Changing faces, changing lives: Correction of facial defects using patient-matched subperiosteal implants
BY PROFESSOR JOHAN REYNEKE
Over the past decades, there have been significant advances in reconstructive facial surgery with patient-matched subperiosteal implants delivering clinical outcomes which could only be described as ‘unbelievable’. The evolution from a purely visual surgical analysis to the use of complex 3D technologies in facial surgery have allowed surgeons to measure defects and plan the reconstruction of a specific area of the face with precision. The expert presentation by Prof Johan Reyneke focused on the correction of facial defects by means of patient matched subperiosteal implants. Prof Reyneke walked through the various considerations for implants for facial reconstruction and presented several real-life cases to show the outcomes of using modern patient-matched implants.
From distraction osteogenesis to patient-matched implants
There are numerous patient-matched subperiosteal implants available for correction of facial defects, and at the same time, any location in the face can be augmented. There are also diverse methods in use for facial defect correction including orthognathic surgery for repositioning existing bone and soft tissue, distraction osteogenesis, or grafting. Grafting in maxillofacial surgery is a procedure that replaces missing structures with tissues from the patient’s own body or with artificial, synthetic, or natural substitutes.
Watch the recording of the expert presentation by Johan Reyneke on “Correction of Facial Defects by Means of Patient Matched Subperiosteal Implants” in the AO Video Hub (members only):
Considerations for selecting patient-matched subperiosteal implants
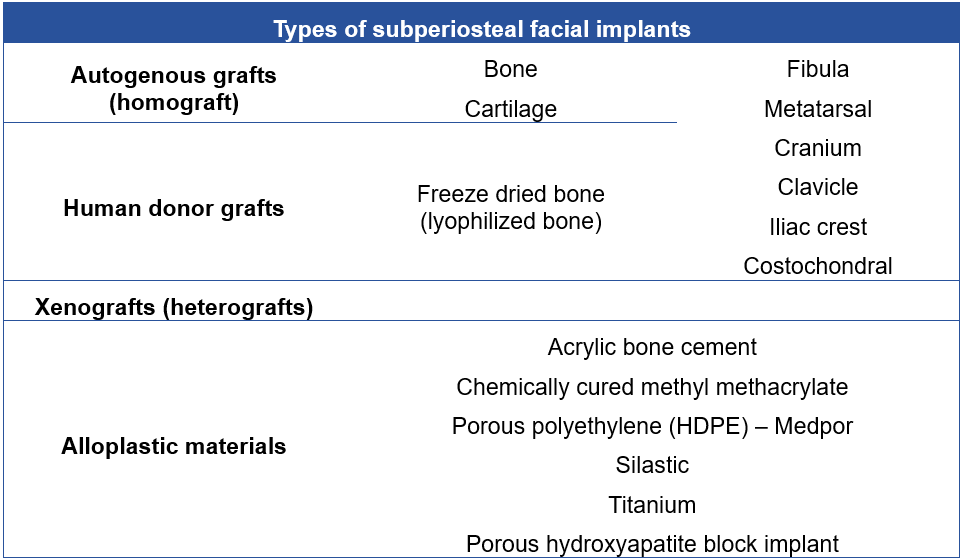
When considering the type of subperiosteal implant, autogenous grafts, human donor grafts, xenografts or alloplastic materials may be used (Table 1). Often bone or cartilage is harvested from the patients themselves, but an alternative is to use a human donor graft such as freeze dried or lyophilized bone. Xenografts and alloplastic materials also have their place in reconstructive surgery, the latter of which is the focus of this article.
Allographic materials and facial defect correction through implants has extensively developed over the years. Around 40 years ago, in the absence of rigid fixation techniques, early mandibular reconstruction could be performed in some cases using just a modified Kirschner wire splint [1]. This early technique, although now considered rudimentary, provided a good base for the advanced technologies seen today. Modern techniques have been further influenced by other developments, such as those in imaging, with the 3D images available today allowing for 3D printed models and production of patient-matched implants. These improvements have carried over into treatment planning, which has also advanced to such an extent that exact measurements of a facial defect can be performed.
