations include high-definition cameras, flexible instruments that can navigate the intricate anatomy of the spine, and multifunctional tools that combine cutting, grasping, and suction capabilities. These improvements enable surgeons to perform a broader range of procedures with greater accuracy and efficiency.4,5
- Artificial Intelligence (AI): AI is being leveraged for various aspects of FESS, from preoperative planning to intraoperative guidance and postoperative care. In preoperative planning, AI algorithms can analyze patient data and imaging studies to assist in identifying the optimal surgical approach and predicting potential challenges. During surgery, AI can provide real-time analysis and feedback, enhancing the surgeon's ability to make precise and informed decisions. In the postoperative phase, AI-driven tools can monitor patient recovery, detect early signs of complications, and guide rehabilitation protocols, ultimately improving patient outcomes.6
In summary, full endoscopic spine surgery represents a significant advancement in the field of spinal surgery, offering numerous benefits to patients and expanding the scope of minimally invasive treatments available for spinal conditions.
About the author:
Dr. Wongthawat Liawrungrueang is the Assistant Vice President (Foreign Affairs) of the Spine Society of Thailand (SST), Chair of the Spine Division, and Head of the Orthopaedics Department at the University of Phayao. Dr. Wongthawat conducts research in the fields of minimally invasive spine surgery, full-endoscopic spine surgery, artificial Intelligence, and software engineering. He currently serves as a board member of the Asia Pacific Spine Society (APSS) and as faculty of AO Spine.
References:
- Jitpakdee K, Liu Y, Kotheeranurak V, et al. Transforaminal Versus Interlaminar Endoscopic Lumbar Discectomy for Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Global Spine J 2023;13(2):575–87.
- Kotheeranurak V, Liawrungrueang W, Kuansongtham V, et al. Surgeons’ Perspective, Learning Curve, Motivation, and Obstacles of Full-Endoscopic Spine Surgery in Thailand: Results From A Nationwide Survey. Biomed Res Int 2022;2022:4971844.
- Kotheeranurak V, Liawrungrueang W, Quillo-Olvera J, et al. Full-Endoscopic Lumbar Discectomy Approach Selection: A Systematic Review and Proposed Algorithm. Spine (Phila Pa 1976) 2023;48(8):534–44.
- Jitpakdee K, Liu Y, Heo DH, et al. Minimally invasive endoscopy in spine surgery: where are we now? Eur Spine J 2023;32(8):2755–68.
- Kim J-H, Jitpakdee K, Kotheeranurak V, et al. Is navigation beneficial for transforaminal endoscopic lumbar foraminotomy? A preliminary comparison study with fluoroscopic guidance. Eur Spine J 2023;32(8):2808–18.
- Liawrungrueang W, Cho ST, Sarasombath P, et al. Current Trends in Artificial Intelligence-Assisted Spine Surgery: A Systematic Review. Asian Spine J 2024;18(1):146–57.
You might also be interested in:
AO Spine MISS resources
AO Spine Minimally Invasive Spine Surgery (MISS) educational material and courses cover all types of minimally invasive spine operations through tubular/microscopic, endoscopic, and instrumented procedures.
AO Spine Course calendars
Find your next educational event from the Course calendars, organized by region. The PDF calendars downloads summarize our upcoming, accredited, high-quality educational activities attracting thousands of surgeons and health care professionals each year.
AO Spine Guest Blog
The guest articles highlight perspectives from the spine community around the world, showcasing experiences and sharing knowledge from our community.
Are you interested in writing for the AO Spine Guest Blog? Read more and send in your ideas.