Oral cancer—flap use can restore functional, aesthetic, and quality-of-life after major oral resection
BY DR JUAN JOSÉ LARRAÑAGA AND DR MARCELO FIGARI
The preferred treatment for most cancers involves resection of the affected tissue. For patients with cancers of the head and neck, the loss of that tissue can impair functions as vital as breathing, eating, and speaking. Fortunately, reconstructive techniques can restore much of their original functionality. One of the most striking reconstructive developments is the replacement of many prostheses with pedicle-containing autologous tissues, i.e., flaps. This article will focus on the main types of flaps in use for face, mouth, and neck reconstruction.
In February of 1917, Sigmund Freud wrote in his journal that a painful growth was forming on his soft palate. While he suspected that it was malignant, he did not seek medical advice about it until 1923. He was eventually diagnosed with and treated for squamous cell carcinoma. The cancer also invaded his jaw and recurred numerous times: by the time of his death in 1939, Freud had endured more than 30 surgical procedures, and had prostheses to replace part of his jaw and several missing teeth, as well as to separate his oral cavity from his nasal cavity and maxillary sinus.
Despite his diagnosis and the persistence of his cancer, Freud lived another sixteen years, publishing articles until shortly before his death. While his surgeons could neither cure his cancer nor provide him with comfortable prostheses, they did manage to fulfil most of today’s functional criteria for successful surgery. The tumor never blocked his airway or damaged his noble structures, e.g., the carotid artery or major facial nerves; he remained able to chew, swallow and speak; he did not suffer from oral incontinence (i.e., drooling); and most external signs of his surgeries were concealed by his beard.
As photographs show, the overall aesthetic affect was very good. Unfortunately, until his death, Freud also endured enormous pain and discomfort.
In the century since Freud’s first surgery, the level of progress in oncology defies imagination. Concurrent advances in technology and diagnostic techniques mean cases can often be identified and corrected very early, leading to constantly improving prognoses.
Life extending surgery may impair major functions
The basic treatment for most cancer still involves resection of the affected tissue. For patients with cancers of the head and neck, the loss of that tissue can impair functions as basic as breathing, eating, and speaking. Fortunately, even in cases where a patient’s life expectancy is severely limited, reconstructive techniques can restore much of their original functionality. I.e., while the resection of cancerous tissue may disfigure patients and impair certain functions to extend their lives, reconstructive procedures can enable them to live more comfortably among their families and communities.
One of the most striking reconstructive developments—and one that would certainly have benefitted Freud—is the replacement of many prostheses with pedicle-containing autologous tissues, i.e., flaps. Bone, muscle, skin, and other soft tissues—whether loco-regional or free/distant—have replaced much custom-built oral cavity/maxillofacial infrastructure. This article will focus on the main types of flaps in use for face, mouth and neck reconstruction.
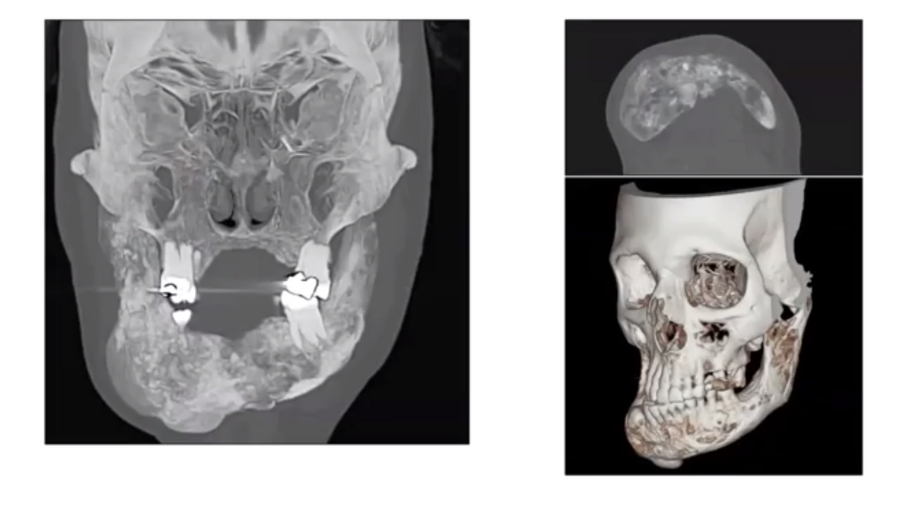
Pre-reconstruction planning: patient and defect evaluations
As the specific details of flap use depend on both the patient and the defect, it is essential to evaluate both carefully. A patient evaluation includes general status, including age and any comorbidities, their oncologic prognosis (including life expectancy), their aesthetic expectations (which may require some management), and the degree of support available to them if discharged to home.