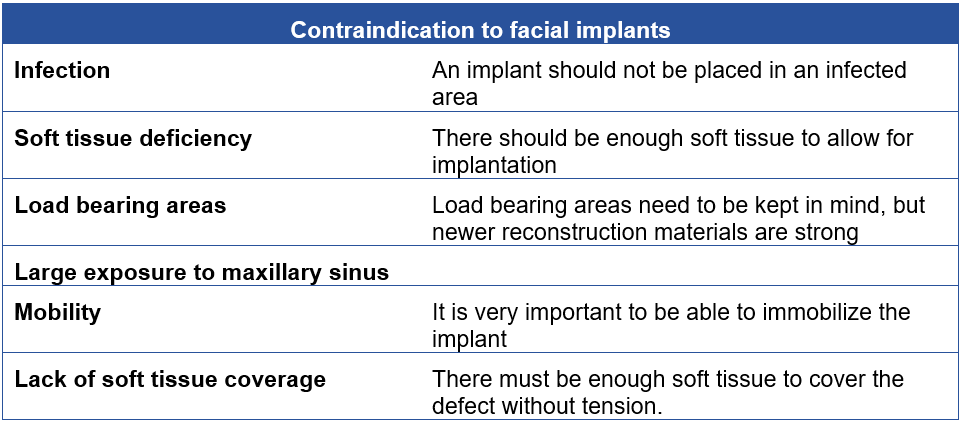
When considering implants for facial reconstruction, the ideal implant should fulfil several criteria. They should be readily available and affordable, sterilizable, strong, inert, non-allergenic, durable, non-carcinogenic, be easily manipulated and shaped, and suitable for single-stage reconstruction. There are also several contraindications to facial implants (Table 2), such as infection or soft tissue deficiency. Regarding load bearing areas, this is no longer such a problem, because of the rigid fixation and materials used.
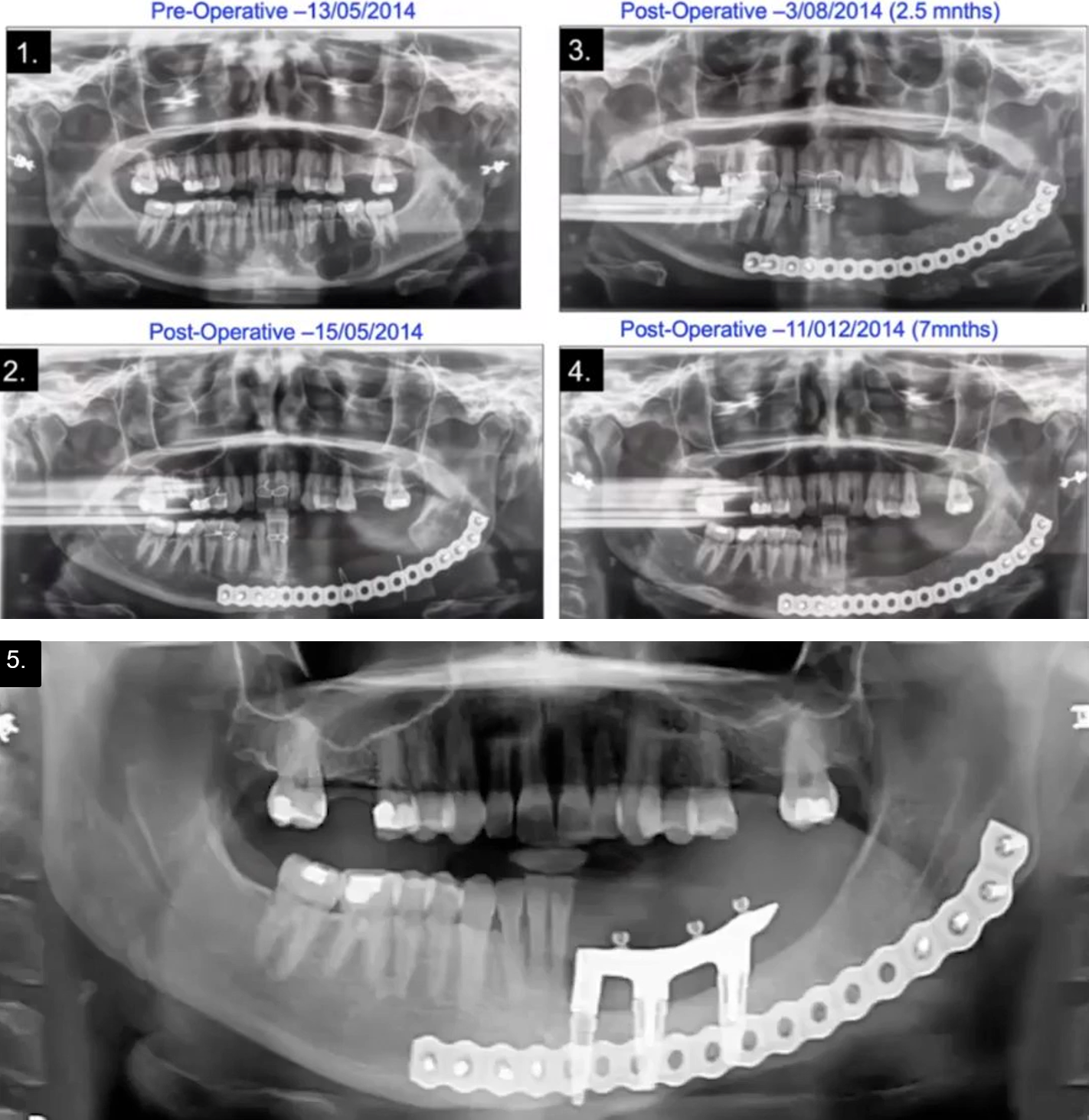
Patient-specific implant placement in an ameloblastoma patient: advantages of 3D technologies in facial surgery
A case with Professor Carlo Ferretti involved a patient with ameloblastoma requiring resection and reconstruction [2]. The 3D virtual planning was very beneficial, as the patient-matched reconstruction plate could be bent on a 3D printed model allowing for the development of cutting guides for the patient-matched plate. The tumor was resected intraorally, resulting in no external incision, and the plate was inserted followed by a silastic spacer with similar anatomy to the part of the mandible removed. Once the defect was closed, the spacer remained in situ for three months, after which it was removed through a small extraoral incision. Compressed particulate cortico-cancellous iliac crest bone was then injected into the pocket left behind after removal of the spacer. The final reconstruction involved implants placed into the graft, a successful procedure accurately executed through the assistance of virtual treatment planning (Figure 1).
Innovations in patient-matched implants for use in trauma cases
The above-described case is a good example of when an implant is not indicated. However, there are numerous cases when patient-matched implants are indicated, particularly in diverse craniomaxillofacial trauma cases.
