AO CMF Incubator study reveals improved nasal positioning with minimally invasive orthognathic surgery technique
BY DR EUGÊNIA FIGUEIREDO
Disclaimer: The article represents the opinion of individual authors exclusively and not necessarily the opinion of AO or its clinical specialties.
I have always been motivated by the impact that orthognathic surgery can make not only in correcting discrepancies and improving function, but also in preventing the recurrence of deformity and delivering an improved aesthetic overall. In my master’s degree, I studied the improvement in breathing and the occurrence of empty nose syndrome achieved by performing orthognathic surgery with maxillary impaction associated with total turbinectomy. Over the past two years I have spent time developing a minimally invasive technique that I have adopted for my own patients.
It was during a women’s meeting at the Brazilian Congress of Surgery that I first realized the opportunity to study the efficacy of these techniques, with the support of the AO CMF Incubator. I was interested in developing my studies in this area in which I have always been passionate, and I saw the Incubator as an excellent opportunity to provide me with the necessary supplies and network to undertake further research.
Multicenter study explores alternative approaches to orthognathic surgery
As principal investigator, I was able to choose my team to work on this research project. We are a group of surgeons from different regions, each with our own experiences but with a shared determination and dedication to develop this work in favor of excellence. The study was conducted in the extreme regions of Brazil (Northeast and South), since the similar way of working is quite interesting. The collaboration allowed us to explore the best techniques for performing orthognathic surgery, examining the benefits and limitations, and undertaking our work a committed and ethical approach.
The research sample included 10 participants, five of whom were treated at the Oral and Maxillofacial Surgery and Traumatology outpatient clinic of private hospitals in Recife-PE, and the other five in Curitiba-PR. I performed the surgeries at Hospital Unimed, Recife, with Dr Gleisse Wantowski from Curitiba. We were also joined by Dr Tayna Carvalho from São Paulo, Dr Sarah Ballarin from Belo Horizonte, and Dr Esthefany Batista at Curitiba.
The surgeries were performed by two calibrated surgeons, with all research participants undergoing minimally invasive orthognathic surgery under general anesthesia with nasotracheal intubation. The technique used was modified Le Fort I Subspinal Osteotomy associated with minimally invasive orthognathic surgery.
Modified Le Fort I incorporating minimally invasive techniques
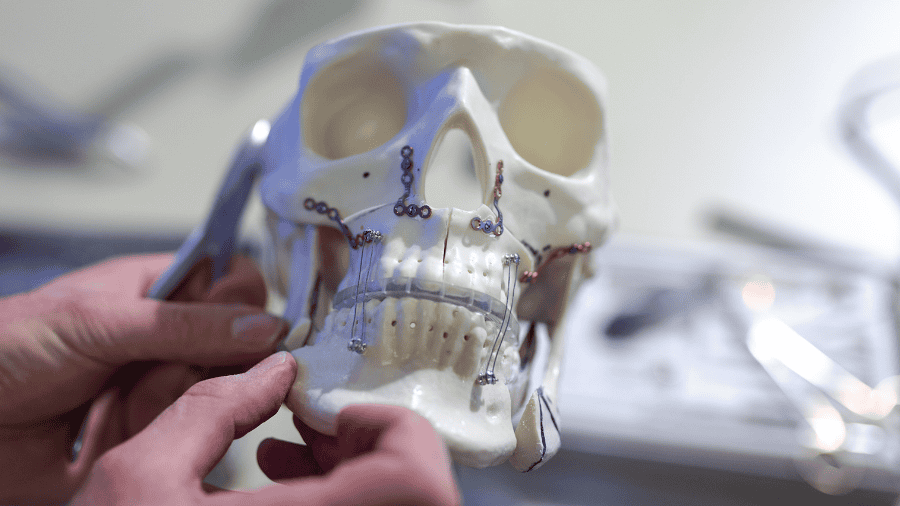
The surgeries analyzed as part of our study began with an incision in the maxillary mucosa, which was made buccal from the lateral incisor to the contralateral lateral incisor. The maxillar bone was exposed, allowing for the identification of the zygomatic, nasal and intraorbital nerve buttresses. Detachment is achieved by tunneling in the anteroposterior direction to the region of the pyterygoid process. In order to preserve the periosteal and muscular insertions, nasal detachment is kept to a minimum. We then performed a subspinal osteotomy using a reciprocating saw at the base of the anterior nasal spine in a V shape, with the nasal septum remaining attached to retain the origins of the nasolabial muscle.
