Orthognathic surgery enhances obstructive sleep apnea management—lifestyle changes precede surgical intervention
BY DR PANG-YUN CHOU
Sleep apnea is a common sleep breathing disorder, mainly divided into obstructive and central types. Obstructive sleep apnea (OSA) refers to the collapse of the upper respiratory tract during sleep, resulting in respiratory cessation due to airflow blockage. This can lead to serious comorbidities that significantly affect the person’s quality-of-life. Treatment of sleep apnea starts with lifestyle changes, but orthognathic surgery may be recommended as a highly effective treatment option, especially in severe cases.
The most affected populations include men, the elderly, and people with obesity or excessive neck circumference. Common clinical symptoms of sleep apnea include snoring, frequent urination at night, and insomnia. Dry mouth when waking up, headache, not getting enough sleep, excessive fatigue and drowsiness during the day, difficulty concentrating, and high blood pressure1.
In Taiwan, approximately 10% of adults contend with obstructive sleep apnea, predominantly affecting males. However, cardiovascular diseases have emerged as the leading cause of mortality worldwide. Recent evidence suggests a heightened risk of cardiovascular mortality among patients with obstructive sleep apnea (OSA)2. Furthermore, OSA is associated with other comorbidities such as depression, asthma, and gastroesophageal reflux disease (GERD).
How to approach treating obstructive sleep apnea
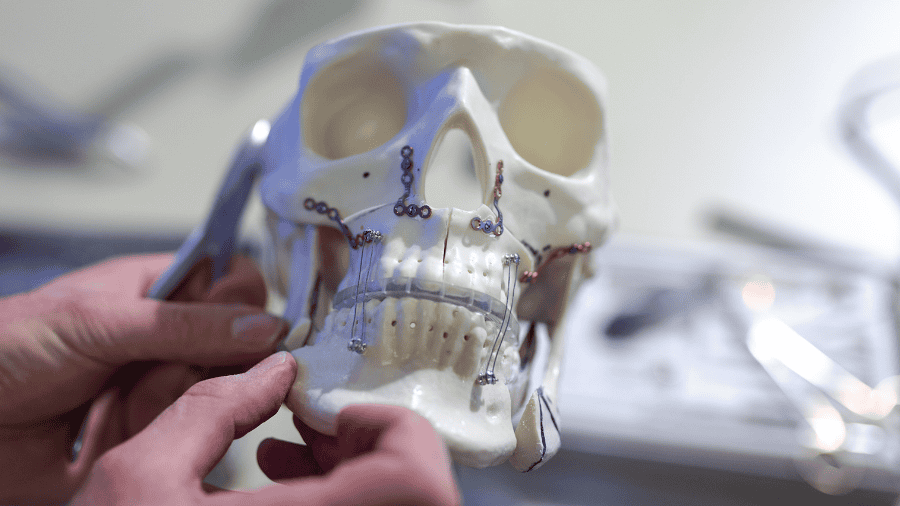
The approach to treating obstructive sleep apnea initiates with assessing the patient's body mass index (BMI) alongside their work and dietary habits. Encouragement is given for weight management, dietary adjustments, and the maintenance of healthy lifestyle habits. Following the assessment for anatomical obstructions in the oropharyngeal airway by an otolaryngologist, orthognathic surgery may be recommended. This surgical procedure involves repositioning the upper and lower jaw bones to expand the volume of the oropharyngeal airway, thereby preventing airway obstruction.
Orthognathic surgery stands out as a highly effective treatment for ameliorating obstructive sleep apnea, particularly in moderate to severe cases, boasting over 90% efficacy according to literature3. Even patients with mild symptoms (AHI: 5-15) have shown improvement post-surgery, as per literature4 and my personal clinical experiences. The procedure entails cutting and repositioning the upper and lower jaw bones to enlarge the respiratory passage in the oropharynx.
However, historical instances of excessive advancement of both jaws have led to a protruded facial appearance, reminiscent of an 'ape' face. Addressing aesthetic concerns, orthognathic surgery may involve tooth extraction and segmented osteotomy of the upper jaw to achieve facial harmony.