Defect evaluation begins with the location. After the resection of the necessary tissues, will all wounds be hidden inside the mouth? Which type of tissue (muscle, bone, skin) will need to be replaced? Will it be necessary to wait for any infections to clear before proceeding with surgery? Is it possible to estimate a healing time? And, following radiotherapy, will the surrounding tissue be adequate to support a flap or other corrective structure?
Preparing for major oral reconstruction
Once the relevant patient and defect characteristics are understood, reconstructive options can be considered. If not enough tissue will be available inside the mouth, e.g., for a local flap, where will the tissue come from? Does the prospective donor site include a good-quality pedicle? If not, how will blood reach the flap? And especially, as a surgeon, do you and your team have the expertise to perform this procedure?
-
Defect site-specific considerations
Certain considerations are specific to the defect site. If it affects the floor of the mouth, any cavities or fistulae will require watertight seals. Flaps used for these purposes should be small and pliable; overly thick or large pieces should be avoided, as they typically cause constant drooling. Any deep recesses must be avoided or corrected, as food will accumulate in them. And, as much as possible, tongue mobility must be preserved.
- Tongue and retromolar trigone reconstruction
For defects in the retromolar trigone or buccal mucosa, resection of the coronoid process is often indicated (for access and to prevent trismus); and if the carotid artery will be exposed, a donor site should be chosen that includes a protective muscle flap. In cases where up to one-third of the tongue will be excised, either direct closure or a local flaps are usually sufficient. Where a slightly larger reconstruction—up to one-half of the tongue—is necessary, a pedicle-containing patch from the radial forearm is recommended (more on this below). For more than half of the tongue, although the surgeon must be careful to avoid excessive bulkiness, an anterolateral thigh (ALT) flap is normally a good choice.
- Pharyngeal reconstruction
For a patient with a pharyngeal circular or subtotal defect, plans will be necessary to restore swallowing function. Steps can also be taken for speech rehabilitation. Among the flaps available for pharyngeal reconstruction, one recommended donor site is the jejunum. As flaps of jejunum tissue alone have a high fistula rate, they can be paired with muscle to prevent this complication.
As an alternative, fasciocutaneous flaps can be used, as the ALT flap. As these do not depend on enteral surgery, they require a shorter hospital stay, but are much bulkier and more prone to stricture, which can impede normal pharyngeal function.
- The base of the tongue, swallowing mechanism
For the base of the tongue, major considerations include restoring the swallowing mechanism, preserving the tongue’s mobility, and resuspending the larynx to avoid aspiration. As flaps in this area must replace some of the volume of the resected defect, fasciocutaneous flaps are best.
- Skin grafts
In a very limited range of cases, skin grafts—as opposed to flaps, which include other vital tissue—are the best option available. Where they will be in visible locations, nearby donor sites are generally preferable, as their colour and texture match the surrounding tissue quite closely. Grafts are simple, fast, safe and thin, but have high rates of partial or total failure. Further, their thinness results from soft tissue deficits. Consequently, they may not match the volume of the tissue they replace, are prone to scar contracture, and depend on a vital tissue bed in the graft site to survive. Aesthetically, any gains to the graft site involve similar losses to the donor site.
- Problems with local flaps
Where more substantial local flaps are used, random circulation with the sub-dermal plexus can be a problem. Also, their transfer capacity tends to be low; and, as with skin grafts, soft tissue deficits are common.
In cases where complications make free flaps unfeasible, e.g., nose reconstructions, local nasolabial flaps can be used. While these are limited to quite small defects, excellent results are possible.
- Regional flaps for larger tissue volumes
Where larger volumes of tissue are necessary, regional flaps, e.g., from the scapula or ribs, may be adequate. While these are often bulky, have a limited arc of rotation, and provide poor aesthetic results, they are plentiful, safe, fast, and moderately well-vascularized.
