Surgical robots—into a new era for spine surgery instrumentation
In recent years, the rapid growth of technology and innovations continues to foster also spine surgeons with tools for better patient care and safer surgical practices. Robotic technology has emerged as an invaluable addition to spine surgeon’s armamentarium, enabling them to perform complex surgeries with more precision and improved patient outcomes.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Spine surgery has always been a fascinating field in the orthopedic and neurosurgical domain with its unmapped landscape of unanswered concepts and much scope for research in spinal disorders and their management. As the complexities of spine-related issues escalate, arriving at optimal solutions is mandatory. Robotics can provide one solution for safer complex surgeries and better outcomes.
What is robotic spine surgery?
In robotic/robotic-assisted spine surgery, specialized robotic systems are employed to assist surgeons in performing surgical procedures. They provide real-time intra-operative navigation and rigid stereotaxy using Computer Assisted Navigation (CAN) and image-guided platforms. Generally, three categories of surgical robotic systems are available viz. supervisory controlled systems, tele-surgical systems, and shared-control robots.
Shared-control robots are the widely used systems in modern spine surgical practice, where the surgeon and robot simultaneously control the surgical instruments in the operative field. A mount with a robotic arm, a navigation tracking camera, and a display monitor are the essential components in this type of robotic systems.
How robots in spine surgery work?
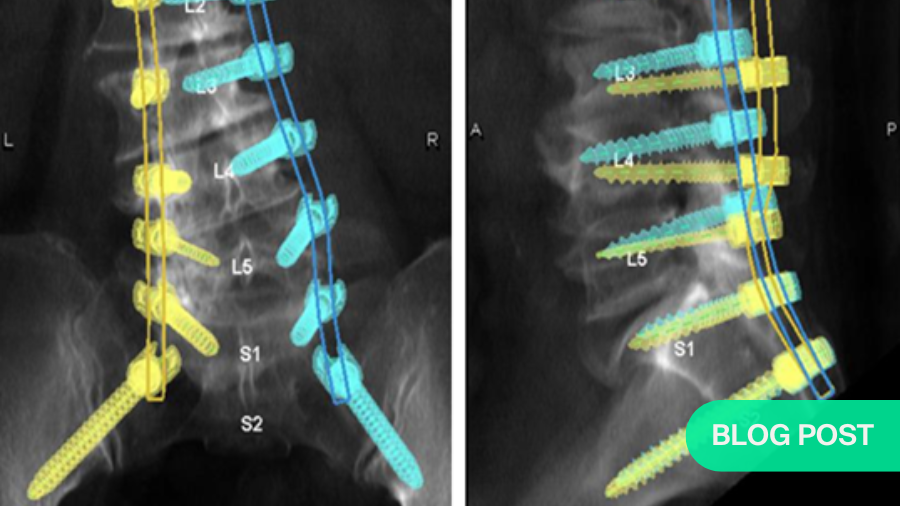
The most common use of the robots in spine surgery is for placement of the pedicle screws. The surgical planning of the pedicle screws (starting point, trajectory, length, diameter) is performed pre-operatively using the CT scan of the patient by the robotic software.
Intra-operatively, the robot is either attached to the operating table (i.e.) table-mount or floor mount at one end of the patient. A navigation tracking camera is placed at the other end to track the position of the patient and the navigated instruments/ implants during screw insertion.
The robotic software then performs a ‘3-D scan’ to register the position of the patient in space. Using an image intensifier, fluoroscopy images of the area of interest are then obtained. Matching of the bone windows of the CT scan stored in robotic software with these fluoroscopic images is performed. This is a critical step that enables the robotic software to configure and understand the bony anatomy of the patient (placed in a prone/ lateral position for a pedicle screw fixation).
This is followed by the registration of all the surgical instruments (bone awl, pedicle finder, and bone tap) and implants to the navigation software.
Once all these steps are completed, the operating technician aligns the robotic arm to the required position over the surgical site (based on the commands of the surgeon) and guides the trajectory for the insertion of pedicle screws.
Dr Jacob Yoong Leong Oh and Dr Guna Pratheep Kalanchiam performing robotic-assisted Lateral and Prone surgeries:
Why should spine surgeons use surgical robots?
We see several advantages in using robotics in spine surgery both for patients and surgeons, for hospitals and the wider society. As with any new technology, there might be limitations, teething problems, and cost issues to consider. Despite the attractive advantages listed below, it is Important to remember that robots will only enhance spine surgeons’ skills and do not replace them.
1) Less invasive:
These minimally invasive robotic surgeries typically require smaller incisions compared to conventional open surgery. These smaller incisions result in less pain, reduced scarring, minimal blood loss, and decreased need for blood transfusion. The cosmetic appearance of the surgical scar is also improved by these key-hole incisions.
2) More safety:
Pedicle screws are the most commonly employed spinal implants in the last few decades owing to their biomechanical superiority compared to others. By enabling high-definition 3D visualization, intra-operative navigation, and fine instrument control, robotic systems guide the accurate and precise trajectory of the screw placement with lesser chances of cortical breach. The lengths and diameters of the screws could also be planned pre-operatively enabling three-column fixation even in patients with altered bony anatomy.
All these mitigate the catastrophic neurological and vascular-related complications related to spine instrumentation. Studies have shown a significant difference in accuracy between the use of fluoroscopy and robotic-guided pedicle screws.
3) Faster recovery:
By minimizing tissue retraction and reducing the stripping of the soft tissues and muscle damage, the intra-operative use of robotic systems has enhanced post-operative patient recovery. Reduction in collateral tissue injury minimizes inflammatory mediators at the surgical site thereby alleviating the need for strong analgesic medications like opioids. Early mobilization and implementation of ERAS protocols further improve the functional recovery of patients and improve patient satisfaction.
