Sequencing in orthognathic treatment: the maxilla-first approach for predictable outcomes
WITH DR PATRICIA STOOR
Orthognathic surgery involves repositioning the maxilla, mandible, or both to improve the maxillomandibular relationship. Patients undergo these procedures for various reasons, including malocclusion, temporomandibular disorders, or aesthetic concerns. Over the years, surgical techniques have evolved, and advancements in 3D imaging and patient-specific implants have significantly improved surgical planning and outcomes.
This article discusses the rationale for favoring a maxilla-first approach, explores common complications in bimaxillary surgery, and explains how modern technology helps mitigate these challenges. It is a companion article to Maxilla- or mandible-first approach: what is the rationale? by Prof Federico Hernández-Alfaro and Dr Adaia Valls-Ontañón.
-
Read the quick summary:
- Proper maxillary positioning improves facial aesthetics, occlusal accuracy, and overall balance of the facial structure.
- The maxilla-first approach in orthognathic surgery offers predictable outcomes and mitigates complications like condylar sag and bad split.
- 3D imaging and patient-specific implants enhance surgical planning and precision, ensuring stable condylar positioning.
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
Complications in orthognathic surgery: condylar sag and bad split
A key challenge in orthognathic surgery is managing complications that arise during bilateral sagittal split osteotomy. One of the most concerning is condylar sag, which occurs in as many as one in seven patients undergoing this procedure. In fact, more than 10% of these cases present with an intraoperative diagnosis of condylar sag, which can result in anterior open bite, posterior bilateral open bite, or midline deviation of the lower incisors. Another common complication, bad split, affects up to 5.5% of bilateral sagittal split osteotomies, potentially compromising surgical outcomes.
When considering the sequencing of surgery, it is crucial to weigh the advantages and drawbacks of each approach. Choosing a mandible-first sequence can lead to unforeseen movements of the maxilla due to intraoperatively undiagnosed condylar sag. This can result in compromised bilateral sagittal split osteotomy outcomes, insufficient mandibular movement, or even midline shifts. While it is possible to achieve proper occlusion with a mandible-first approach, there is a risk of clockwise closure instead of counterclockwise rotation, which can alter facial aesthetics, especially if a subtle canting of the occlusal plane occurs.
The maxilla-first approach: advantages and considerations
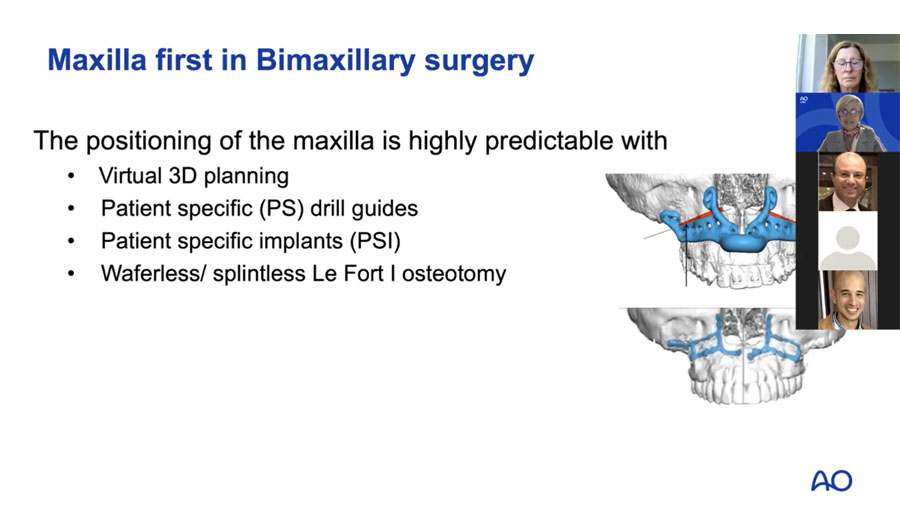
In certain cases, particularly those involving condylar pathologies, severe asymmetries, or severe open bite, a maxilla-first approach is strongly recommended. This method allows for a waferless (splintless) osteotomy, combined with 3D planning and patient-specific implants, which help prevent issues such as condylar sag, mandibular midline deviation, and insufficient mandibular movement.