- For very weak patients, operative time must be minimized
For a patient with a large defect, combined with a very poor prognosis (limiting the time available for surgery), the use of a pectoralis major, dorsalis, or trapezius muscle flap will save precious time and produce acceptable results. And, as noted, muscle flaps greatly reduce the probability that fistulae will form.
- Microvascular free flaps versus other flaps
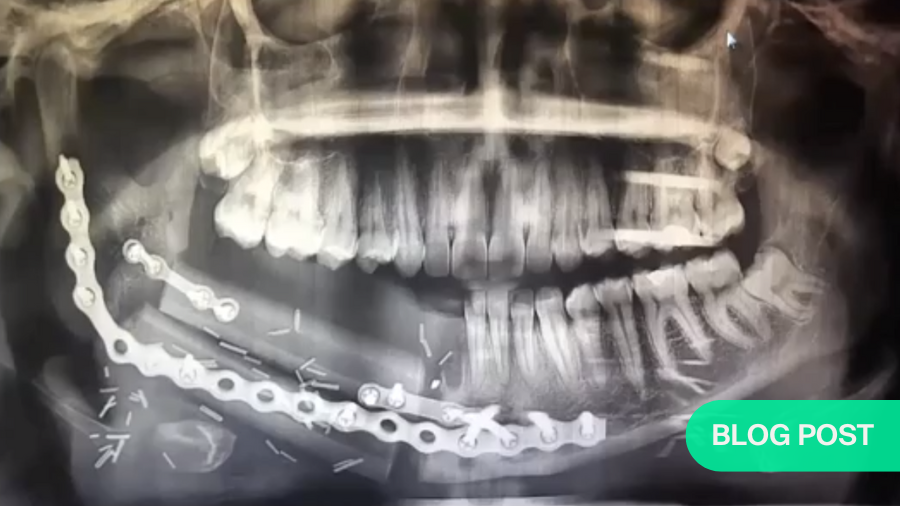
Overall, where microvascular/microsurgical free flaps are an option, they are the gold standard for head and neck reconstruction. They offer the best bone, along with the best possibilities for adaptation to the region, paired with excellent recovery. With few exceptions, where tissue transfer is necessary for reconstruction, they should be the primary option.
For example, free flaps are normally indicated for circumferential pharyngoesophageal reconstruction, class III or higher defects of the maxilla, and composite defects in mandibular reconstruction. When used for salvage total laryngectomy, they reduce the incidence of pharyngocutaneous fistulae.
Other advantages of microvascular free flaps include the wealth of tissue available to produce them, their distribution of free tissue, their well-vascularized soft tissue and bone, their flexibility regarding donor sites, and the possibility to produce chimeric structures, i.e., combinations of tissue from different sources (e.g., muscle and jejunum tissue) linked via a common blood vessel.
Their direct disadvantages include the risk of total necrosis (<6% of cases) and longer operating times (which are not always balanced by improved patient outcomes). They also require intensive training (for which fellowships are widely available) and have greater institutional requirements. I.e., this type of surgery is best suited to institutions that see a steady stream of cases.
Microvascular surgery is not a one-size-fits-all
From a health-economic perspective, however, microvascular surgery is not a one-size-fits-all solution. Compared to a simpler pedicled flap surgery, a 2013 Italian study found that both the cost and cost-effectiveness of microvascular free flap surgery varied between patient groups. Particularly for those with very short expected survival, the risk of longer operative time generally outweighs the advantages of the microvascular flap.
This brings us back, as promised, to the radial forearm, which is the most popular free flap donor site for head and neck reconstructions. Flaps from this area are thin and pliable, easy to harvest, and include a pedicle of up to around 20cm. Additionally, the radial artery is typically 2mm or more in diameter, ensuring a healthy blood supply. As noted, a radial forearm flap is usually an excellent choice to replace up to half of the tongue. For a lower lip reconstruction, a double skin paddle including the palmaris longus is possible from the same site.
However, if bone is required, the radius is normally a poor candidate. Removing part of it will necessitate plating, and various other sites offer far more usable bone.