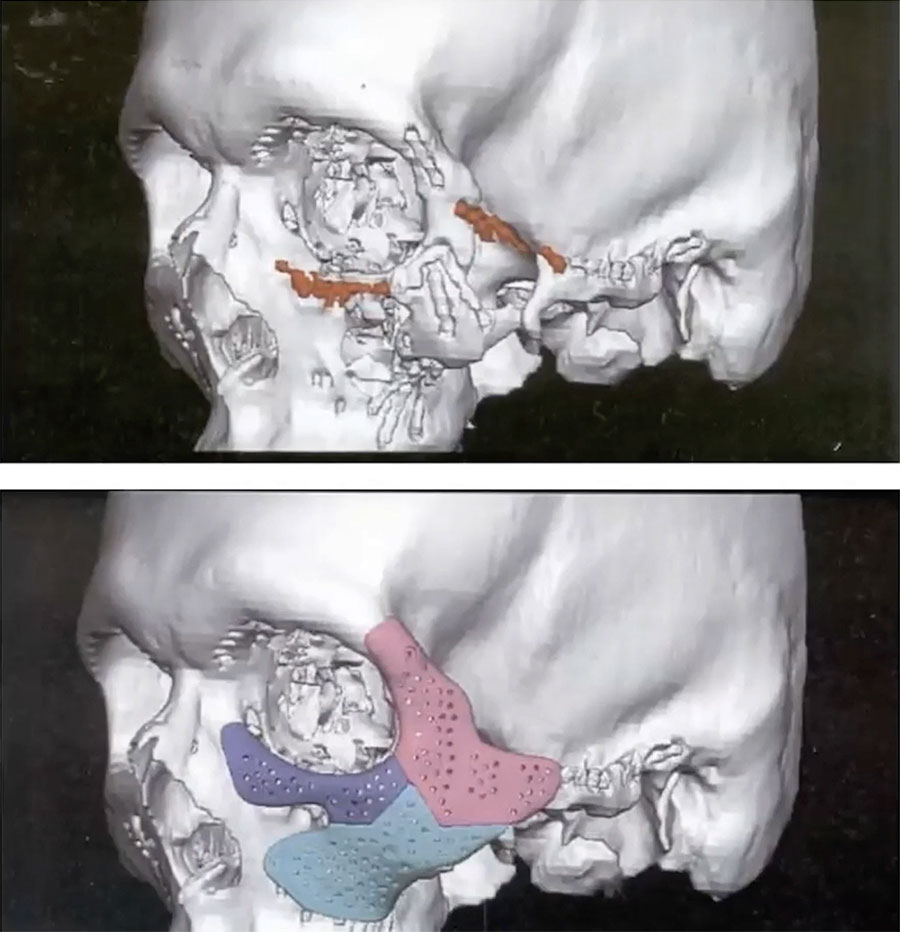
A patient initially presented with class II malocclusion and was referred for orthognathic surgery. However, the patient incurred a ballistic injury to the left zygomatic area prior to the orthognathic surgery and was treated elsewhere. A residual zygomatic defect occurred, and it was decided to defer correction for simultaneous correction with his orthognathic surgery. To resolve both issues, the treatment plan was to perform a sagittal split osteotomy, advancing the mandible, and at the same time augmenting the defect of the left zygoma.
During the initial reconstruction 17 bone plates had been inserted which hindered the ability to perform an osteotomy. After removal of several plates a large three-piece zygomatic patient-matched implant was inserted. The defect in this patient was large, requiring a large implant. A three-piece implant was designed to allow for insertion coronally, intraorally and infra-orbitally. The patient had a successful outcome with stability and functionality still at 10 years postoperatively.
In a second trauma case, a patient had a large cranial defect having lost the outer table of the skull after a head injury sustained in a bicycle accident. To correct the defect, a polymethyl methacrylate and polyhydroxyethyl methacrylate patient-matched implant was designed. In this patient the inner table of the skull was very thin and mobile which added another layer of complexity to the surgery. After dissection, the implant was placed and fixed with two-to-three small bone plates. The patient had a good clinical outcome with high satisfaction after resolution of the bone defect.