For optimal results, any bimaxillary surgical plan must begin with the mandible in a stable condylar position, as this is a fundamental factor in achieving stable outcomes. Literature emphasizes the importance of temporomandibular joint stability in orthognathic procedures, and I believe that preoperative identification of this stable joint position is essential for every patient, regardless of whether they have temporomandibular joint pathology. Surgery should never be performed during active temporomandibular joint changes or if the patient is experiencing condylar pain.
To establish joint stability, conservative treatments such as occlusal splint therapy or physiotherapy can be utilized preoperatively. If splint therapy is chosen, it should be applied for at least three months or until the joint position has stabilized. Depending on the case, different options such as a one-piece splint for nighttime use or a three-piece splint for continuous use may be considered.
The role of imaging in orthognathic surgery
The integration of 3D imaging, cone-beam computed tomography (CBCT), and computed tomography (CT) scanning has revolutionized orthognathic surgery. A well-structured bimaxillary surgical plan should start with a CBCT or CT scan with the jaw in a stable joint position. This position should be accurately recorded by having patients wear a solid bite index during the scan. This simple step allows verification of the joint position when surgery begins—if the bite index does not fit under general anesthesia, it indicates that the stable condylar position was not achieved while the patient was awake.
When performing a maxilla-first approach, achieving the stable condylar position preoperatively is crucial. If this step is neglected, the intermediate splint may not fit during surgery, complicating the procedure. One solution is the use of patient-specific implants, which can guide the maxilla into its correct, pre-planned position. Additionally, CBCT or CT scans allow for postoperative verification of condylar positioning, ensuring alignment with the preoperative plan.
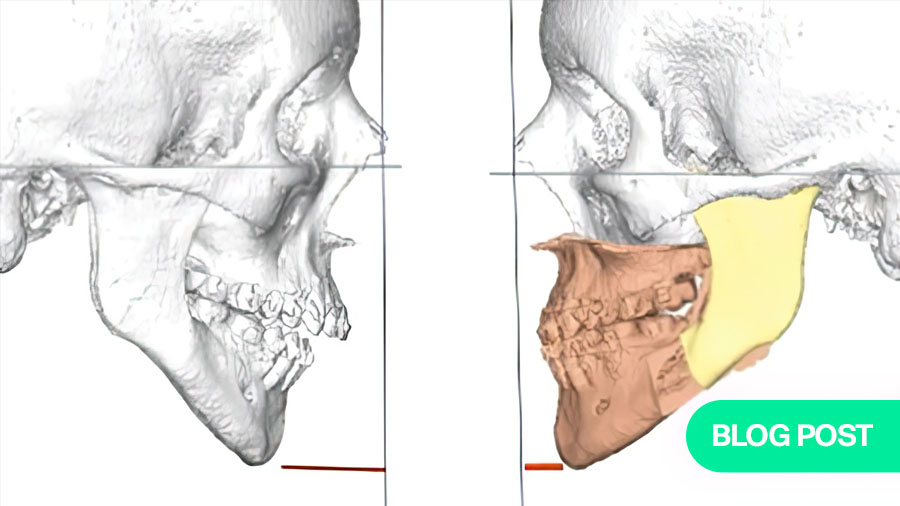
Why the maxilla-first approach offers greater precision
One of the major advantages of starting with the maxilla is its profound influence on the mandible’s position and movement. For instance, when correcting facial height, the maxilla must first be aligned, after which the lower jaw can be positioned correctly in occlusion. Similarly, transversal widening of the maxilla and midline adjustments can be planned in advance, ensuring that any changes are accounted for in the final splint.
Facial aesthetics, including the position of the pogonion (the most forward point on the chin), are also largely dependent on maxillary positioning. If increased protrusion of the lower jaw is required, counterclockwise rotation of the occlusal plane can be performed. This rotation directly affects the condylar fragments and angular areas, and in cases involving asymmetric mandibular advancement, a posterior rotation of the maxilla can help balance the necessary movements to prevent excessive tilting on one side.