The repositioning of the nasal spine must be passive between the bone stumps, and a suture with Prolene 2.0 thread was performed to fix the spine—a procedure calculated in advance of the surgery with the assistance of virtual planning. After repositioning the maxilla, we performed osteosynthesis with rigid internal fixation using four 1.5mm system plates.
Sutures were placed on the alar base muscles. The suture of the nasal sphincter was performed with the 3.0 vicryl thread by plication of the right nasal muscle and the tissues at the base of the nose, transfixing the muscle of the contralateral cut into the remaining attached gingiva at the level of the lateral incisor, crossing the midline and inserting to the sectioned muscle on the other side, the left nasal muscle and tissues at the base of the nose. The interwing brace was tightened symmetrically in direct view, with the muscles and mucosa closed in layers with Monocryl 4.0 suture.
Addressing facial deformity and delivering improved aesthetics
For my professional practice, the biggest challenge I faced lay in changing the Le Fort I osteotomy technique that I had been using for years on my patients and was already quite accustomed with. However, I had no difficulty in performing the MI technique, having had considerable recent experience in this area, and I combined this with the best benefit of the surgery for my patients. I did experience some complications, including two cases of necrosis of the upper central incisor, not because the apex of the root was amputated, but probably because the osteotomy passed too close to the root, breaking the vascular-nerve bundle.
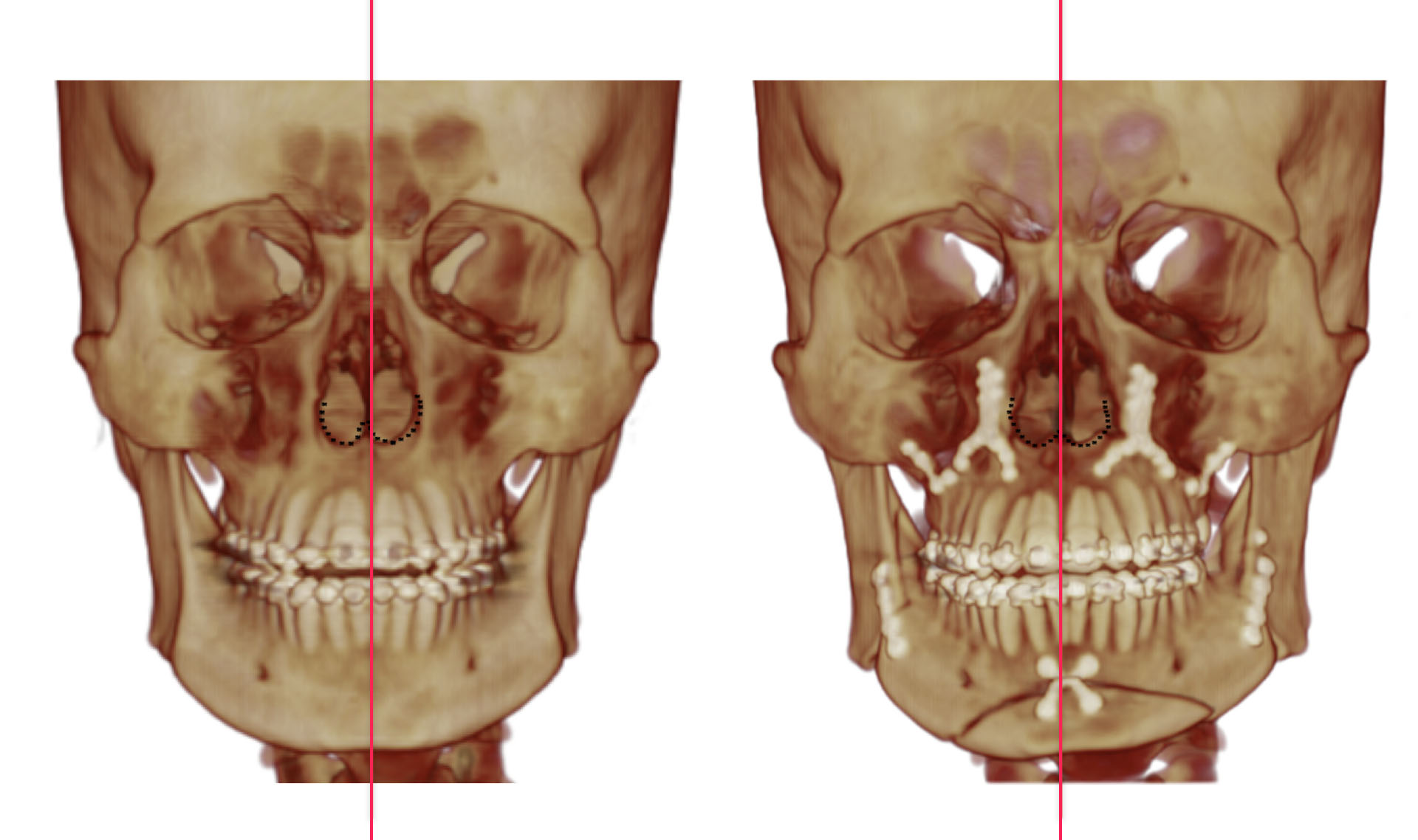
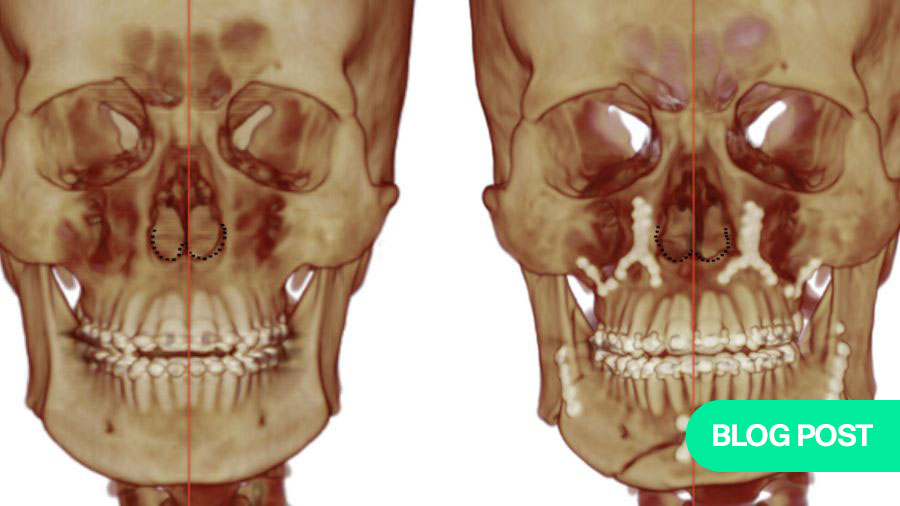
Through orthognathic surgery, we have the opportunity to considerably enhance the quality of life of our patients, addressing respiratory difficulties as well as the possibility of the occurrence of sinusitis that coexists with facial deformity. However, existing techniques carry the risk that along with the movement of bone segments, there is also movement of adjacent soft tissues, which may change the morphology, especially in the nasal region. Our study discusses the effects of the Le Fort I osteotomy on facial morphology, finding that changes in the nose region related to the new surgical position of the maxilla do not necessarily depend on the amount of advancement and/or impaction. The change can be substantiated due to the movement of the maxilla that places the anterior nasal spine in a new position.