Choosing a flap donor site: logistical and time-related considerations
When planning the surgery, choosing a donor site that is easily accessible without repositioning the patient—and the radial forearm is an excellent example—can considerably shorten the operative time. If it is possible to have two groups operating concurrently, this will allow a flap harvest team to work alongside the o team. Even if only a single team is available, repositioning the patient (twice) is time-consuming and should be avoided if not completely necessary.
- Adjusting for retraction where bulk is added
Particularly where a flap is used to increase bulk, some degree of retraction normally occurs. This process can continue for a very long time. Therefore, in cases where a massive resection of the tongue and mandibulotomy have been necessary, a slightly-oversized ALT flap (with bone taken from the femur, if necessary ) will allow for shrinkage over a period of ten or more years.
- Multi-phase surgical plans
Concerning the way we plan the reconstruction, for various reasons, previous generations of surgeons often divided a reconstruction into many small steps. Using current techniques, while two or more surgeries may be necessary, it is best to do as much as possible of what we know will be necessary in each episode.
Naturally, there are exceptions. For example, if we need to increase the height of mandible via distraction, but the patient is scheduled for radiation treatment, it is advisable to wait three to six months after the radiotherapy before beginning the distraction process. And the process itself will require daily adjustments.
- Ladder vs elevator planning
As for long-term planning, earlier generations of surgeons approached reconstruction like a series of rungs on a ladder, with numerous steps built into a rather long process. In addition to stretching a reconstruction out for months or years, this multiplied the patient’s chances of perioperative infection and other complications. As many patients are quite old at the time of their first surgery, many would die before their reconstructions were complete.
Today, we are more likely to use an elevator-style approach. When the patient leaves the operating room after their first surgery, their reconstruction may not always be complete, but it will be much closer to that level than previously.
Finally, to return to the case of Dr Freud, the techniques discussed here would not have saved him, but they would have allowed him far more comfort, and may very well have extended his life. Likewise, for many of our patients—some of whom have only a few months left to live—a well-executed reconstruction can return such basic capacities as the ability to chew and swallow food, to breathe naturally, and to speak understandably to the people around them. That is, flaps increase the quality of patients’ lives.
About the authors:
Dr Marcelo Figari is the Past Chair of the Head and Neck Surgery Department and also the University Rector at Hospital Italiano in Buenos Aires, Argentina. He is also a current member of the AOFB. He specializes in thyroid and parathyroid surgery, head & neck cancer surgery, head & neck reconstruction, facial trauma surgery, medical education, and surgical education.
Dr Juan José Larrañaga is the current Head of the Department of Head and Neck Surgery at the Hospital Italiano in Buenos, Aires Argentina. He is a head and neck surgeon and a plastic surgeon, and a recognized specialist in microvascular head and neck reconstruction.
References and further reading:
- Lazaridis, N, Sigmund Freud’s oral cancer. Journal of Oral and Maxillofacial Surgery (2003) 41, 78–83. Available online at www.sciencedirect.com.
- Deganello A, Gitti G, Parrinello G, Muratori E, Larotonda G, Gallo O. Cost analysis in oral cavity and oropharyngeal reconstructions with microvascular and pedicled flaps. Acta Otorhinolaryngol Ital. 2013;33(6):380-387.
This article is a summary of an AO CMF expert presentations webinar titled Reconstruction After Major Oral Cavity Resection. It focuses on the use of free flaps (microvascular and non-microvascular), including recommended donor sites, for oral cavity/pharyngeal reconstruction after oncological resection. It covers:
- conditions that influence the best reconstruction options following major oral cavity resection
- common goals of microvascular and non-microvascular techniques and when to use each, and
- clinical examples, to discuss the different indications for oral cavity reconstruction.
All AO CMF recorded webinars are available free of charge to AO CMF members.
You might also be interested in:
Global Oral Cancer Diploma
Interactive, self-directed online program for management of oral cancer cases. Global launch in 2024, 10 online modules, 10 months.
AO CMF Global Study Clubs
Monthly online events with renowned speakers, delving into a wide range of craniomaxillofacial surgical topics.
AO CMF Guest Blog
A front-seat view to the lates hot topics from AO’s global craniomaxillofacial community. Submit your own ideas.