It is important, however, to avoid creating aesthetic black corridors—gaps between the teeth and cheeks—which can occur if the posterior maxilla is rotated too aggressively. A well-positioned maxilla not only facilitates occlusal accuracy but also enhances lower face symmetry, midline alignment, and the overall balance of the facial structure.
The power of 3D planning and patient-specific implants
The use of 3D planning and patient-specific implants has transformed the field of orthognathic surgery, allowing for greater precision in condylar positioning, avoidance of condylar sag, and improved management of bone interferences. Unlike traditional surgical scanning, 3D planning enables detailed assessment of the degrees of rotation possible in a patient, particularly in cases with potential condylar pathologies.
While patient-specific implants are most commonly used for the maxilla, customized implants for the mandible are also becoming available, expanding the range of possibilities for condylar positioning and proximal fragment rotation. These technological advancements significantly reduce surgical variability and increase predictability in outcomes.
Challenges and controversies in the maxilla-first approach
Despite its advantages, the maxilla-first approach has its challenges. In traditional model surgery, both intermediate and final splints are required for maxillomandibular fixation, which can be complex if the stable joint position is not clearly defined preoperatively. Additionally, in cases of large counterclockwise rotations, the thick intermediate splint may be difficult to position, affecting intermaxillary fixation.
However, 3D planning and patient-specific implants help overcome these issues. If the stable condylar position is unclear, the maxilla can be fixed splintless, allowing for adjustments. Moreover, splintless maxilla fixation can facilitate cases involving large counterclockwise rotations, preventing the need for cumbersome intermediate splints.
In certain situations, such as posterior down grafting of the maxilla, the bilateral sagittal split osteotomy can be more challenging. One preferred approach in these cases is to perform the osteotomy lines in the mandible first, complete the Le Fort I osteotomy, secure the maxilla with patient-specific implants, and then split the mandible last, ensuring accurate positioning.
Why the maxilla-first approach leads to predictable outcomes
There are compelling reasons to prioritize the maxilla in bimaxillary surgery. Le Fort I osteotomies are generally less prone to complications, straightforward to perform (especially with 3D planning), and highly predictable in terms of aesthetic and functional outcomes. Proper maxillary positioning ensures an ideal smile line, soft tissue balance, and occlusal accuracy.
In contrast, the bilateral sagittal split osteotomy carries a higher risk of complications, such as condylar sag, anterior/posterior open bites, midline shifts, and bad splits. By addressing the maxilla first, these risks are minimized, allowing for a more predictable final result, and a harmonious facial appearance.
For these reasons, a maxilla-first approach in bimaxillary surgery is strongly advised, as it consistently leads to more stable, precise, and aesthetically satisfying outcomes.
Watch the full AO CMF Expert Case Discussion—Orthognathic Surgery, Mandible First vs Maxilla First presentation outlining different approaches for orthognathic surgery, mandible first vs maxilla first, presented by Patricia Stoor and Federico Hernandez Alfaro.
This blog post is a companion article to Maxilla- or mandible-first approach: what is the rationale? by Prof Federico Hernández-Alfaro and Dr Adaia Valls-Ontañón.
About the expert:
Patricia Stoor has been actively involved in research since 1993, and she obtained her PhD on biomaterials and microbes. Her research work resulted in two US patents. Her latest research interests include 3D planning, patient-specific implants in reconstructive surgery, trauma, deformity, and orthognathic surgery. Recently, she contributed to a multicenter study on dental implants, which was presented at the EAO congress in September 2022 in Geneva. She has published more than 30 publications.
You might also be interested in:
Further resources on orthognathic surgery
Explore AO CMF’s resources on craniomaxillofacial orthognathic surgery.
Orthognathic Surgery with Human Anatomical Specimens
Elevate your orthognathic surgery skills and expertise in orthognathic surgery with the intensive 2-day AO CMF course.
AO Surgery Reference
The all-in-one online reference supporting you from patient assessment to aftercare. The CMF section includes Trauma, Sequela, Orthognathic, Reconstruction, and Congenital deformities.
AO CMF Global Study Club
A dynamic platform for AO CMF members to discuss cases, share experiences, and network effectively.


.png?h=506&iar=0&w=900&rev=b21ac33735a64efbb5bd16621f4a93d3)