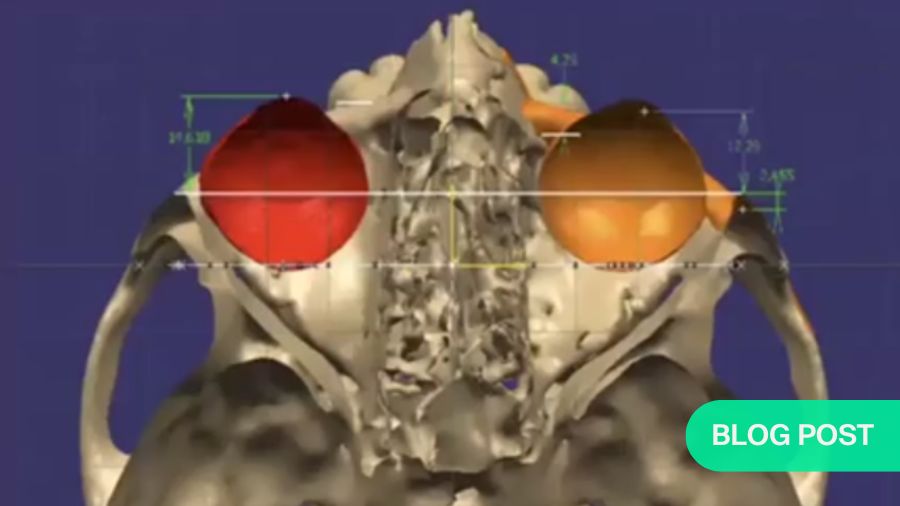
Patient-matched implants can also be used in young patients to correct diplopia occurring because of facial trauma. A young patient sustained a zygomatic injury which developed into enophthalmos with a slight facial defect. As a result, the patient also developed diplopia, which can be challenging to correct in the long term. The initial 3D cephalometric image revealed that the right orbit was lower and more inferior than the left orbit. With the use of 3D simulation, a treatment plan was created which involved repositioning the globe of the eye, placing an implant in the orbit with the correct volume and in the correct position to support the globe, and placing a patient-matched implant to augment the right zygoma. At five years post-surgery, the diplopia was corrected, and the patient had a good esthetic outcome.
Bone grafting and patient-matched implants in hemifacial microsomia
Patients with hemifacial microsomia have a long treatment pathway, being first seen at the ages of two or three years and followed through to adulthood. An important consideration in the treatment of hemifacial microsomia is the timing of each procedure: the timing of each corrective procedure should also consider the patient’s development as well as their psychological state.
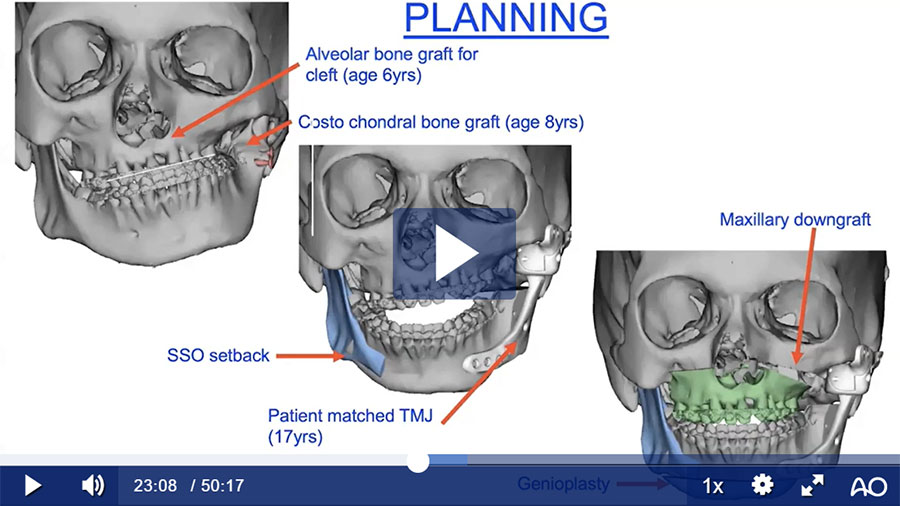
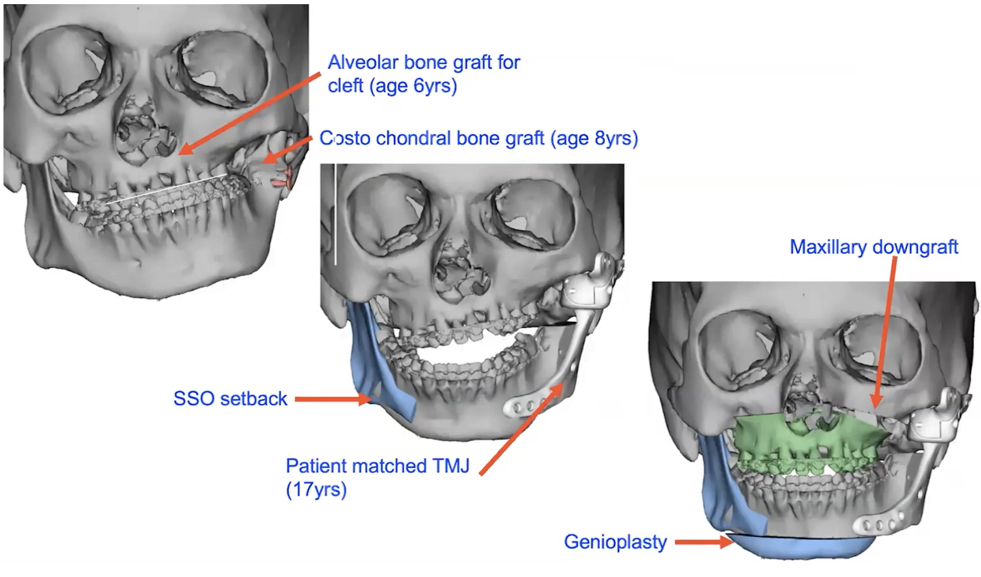
In the case of one patient with hemifacial microsomia also involving cleft palate, a bone graft was used to correct the alveolar cleft at the age of six years. Later, a costochondral graft was performed to reconstruct the left condyle and ramus of the mandible when the patient was eight years old. Unfortunately, the costochondral graft did not grow; costochondral grafts should be viewed critically as they are unpredictable, sometimes growing excessively, sometimes not at all, and they can also be subject to infection and/or ankylosis.
By seventeen years of age, the patient’s deformity had worsened, and a severe asymmetric Class III malocclusion had developed. From a psychological point of view, the patient was very unhappy. The final treatment plan consisted of placement of a patient-matched temporomandibular joint and setback of the mandible on the right side with a sagittal split osteotomy, a Le Fort I osteotomy with the correction of the canted occlusal plane (maxillary downgraft on the left) and genioplasty to correct asymmetry (Figure 3).
Advantages and disadvantages of patient-matched subperiosteal implants