The subspinal osteotomy technique allowed us to preserve or reposition the insertions of the paranasal musculature and the pre-existing position of the anterior nasal spine and septum as planned. Our findings revealed that this variation of the subspinal osteotomy technique allowed for better surgical management of the soft tissues of the paranasal region, in order to prevent anatomical and functional changes in the nasolabial region and to improve the aesthetic results of the anterior repositioning of the nasal spine.
Incubator opportunity allowed for professional and personal growth
Taking into account that nasal alteration has great aesthetic relevance for the patient and is directly associated with their self-esteem, the improved results delivered by minimally invasive techniques can have a considerable impact on the patient’s quality of life.
I now hope to continue working with clinical and surgical research, and supporting surgeons who have the same desire. This study has been an incredible and very important experience in my professional career. I have particularly benefited from the exchange of experiences with surgeons from all over the world, and the excellent mentorship from AO CMF faculty—including Dr Renata Pittella, Dr Otacílio Chagas, Dr Belinda Beltran, and Dr Ana Catalina Tobon—who provided invaluable feedback and high-level scientific discussion as the study progressed.
I am grateful for the opportunity provided by the Incubator, which has supported me to evolve daily not only as a surgeon, but as a person. I would encourage others to stay tuned for further Incubator opportunities via the AO Foundation website.
About the author:
You might also be interested in:
Further resources on orthognathic surgery
Explore AO CMF’s resources on craniomaxillofacial orthognathic surgery.
AO CMF research opportunities
Access to experimental and clinical research for craniomaxillofacial clinical care
Global Oral Cancer Diploma
A standardized evidence-based knowledge platform for treatment and management of oral cancer
AO CMF Guest Blog collection
Inspiring stories from practitioners and researchers in the CMF specialty