4) Difficult to access areas:
Surgical robots by adapting the navigation technology, offer depth perception and spatial awareness of the surgical field even in the tissues that are not visualized directly by the surgeon during surgery. This enables the surgeons to perform more controlled surgical maneuvers. Robots also help plan the osteotomies and the extent of bony resections in surgeries like complex spinal deformities. In spine tumor surgeries, they provide a targeted approach and enable adequate tumor removal providing disease-free margins.
5) Lesser complications:
Complications associated with spine surgeries like infections and delayed wound healing, could be devastating and result in significant morbidity. Being a minimally invasive strategy, robotic-assisted surgeries reduce the risk of postoperative infections. Also, lesser soft tissue damage and preserved vascularity of these tissues enhance the overall wound healing of the surgical site.
6) Duration of surgery:
As the surgical steps, like placement of incisions and instrumentation of the spine, are all executed with the guidance of a robotic system, the overall duration of the surgical procedure is less compared to open surgeries. However, the early days of its application will require more time for the setup and understanding of its workflow by the surgical team. In the future, this can be further reduced by optimizing the preparation process and skilled use of the robot.
7) Cost-effectiveness:
As previously mentioned, by minimizing complications, hastening post-operative recovery, and shortening the hospital stay, surgical robots improve the overall cost-effectiveness of the procedure. Though the initial procurement of the technology may be higher, considering the long term, it will be of immense benefit in reducing the expenditure on healthcare.
8) Better ergonomics:
Robotic surgery minimizes the physical strain experienced by surgeons during procedures. Unlike traditional surgery, where surgeons often maintain physically demanding positions for extended periods, robotic surgeons assume a comfortable position, as the robotic arm moves in the surgical field. This ergonomic advantage reduces the risk of musculoskeletal exertion and fatigue, contributing to the overall well-being of the surgeon.
Any newer technology has several limitations. It must be noted that there could be a discrepancy between the preoperative CT imaging and intra-operative registration of the patient. This can be due to excessive soft tissue in the patient, poor image quality, surgeon error during registration, or a combination of these factors.
Also, the economic viability of such a device in all settings is practically not possible and for now, it could only be available in a resource-rich operative environment.
Robotic-assisted surgery has already emerged as one of the prominent options in the field of spine surgery and will only continue to evolve with further advancements in artificial intelligence and machine learning.
Despite these innovations, we, surgeons have to understand that it is the knowledge and prowess of the surgeon that guides the robotic technology and should always continue to strengthen our surgical skills.
About the authors:
Dr Guna Pratheep Kalanchiam MBBS; MS (ORTHO); FNB (SPINE); FESS; FMISS, is a fellowship trained Orthopaedic spine surgeon from Madurai, Tamilnadu, India. He is specialized in endoscopic (uniportal/biportal), minimally invasive, navigation, and robotic spine surgery. He has presented his work in several national and international conferences. Dr Guna has a keen interest in research and has published his work in various high impact international scientific journals. He is an active member of AO Spine, AO Spine Youth Club, Asia Pacific Spine Society (APSS), Association of Spine Surgeons of India (ASSI), and the Pacific and Asian Society of Minimally Invasive Spine Surgery (PASMISS).
References and further reading:
- Rasouli JJ, Shao J, Neifert S, Gibbs WN, Habboub G, Steinmetz MP, Benzel E, Mroz TE. Artificial Intelligence and Robotics in Spine Surgery. Global Spine J. 2021 May;11(4):556-564. doi: 10.1177/2192568220915718.
- Pratheep, Guna; Murugan, Chandhan; Rajasekaran, Shanmuganathan; Shetty, Ajoy Prasad; Kanna, Rishi Mugesh. Role of Robotics and Spinal Navigation in Reducing Surgical Complications. Indian Spine Journal 6(1):p 37-47, Jan–Jun 2023. | DOI: 10.4103/isj.isj_72_22
- Perfetti, Dean C; Kisinde, Stanley; Rogers-LaVanne, Mary P; Satin, Alexander M; Lieberman, Isador H. Robotic Spine Surgery: Past, Present, and Future. Spine 47(13):p 909-921, July 1, 2022. | DOI: 10.1097/BRS.0000000000004357
- Farber SH, Pacult MA, Godzik J, Walker CT, Turner JD, Porter RW, Uribe JS. Robotics in Spine Surgery: A Technical Overview and Review of Key Concepts. Front Surg. 2021 Feb 23;8:578674. doi: 10.3389/fsurg.2021.578674.
- Kim HJ, Jung WI, Chang BS, Lee CK, Kang KT, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot. 2017;13. doi:10.1002/rcs.1779.
You might also be interested in:
Minimally Invasive Spine Surgery (MISS)
Explore AO’s MISS resources and educational offerings, including the annual MISS Spectrum Series, developed and taught by the global AO Spine MISS Task Force experts.
AO Davos Courses
Join our advanced courses with human anatomical specimen on lumbar degeneration procedures or dealing with complex deformity and revision problems of the cervical spine.
Innovation at the AO
AO Innovation Translation Center offers funding and drives AO’s innovation projects with partners, including clinical solutions, evidence, proof-of-concept, and strategic investment.
AO Spine Youth Club
The AO Spine Youth Club (AO SYC) connects young spine surgeons worldwide and provides information and ‘edutainment’, specifically addressing young surgeons’ needs.