There are several advantages of patient-matched subperiosteal implants: they allow for immediate postoperative physiotherapy, especially in a patient with TMJ ankylosis; there is no donor site morbidity; surgical time is decreased; the implant mimics the normal patient anatomy; there is maintenance of stable occlusion; orthognathic surgery can be performed at the same time; and the glenoid fossa is reconstructed simultaneously. The main disadvantage is the cost of the implant; however, it needs to be weighed up against additional morbidity and costs of increased operating time. Material wear and tear may occur, however, clinical experience—as well as the results of several long-term studies—has shown that in practice this is minimal.
The many advantages of patient-matched subperiosteal implants can be seen in the patients many years later, not just changing faces, also changing lives.
About the author:
Professor Johan P. Reyneke has served as professor in the department of maxillofacial and oral surgery at the university of the Witwatersrand in Johannesburg since 1991 and was appointed extraordinary professor of the University of the Western Cape in South Africa in 2014. Internationally, he holds professorships at the university of Oklahoma and Florida in the USA as well as the university of Nacional Autònoma de Mexico, San Salvador, Mexico. He is currently a visiting Professor at the University of Amsterdam.
Prof Reyneke has a passion for Orthognathic and Reconstructive facial surgery and has published more than 93 papers in refereed journals and delivered numerous courses and lectures.
References and further reading:
- Reyneke JP, Wilcock VE. Immediate mandibular reconstruction after resection using a modified Kirschner wire splint. J Oral Surg. 1979;37(6):415-418.
- Ferretti C, Muthray E, Rikhotso E, Reyneke J, Ripamonti U. Reconstruction of 56 mandibular defects with autologous compressed particulate corticocancellous bone grafts. Br J Oral Maxillofac Surg. 2016;54(3):322-326.
You might also be interested in:
AO CMF Global Study Club
Join the dynamic platform for AO CMF members to discuss cases, share experiences, and network effectively.
myAO
Join the myAO AO CMF Global Study Club group to get access to the registration link and watch the recorded sessions.
AO CMF Guest Blog
Diverse views and perspectives from the craniomaxillofacial community around the world.
Not a member yet?
Join AO CMF and position yourself to make the right decisions in the operating room.