Addressing aesthetic concerns in OSA
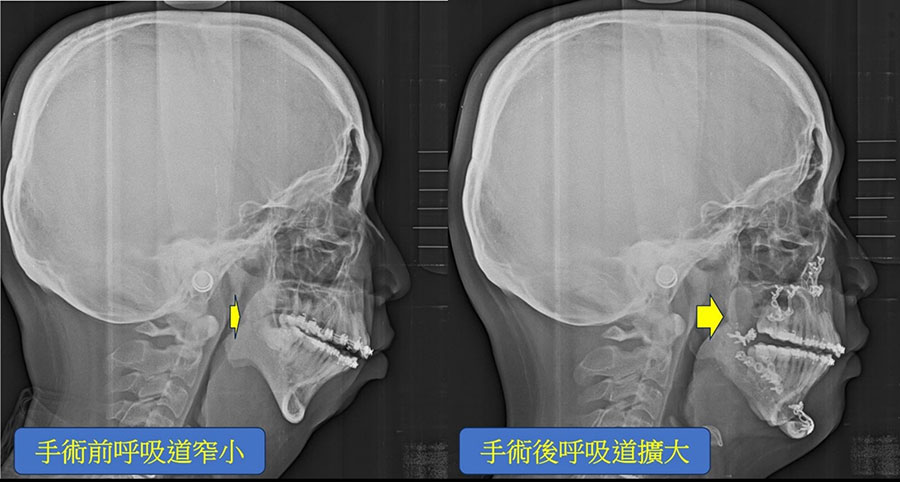
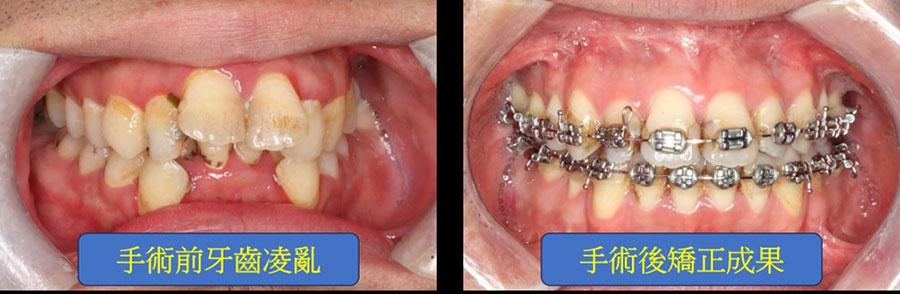
Illustratively, consider the case of Peter (Fig. 1a), afflicted with severe obstructive sleep apnea (AHI: 143; categorized as severe if above 30), possessing a short chin and a protruding upper jaw. Peter underwent tooth extraction and segmented osteotomy of the upper jaw, coupled with advancement and rotation of the lower jaw during surgery (Fig. 1b). This substantially augmented the volume of the oropharyngeal airway, alleviating airway obstruction (post-surgery AHI: 11). Additionally, the chin reshaping resulted in a more aesthetically pleasing facial appearance, bolstering Peter's self-assurance. Post-operative orthodontic treatment enhanced dental alignment, function, and esthetics (Fig. 1c).
Orthognathic surgery highly successful in severe OSA
Orthognathic surgery stands as a primary option for treating patients with moderate and severe OSA (≥ 15 events/h), boasting a commendable surgical success rate of 87.5%3. Despite the challenge of diagnosing mild OSA due to its often asymptomatic nature (referred to as 'Silent' OSA), continuous positive airway pressure (CPAP) therapy remains the gold standard treatment, albeit with low patient adherence1.
Studies have reported a high success rate of orthognathic surgery in moderate and severe OSA cases, reaching 87.5% (with AHI < 20 events/h and a reduction of at least 50% in AHI). However, focusing on cure rates (achieving a final AHI < 5 events/h), studies show rates between 40% and 50% in moderate and severe OSA patients4.
Interestingly, most patients in one study (88.9%) were unaware of having mild OSA. Skeletal profile analysis revealed that a majority of patients presented with an underlying Class II DFD (61.1%), which is a common facial pattern in OSA patients, while the remainder (38.9%) had a Class III deformity. Despite the limited sample size, evidence suggests that in patients with an underlying retrusive DFD suffering from mild OSA, orthognathic surgery may offer benefits by reducing the number of apnoea–hypopnoea events due to the achieved enlargement of the upper airway, with a mild OSA cure rate of 50%.
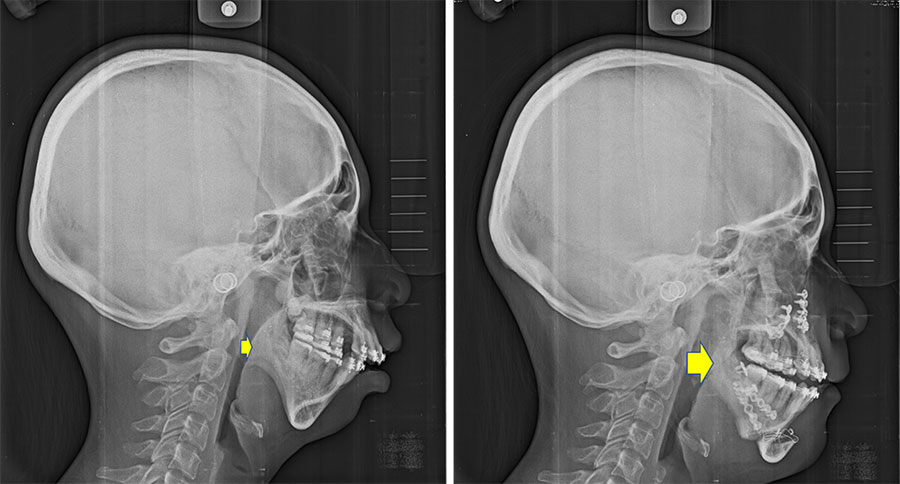
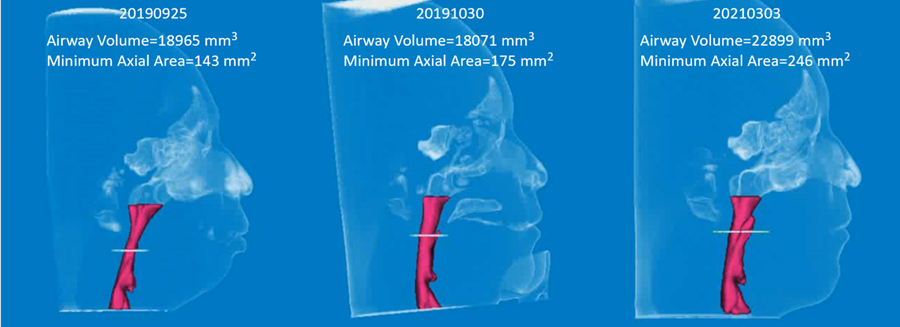
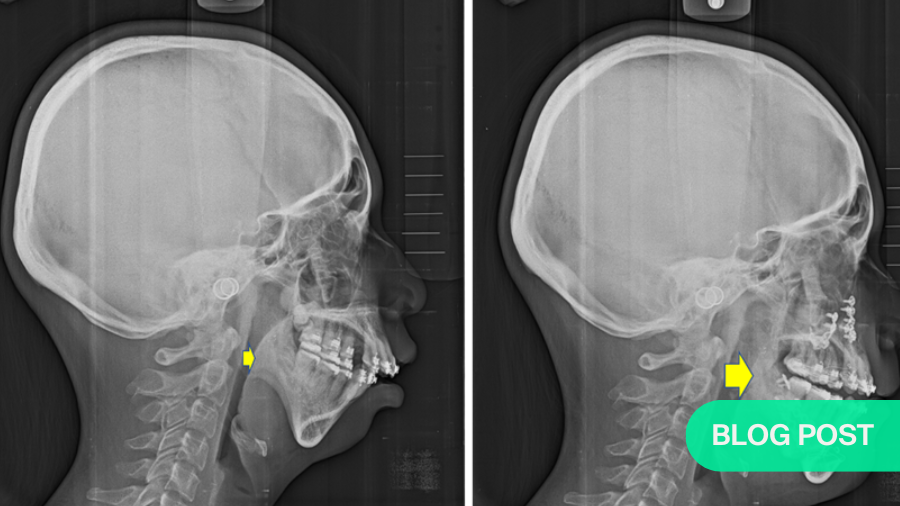
A patient with small chin complaining of sleeping disturbance with snoring, and pre-op AHI: 8.5 was noted (Fig. 2a) underwent segmental Le Lefort I osteotomy with maxilla-mandibular advancement (Fig. 2b). Post-operative airway expansion has been achieved with reduction of AHI (AHI: 2.4) after orthognathic surgery. Three-dimensional airway change shows volume of pharyngeal airway has enlarged from 18965 mm3 to 22899 mm3 peri-operatively (Fig. 2c). The patient was happy with functional and esthetical improvement during the whole treatment. Similar study of airway change could be searched in the literature which addressed patients with cleft receiving orthognathic surgery5.
As public awareness of obstructive sleep apnea grows, proper diet, weight control, and lifestyle adjustments are emphasized as prerequisites before considering surgical intervention, despite the proven efficacy of orthognathic surgery.
In conclusion, orthognathic surgery not only aids in expanding the airway but also enhances the patient's facial aesthetics. Hence, thorough discussions regarding functional and aesthetic changes post-surgery are imperative between patients and healthcare providers.
About the author:
Dr Pang-Yun Chou is Associate Professor at the Chang Gung Memorial Hospital, Taipei, Taiwan. He focuses on two-jaw orthognathic surgery, cleft lip and palate treatment, and facial trauma reconstruction. In cosmetic surgery, he practices facial bone contouring, facelift, and upper and lower blepharoplasty. Dr Pang-Yun Chou is assigned as the Director of Residency Education Program of Plastic Surgery in Chang Gung Memorial Hospital.
His research interests include newborn, school students 3dMD craniofacial images, Cleft lip and palate – alveolar bone graft, BMP-2, Orthognathic surgery – Surgery-First Approach, Simulation, Single and Double Splints, Polymers animal model – Biodegradable 3D printing plus antibiotics and analgesics, 3D printing, surgical simulation – Practice to facilitate surgical process, Artificial intelligence (AI) assisted in outcome prediction of craniofacial surgery, Multi-sensed Helmet for plagiocephaly treatment, and Anti-aging, aesthetic surgery, and cell therapy and exosome study.
References and further reading:
- Lin, C. H., Liao, Y. F., Chen, N. H., Lo, L. J., & Chen, Y. R. (2011). Three‐dimensional computed tomography in obstructive sleep apneics treated by maxillomandibular advancement. The Laryngoscope, 121(6), 1336-1347.
- Pinto, J. A., Ribeiro, D. K., da Silva Cavallini, A. F., Duarte, C., & Freitas, G. S. (2016). Comorbidities associated with obstructive sleep apnea: a retrospective study. International archives of otorhinolaryngology, 20(02), 145-150.
- Giralt-Hernando, M., Valls-Ontañón, A., Junior, O. L. H., Masià-Gridilla, J., & Hernández-Alfaro, F. (2021). What are the surgical movements in orthognathic surgery that most affect the upper airways? A three-dimensional analysis. Journal of Oral and Maxillofacial Surgery, 79(2), 450-462.
- Valls-Ontañón, A., Giralt-Hernando, M., Zamora-Almeida, G., Anitua, E., Mazarro-Campos, A., & Hernández-Alfaro, F. (2023). Does orthognathic surgery have an incidentally beneficial effect on mild or asymptomatic sleep apnoea? International Journal of Oral and Maxillofacial Surgery, 52(12), 1255-1261.
- Chen, P. R., Kwon, S. H., Lo, L. J., & Chou, P. Y. (2023). Three-dimensional comparative changes in the pharyngeal airway of patients with cleft after two-jaw orthognathic surgery. Plastic and Reconstructive Surgery, 10-1097.
You might also be interested in:
Further resources on orthognathic surgery
Explore AO CMF’s resources on craniomaxillofacial orthognathic surgery.
Craniomaxillofacial Trauma & Reconstruction (CMTR)
The official scientific publication of AO CMF, peer-reviewed and devoted to the study and treatment of craniomaxillofacial conditions.
Tackling obstructive sleep apnea
AO CMF faculty members go in-depth to address a condition that affects 1 billion worldwide.